Hypoxia, along with other pathologies of intrauterine development, poses a real danger to the health and life of an unborn child. In this article we will talk about different types of hypoxia, its causes, consequences, as well as the prevention and treatment of this pathology.
This pathology is a multi-organ syndrome that occurs due to the fact that oxygen does not reach the organs and tissues of the fetus in the required volume. The consequences are quite serious - from dysfunction of the central nervous system to the most dismal outcome. If acute fetal hypoxia is detected, immediate medical attention is required - the sooner it is provided, the lower the risk of complications.
Degrees of hypoxia: acute and chronic
Our body cannot live without oxygen, so even a short oxygen deprivation leads to serious consequences. There are two types of hypoxia – acute and chronic.
What is the difference between them? A simple example: if a piece of food is blocked in the respiratory tract, this causes acute hypoxia. And if you live for months in a stuffy, poorly ventilated room, this causes chronic oxygen starvation.
Chronic hypoxia as a result of constant stuffiness is often the cause of malaise in adults - it leads to decreased immunity, deterioration in the quality of sleep, frequent headaches, constant fatigue and weakness.
Important! During pregnancy, prolonged stay in a stuffy room is dangerous precisely because of the risk of developing intrauterine fetal hypoxia. Therefore, doctors recommend being in the fresh air as often as possible, since they assume that all the windows in the apartment are closed and there is not enough fresh air.
The fruit is 100% dependent on the environment in which it is located. Therefore, expectant mothers need to avoid stuffiness, large crowds of people and regularly ventilate the apartment where they spend a lot of time. There is a myth that the room only needs to be ventilated for 15 minutes in the morning and evening. Ventilation should be constant, but this is not always possible due to the environment - dirt, noise, drafts, allergies.
Acute fetal hypoxia during pregnancy is the nightmare of any obstetrician. It can develop due to pathologies of intrauterine development (for example, placental abruption), or during childbirth - due to abnormalities in the birth act.
Consequences and prognosis
Mild and moderate hypoxia with timely and high-quality treatment does not lead to serious consequences, but severe hypoxia is dangerous due to the development of the following conditions:
- anxiety, restlessness of the child and mental lability;
- retardation in physical and mental development, headaches and development of neurocirculatory dystonia;
- increased intracranial pressure;
- development of epileptic syndrome and hydrocephalus;
- formation of brain cysts;
- damage to the cranial nerves and loss of their functions.
Rare consequences of severe hypoxia in a newborn include disability of the child or death.
The prognosis depends on the degree of hypoxia. With mild and moderate hypoxia and adequate therapy, the prognosis is favorable; with severe brain hypoxia, the prognosis is questionable.
Consequences: why is this intrauterine syndrome dangerous?
Until the moment the child is born, he does not have independent breathing. He breathes liquid with oxygen dissolved in it, which entered it through the placenta from the mother’s blood. Simply put, the child breathes the air that his mother breathes, and if there are problems with O2 delivery at any stage, a threat of fetal hypoxia is created.
When oxygen deficiency occurs, the child’s body begins to redistribute it so that first O2 enters vital organs (brain, heart and adrenal glands), and only then goes to the skin, kidneys, gastrointestinal tract and lungs. Because of this, the first violations affect the development of those organs and systems that, during hypoxia, received oxygen according to the “residual principle.”
Problems with chronic hypoxia:
- difficulty in adapting to stimuli in a newborn (convulsions, problems with appetite and breathing);
- risk of developing epilepsy;
- cardiovascular disorders;
- risk of kidney failure;
- enterocolitis, frequent regurgitation;
- secondary immunodeficiency;
What could be the consequences for a child in the future due to acute hypoxia? In this case, the central nervous system is primarily affected. Acute oxygen deficiency in the fetus can cause the following disorders:
- mental retardation;
- DIC syndrome;
- neurological disorders;
- cerebral edema;
- pulmonary hypertension;
- necrosis and ischemia of various organs.
Treatment for fetal hypoxia
If oxygen starvation of the pregnant child is detected, the pregnant woman is placed in an obstetrics and gynecology hospital. In case of fetal hypoxia, the existing obstetric and extragenital pathology in the woman is corrected, and measures are taken to normalize fetoplacental blood circulation.
The pregnant woman is recommended to undergo strict bed rest, oxygen therapy, and treatment to normalize uterine tone and reduce intravascular coagulation.
The only treatment with proven effectiveness is controlled hypothermia.
.
Complications of fetal hypoxia include:
- cerebral edema, perinatal encephalopathy, convulsions, areflexia;
- posthypoxic pneumopathy, pulmonary hypertension;
- ischemic necrosis of the endocardium, heart and vascular defects;
- renal failure, oliguria;
- regurgitation, vomiting, enterocolitis;
- DIC syndrome;
- secondary immunodeficiency;
- asphyxia of newborns (75–80%).
Main causes of hypoxia
There are four main causes of oxygen deficiency in the fetus: pathologies during pregnancy (for example, a conflict of Rh factors), illnesses of the mother, her bad habits and harmful environmental influences.
Pathologies during pregnancy . Hypoxia can be caused by postmaturity, entanglement with the umbilical cord, Rh conflict between the blood of mother and child, disturbances in the development of the umbilical cord and placenta, as well as pathologies of the fetus itself:
- intrauterine trauma;
- genetic abnormalities;
- developmental defects;
- hemolytic disease.
Mom's illnesses. The range of pathologies is very wide. One of the most common causes of hypoxia in this case is iron deficiency anemia.
Oxygen deficiency in the fetus can also result from:
- pyelonephritis;
- diabetes;
- diseases of the urinary and respiratory system;
- arterial hypertension;
- endocrine diseases;
- kidney diseases;
- diseases of the immune system.
Separately, it is worth mentioning the consequences of STIs (herpes, chlamydia, gonorrhea, mycoplasmosis, bacterial vaginosis, candidiasis and trichomoniasis), malnutrition, exhaustion and severe toxicosis in the mother.
Drinking alcohol and smoking. Why does the mother’s bad habits often result in fetal hypoxia? It’s all about the effect that the listed substances have on the inner surface of the alveoli of the lungs.
The alveoli have a special lubricant that ensures rapid delivery of oxygen to the blood. Alcohol vapor dilutes this lubricant, causing it to perform its function worse. This is just one of many other harmful effects of drinking alcohol during pregnancy.
Smoking also provokes the development of fetal hypoxia: the tars in tobacco smoke “clog” the alveoli, due to which lubrication is not produced in the required quantity. Smoking contributes to chronic hypoxia - both for the mother and the unborn child.
Environmental factors . Living in an ecologically unfavorable area, working in a hazardous industry, or in the presence of toxic substances in the air can also cause fetal hypoxia. A similar effect is caused by constant stay in rooms with poor ventilation, when the air contains too much carbon dioxide and too little oxygen.
Therapeutic tactics of hypoxia
If fetal hypoxia occurs during the period of pushing or during contractions (decrease in heartbeat), a decision is made to complete the labor as soon as possible: a cesarean section or the application of obstetric forceps (in the case of labor stimulation with oxytocin, the administration of the drug is stopped). After the birth of the child, immediate medical care begins:
- clearing the respiratory tract from mucus, meconium and water (suction with a special aspirator);
- supplying a mixture of oxygen with air or pure humidified oxygen through a mask, nasal catheter or mechanical ventilation device (in case of severe hypoxia, the newborn is placed in an incubator, intubated and mechanical ventilation is started);
- heating the baby with radiant heat (on a special changing table), and in case of severe hypoxia, placing the baby in an incubator;
- administration of drugs that stimulate blood circulation and increase blood pressure (camphor, dopamine) and drugs that stimulate the respiratory center (etimizole);
- intravenous infusions solution, sodium bicarbonate (neutralization of carbon dioxide in the blood), glucose to restore the reduced volume of the vascular bed;
- transfusion of blood products if necessary (hemolytic disease of the newborn);
- prescribing antibiotics to prevent pulmonary infections in case of severe hypoxia or intrauterine infection of the fetus, as well as in respiratory distress syndrome during premature birth;
- prescription of anticonvulsants (phenobarbital, phenazepam);
- To reduce intracranial pressure, administration of diacarb and veroshpiron (diuretics with the effect of reducing cerebrospinal fluid production) is indicated.
How to identify hypoxia: symptoms and diagnosis
The modern level of medicine makes it possible to detect the presence of hypoxia “without delay”, at its earliest stage. There are a number of diagnostic methods for this:
- analysis of the biochemical composition of blood and hormones;
- listening to heart sounds with a stethoscope (detection of bradycardia and tachycardia);
- amnioscopy - analysis of amniotic fluid (a sign of hypoxia - the presence of meconium in its composition);
- ultrasonography;
- cardiotocography;
- ECG;
- Dopplerometry (study of the circulatory system, analysis of blood circulation in all its areas).
What should you pay attention to? Very strong, sharp kicks of the child that cause pain in the mother are an alarming sign. They may be a consequence of the development of hypoxia: these are reflex movements when the child experiences a lack of oxygen and wants to increase the incoming blood flow. The next symptom is the weakening and complete disappearance of tremors.
Important! The child’s activity norm is at least ten movements in 12 hours.
At what point should fetal activity be monitored? Doctors recommend monitoring your sensations, frequency and strength of kicks, starting from the 28th week of pregnancy. However, the risk of developing hypoxia exists from the first weeks, when it is impossible to monitor fetal activity.
If there are risk factors, then obstetrician-gynecologists recommend a set of measures to prevent oxygen deficiency. In addition, the mother needs to eat in a timely and nutritious manner, avoid lack of sleep and overwork, spend more time outdoors, and ensure regular ventilation in the room.
Assessment of the baby's condition using the Apgar scale . At birth, obstetricians evaluate the baby's condition using Apgar scores (named after the author of this technique, Virginia Apgar). This method analyzes five criteria - breathing, skin color, muscle tone, and heart rate. The child's condition is assessed twice - immediately after passing through the birth canal, and five minutes after that.
- Norm (from 8 to 10 points);
- The condition requires control (from 4 to 7 points). Moderate hypoxia is possible, compensation may be required, prognosis is favorable;
- Asphyxia ( from 0 to 3 points). Severe hypoxia, in which the child requires immediate resuscitation measures.
Low scores on this scale are not always given due to hypoxia, but in most cases it is oxygen deficiency that causes the difficult condition of the newborn.
Hypoxia of the fetus and newborns
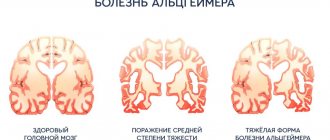
Intrauterine hypoxia can be caused by various reasons: infectious, cardiovascular, hematological and pulmonary diseases of the mother, toxicosis of pregnancy, maternal isoimmunization due to Rhesus and ABO incompatibility of the blood of the mother and fetus, intoxication. Obstetric pathology leading to disruption of the uteroplacental circulation is also important. Hypoxia occurs in 4–6% of newborns and is one of the most common causes of stillbirth and neonatal death. Children who have suffered hypoxia often experience persistent psychiatric and neurological disorders. Clinical manifestations of hypoxia depend on the severity and duration of the latter.
1) With hypoxia of mild severity (“blue asphyxia”), the condition of the newborn can be severe only in the first hours of life after birth. In this case, breathing is rapid, the skin is cyanotic (Greek kyanos - azure), muscle tone is normal or slightly changed, unconditioned reflexes are preserved. The newborn's condition quickly improves and becomes satisfactory on the 3rd–4th day. Subsequently, serious psychiatric and neurological pathology is usually not detected.
2) With moderate hypoxia, the newborn’s breathing is shallow, irregular, heart sounds are muffled, the reaction to external stimuli is significantly reduced, the cry is quiet and painful. Muscle tone may be altered (increased or decreased), unconditioned reflexes are depressed or quickly depleted. Sometimes convulsive twitching of the facial muscles is observed. The skin and mucous membranes are bluish or pale. The child's condition improves slowly over 1–2 weeks. Subsequently, residual neurological symptoms and signs of mental retardation may be identified.
3) Severe hypoxia is characterized by significant disturbances in breathing and circulation. The skin is pale and has an earthy tint (“white asphyxia”), the mucous membranes are cyanotic, heart sounds are muffled, and the pulse is arrhythmic. Muscle tone is reduced, unconditioned reflexes are suppressed, and signs of damage to the cranial nerves are revealed. The eyeballs "float". After birth, children do not cry, and later do not suck or swallow on their own. They are lethargic and inactive, but sometimes they suddenly become very agitated. Sleep is disrupted - children sleep very little. The palpebral fissures are wide open, the gaze is fixed at one point. Hyperkinesis is observed, often tremor, and tonic-clonic convulsions often occur. The umbilical cord is collapsed and does not pulsate. Subsequently, significant mental development disorders and residual neurological symptoms are revealed.
It should be borne in mind that asphyxia during childbirth is often a continuation of intrauterine fetal hypoxia. In maternity hospitals, in the first minutes or hours of a child’s life after birth, they use an assessment of his condition on the Apgar scale, which takes into account five indicators: heartbeat, breathing, muscle tone, skin color, reflexes. Each indicator is assessed in points (the norm is 2 points). With a sum of indicators equal to 8–10 points, the condition of the newborn is considered good, with an indicator of 6–7 points – satisfactory, 5 points or less – severe.
Treatment of hypoxia in newborns comes down, firstly, to the rapid elimination of oxygen starvation (Persianinov method, artificial respiration, other methods of oxygen therapy). Secondly, drug therapy is used: dehydration and hormonal treatment (especially important to avoid cerebral edema), the prescription of cardiac medications, respiratory analeptics, vitamins, sedatives, anticonvulsants - depending on the severity of the disorders that arise.
Return to Contents
Treatment and prevention
Treatment in this case involves normalizing blood flow and a stable supply of oxygen to the blood. Doctors draw up a treatment plan based on the results of the examination and studies performed. In some cases, due to a threat to the life of the fetus, labor is induced using medications.
Hypoxia is a serious pathology, therefore only a doctor has the right to prescribe treatment. There are no ready-made, universal treatment regimens. There are only general recommendations for pregnant women - rest, bed rest, sleeping on your side.
Prevention. A woman is required, first of all, to be responsible in preparing for pregnancy - preliminary treatment of the reproductive organs, adherence to the rules of a healthy diet, complete abandonment of bad habits, and physical activity.
Frequent walks in the fresh air are an important part of prevention. It is also necessary to ensure that the ventilation in the house works properly and that effective air exchange is ensured. A practical solution would be to install compact supply ventilation with a set of filters - this way you can be sure that there will always be fresh, clean air in the house.
Condition monitoring. After conception, regular medical monitoring of the fetus's condition is necessary. Special attention should be paid to the prevention of anemia, as it is one of the common causes of hypoxia. If hypoxia has been diagnosed, the correct choice of birth method is necessary, as well as measures to prevent birth injuries.
Ventilator OXY as a means of preventing fetal hypoxia
Constant stuffiness is one of the causes of chronic hypoxia. Ventilation problems usually occur due to poorly functioning hoods and the installation of plastic windows that “seal” the room. In this case, supply ventilation will help “start” normal air exchange.
An example of such ventilation is the OXY ventilator - a compact device equipped with a fan and a set of filters. To install it, a channel is drilled in the outer wall onto which the ventilator is mounted.
The OXY ventilator is an effective means of preventing fetal hypoxia. Immediately after installation, it provides a round-the-clock supply of fresh air with the windows closed. With it, the expectant mother will not be disturbed by street noise, dirt and drafts. Thanks to the optimal oxygen content in the atmosphere of the room, you will be provided with complete, healthy sleep and rest, good health and mood.