Transfusion shock is the most dangerous complication of transfusion of blood and its components. Since this procedure is a selective medical one, the main reason is errors in determining blood groups, Rh factor, and conducting compatibility tests.
According to statistics, they account for up to 60% of cases. Blood transfusions are carried out only in hospital settings. Doctors are trained in this technique. In large hospitals, a transfusiologist has been introduced who monitors transfusion cases, monitors the correct execution, ordering and receipt of prepared donor blood and its components from the “Blood Transfusion Station”.
What changes in the body occur during transfusion shock?
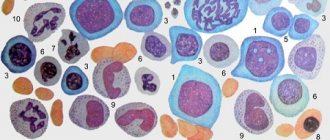
When blood incompatible with the ABO system enters the recipient's blood, the destruction of donor red blood cells (hemolysis) begins inside the blood vessels. This causes the release and accumulation in the body of:
- free hemoglobin;
- active thromboplastin;
- adesine diphosphoric acid;
- potassium;
- erythrocyte coagulation factors;
- biologically active substances, clotting activators.
This reaction is classified as cytotoxic, a type of allergic reaction.
As a result, several pathogenetic mechanisms of the blood transfusion shock state are launched at once:
- altered hemoglobin loses connection with oxygen molecules, which leads to tissue hypoxia (oxygen deficiency);
- the vessels first spasm, then paresis and expansion occur, microcirculation is disrupted;
- increased permeability of vascular walls promotes the release of fluid, and blood viscosity increases;
- increased coagulation causes the development of disseminated intravascular coagulation (DIC syndrome);
- due to an increase in the content of acidic residues, metabolic acidosis occurs;
- hydrochloric acid hematin accumulates in the renal tubules (the result of the breakdown of hemoglobin), in combination with spasm and impaired patency of the vascular glomeruli, this contributes to the development of acute renal failure, the filtration process gradually stops, and the concentration of nitrogenous substances and creatinine in the blood increases.
Impaired microcirculation and hypoxia lead to changes in internal organs, primarily in brain cells, lung tissue, liver, and endocrine glands. Hemodynamic parameters drop sharply.
Shock. Etiology. Pathogenesis. Classification
The term "shock", meaning a blow, shock, shock in English and French, was accidentally introduced in 1743 by a now unknown translator into English of a book by Louis XV's army consultant Le Dran to describe the condition of patients after a gunshot injury. Until now, this term has been widely used to describe the emotional state of a person when exposed to unexpected, extremely strong mental factors, without implying specific damage to organs or physiological disorders. In clinical medicine, shock means a critical condition, which is characterized by a sharp decrease in organ perfusion, hypoxia and metabolic disorders. This syndrome is manifested by arterial hypotension, acidosis and rapidly progressive deterioration in the functions of vital body systems. Without adequate treatment, shock quickly leads to death.
Acute short-term hemodynamic disturbances can be a transient episode when there is a violation of vascular tone, reflexively caused by sudden pain, fear, the sight of blood, stuffiness or overheating, as well as cardiac arrhythmia or orthostatic hypotension due to anemia or hypotension. This episode is called collapse and in most cases resolves on its own without treatment. Due to a transient decrease in blood supply to the brain, syncope - a short-term loss of consciousness, which is often preceded by neuro-vegetative symptoms: muscle weakness, sweating, dizziness, nausea, darkening of the eyes and tinnitus. Characterized by pallor, low blood pressure, bradycardia or tachycardia. The same thing can develop in healthy people at high ambient temperatures, since heat stress leads to a significant dilation of skin vessels and a decrease in diastolic blood pressure. Longer hemodynamic disorders always pose a danger to the body.
Causes of shock
Shock occurs when the body is exposed to super-strong irritants and can develop as a result of various diseases, injuries and pathological conditions. Depending on the cause, hemorrhagic, traumatic, burn, cardiogenic, septic, anaphylactic, blood transfusion, neurogenic and other types of shock are distinguished. There may also be mixed forms of shock caused by a combination of several reasons. Taking into account the pathogenesis of changes occurring in the body and requiring certain specific therapeutic measures, four main types of shock are distinguished
Hypovolemic shock occurs with a significant decrease in blood volume as a result of massive bleeding or dehydration and is manifested by a sharp decrease in venous return of blood to the heart and severe peripheral vasoconstriction.
Cardiogenic shock occurs when there is a sharp decrease in cardiac output due to impaired myocardial contractility or acute morphological changes in the heart valves and interventricular septum. It develops with normal bcc and is manifested by overflow of the venous bed and pulmonary circulation.
Redistribution shock is manifested by vasodilation, a decrease in total peripheral resistance, venous return of blood to the heart and an increase in the permeability of the capillary wall.
Extracardiac obstructive shock occurs due to the sudden occurrence of an obstruction to blood flow. Cardiac output drops sharply despite normal blood volume, myocardial contractility and vascular tone.
Pathogenesis of shock
Shock is based on generalized perfusion disturbances, leading to hypoxia of organs and tissues and disorders of cellular metabolism ( Fig. 15. 2. ). Systemic circulatory disorders are a consequence of decreased cardiac output (CO) and changes in vascular resistance.
Primary physiological disorders that reduce effective tissue perfusion are hypovolemia, heart failure, impaired vascular tone, and obstruction of large vessels. With the acute development of these conditions, a “mediator storm” develops in the body with the activation of neuro-humoral systems, the release into the systemic circulation of large quantities of hormones and pro-inflammatory cytokines, affecting vascular tone, vascular wall permeability and CO. In this case, the perfusion of organs and tissues is sharply disrupted. Acute severe hemodynamic disorders, regardless of the reasons that caused them, lead to the same type of pathological picture. Serious disturbances of central hemodynamics, capillary circulation and critical disruption of tissue perfusion with tissue hypoxia, cell damage and organ dysfunction develop.
Hemodynamic disorders
Low CO is an early feature of many types of shock, except for redistribution shock, in which in the initial stages the cardiac output may even be increased. CO depends on the strength and frequency of myocardial contractions, venous blood return (preload) and peripheral vascular resistance (afterload). The main reasons for a decrease in CO during shock are hypovolemia, deterioration in the pumping function of the heart and increased arteriolar tone. The physiological characteristics of various types of shock are presented in table. 15.2 .
In response to a decrease in blood pressure, the activation of adaptive systems increases. First, reflex activation of the sympathetic nervous system occurs, and then the synthesis of catecholamines in the adrenal glands increases. The content of norepinephrine in plasma increases 5-10 times, and the level of adrenaline increases 50-100 times. This enhances the contractile function of the myocardium, increases cardiac activity and causes a selective narrowing of the peripheral and visceral venous and arterial beds. Subsequent activation of the renin-angiotensin mechanism leads to even more pronounced vasoconstriction and the release of aldosterone, which retains salt and water. The release of antidiuretic hormone reduces urine volume and increases its concentration.
In shock, peripheral vasospasm develops unevenly and is especially pronounced in the skin, abdominal organs and kidneys, where the most pronounced decrease in blood flow occurs. Pale and cool skin observed during examination and pallor of the intestine with weakened pulse in the mesenteric vessels visible during surgery are clear signs of peripheral vasospasm.
Constriction of the blood vessels of the heart and brain occurs to a much lesser extent compared to other zones, and these organs are provided with blood longer than others due to a sharp limitation of the blood supply to other organs and tissues. The metabolic rates of the heart and brain are high, and their reserves of energy substrates are extremely low, so these organs do not tolerate prolonged ischemia. Neuroendocrine compensation of a patient in shock is primarily aimed at providing the immediate needs of vital organs - the brain and heart. Sufficient blood flow in these organs is maintained by additional autoregulatory mechanisms as long as blood pressure exceeds 70 mmHg. Art.
Centralization of blood circulation is a biologically appropriate compensatory reaction. In the initial period, it saves the patient’s life. It is important to remember that initial shock reactions are adaptation reactions of the body aimed at survival in critical conditions, but beyond a certain limit, they begin to be pathological in nature, leading to irreversible damage to tissues and organs. Centralization of blood circulation, which persists for several hours, along with protection of the brain and heart, is fraught with a mortal danger, although more distant. This danger lies in the deterioration of microcirculation, hypoxia and metabolic disorders in organs and tissues.
Correction of central hemodynamic disturbances during shock includes intensive infusion therapy aimed at increasing blood volume, the use of drugs that affect vascular tone and myocardial contractility. Only in case of cardiogenic shock is massive infusion therapy contraindicated.
Disorders of microcirculation and tissue perfusion
The microvasculature (arterioles, capillaries and venules) is the most important link in the circulatory system in the pathophysiology of shock. It is at this level that nutrients and oxygen are delivered to organs and tissues, and metabolic products are also removed.
The developing spasm of arterioles and precapillary sphincters during shock leads to a significant decrease in the number of functioning capillaries and a slowdown in the speed of blood flow in the perfused capillaries, ischemia and tissue hypoxia. Further deterioration of tissue perfusion may be associated with secondary capillary pathology. The accumulation of hydrogen ions, lactate and other products of anaerobic metabolism leads to a decrease in the tone of arterioles and precapillary sphincters and an even greater decrease in systemic blood pressure. In this case, the venules remain narrowed. Under these conditions, the capillaries become overfilled with blood, and albumin and the liquid part of the blood intensively leave the vascular bed through pores in the walls of the capillaries (“capillary leak syndrome”). Thickening of blood in the microcirculatory bed leads to an increase in blood viscosity, while the adhesion of activated leukocytes to endothelial cells increases, red blood cells and other formed elements of blood stick together and form large aggregates, peculiar plugs, which further worsen microcirculation until the development of sludge syndrome.
Vessels blocked by the accumulation of blood cells are switched off from the bloodstream. The so-called “pathological deposition” develops, which further reduces the bcc and its oxygen capacity and reduces the venous return of blood to the heart and, as a result, causes a drop in CO and a further deterioration in tissue perfusion. Acidosis, in addition, reduces the sensitivity of blood vessels to catecholamines, preventing their vasoconstrictor effect and leads to atony of the venules. Thus, a vicious circle is closed. A change in the ratio of the tone of the precapillary sphincters and venules is considered a decisive factor in the development of the irreversible phase of shock.
An inevitable consequence of slowing capillary blood flow is the development of hypercoagulation syndrome. This leads to disseminated intravascular thrombus formation, which not only increases capillary circulation disorders, but also causes the development of focal necrosis and multiple organ failure.
Ischemic damage to vital tissues consistently leads to secondary damage that maintains and aggravates the shock state. The resulting vicious circle can lead to a fatal outcome.
Clinical manifestations of impaired tissue perfusion are cold, moist, pale cyanotic or marbled skin, prolongation of capillary refill time over 2 seconds, temperature gradient over 3 °C, oliguria (urination less than 25 ml/hour). To determine the capillary refill time, squeeze the tip of the nail plate or the pad of the toe or hand for 2 seconds and measure the time during which the pale area regains its pink color. In healthy people this happens immediately. If microcirculation deteriorates, blanching lasts for a long time. Such microcirculation disorders are nonspecific and are a constant component of any type of shock, and the degree of their severity determines the severity and prognosis of shock. The principles of treatment of microcirculation disorders are also not specific and practically do not differ for all types of shock: elimination of vasoconstriction, hemodilution, anticoagulant therapy, disaggregant therapy.
Metabolic disorders
Under conditions of reduced perfusion of the capillary bed, adequate delivery of nutrients to tissues is not ensured, which leads to metabolic disorders, dysfunction of cell membranes and cell damage. Carbohydrate, protein, and fat metabolism are disrupted, and the utilization of normal energy sources—glucose and fatty acids—is sharply inhibited. In this case, pronounced catabolism of muscle protein occurs.
The most important metabolic disorders in shock are the destruction of glycogen, a decrease in dephosphorylation of glucose in the cytoplasm, a decrease in energy production in mitochondria, disruption of the sodium-potassium pump of the cell membrane with the development of hyperkalemia, which can cause atrial fibrillation and cardiac arrest.
The increase in plasma levels of adrenaline, cortisol, glucagon that develops during shock and the suppression of insulin secretion affect the metabolism in the cell by changes in the use of substrates and protein synthesis. These effects include increased metabolic rate, increased glycogenolysis and gluconeogenesis. A decrease in tissue glucose utilization is almost always accompanied by hyperglycemia. In turn, hyperglycemia can lead to a decrease in oxygen transport, disruption of water-electrolyte homeostasis and glycosylation of protein molecules with a decrease in their functional activity. Significant additional damaging effects of stress hyperglycemia during shock contribute to the deepening of organ dysfunction and require timely correction while maintaining normoglycemia.
Against the background of increasing hypoxia, oxidation processes in tissues are disrupted, their metabolism proceeds along the anaerobic pathway. At the same time, acidic metabolic products are formed in significant quantities, and metabolic acidosis develops. The criterion for metabolic dysfunction is a blood pH level below 7.3, a base deficiency exceeding 5.0 mEq/L and an increase in the concentration of lactic acid in the blood above 2 mEq/L.
An important role in the pathogenesis of shock belongs to the disturbance of calcium metabolism, which intensively penetrates into the cytoplasm of cells. Elevated intracellular calcium levels increase the inflammatory response, leading to intense synthesis of potent mediators of the systemic inflammatory response (SIR). Inflammatory mediators play a significant role in the clinical manifestations and progression of shock, as well as in the development of subsequent complications. Increased production and systemic distribution of these mediators can lead to irreversible cell damage and high mortality. The use of calcium channel blockers improves survival in patients with various types of shock.
The action of pro-inflammatory cytokines is accompanied by the release of lysosomal enzymes and free peroxide radicals, which cause further damage - “sick cell syndrome”. Hyperglycemia and an increase in the concentration of soluble products of glycolysis, lipolysis and proteolysis lead to the development of hyperosmolarity of the interstitial fluid, which causes the transition of intracellular fluid into the interstitial space, dehydration of cells and further deterioration of their functioning. Thus, cell membrane dysfunction may represent a common pathophysiological pathway for various causes of shock. And although the exact mechanisms of cell membrane dysfunction are unclear, the best way to eliminate metabolic disorders and prevent the irreversibility of shock is the rapid restoration of blood volume.
Inflammatory mediators produced during cellular damage contribute to further disruption of perfusion, which further damages cells within the microvasculature. Thus, a vicious circle is completed - impaired perfusion leads to cell damage with the development of systemic inflammatory response syndrome, which in turn further worsens tissue perfusion and cell metabolism. When these excessive systemic responses persist for a long time, become autonomous and cannot be reversed, multiple organ failure syndrome develops.
In the development of these changes, the leading role belongs to tumor necrosis factor (TNF), interlekins (IL-1, IL-6, IL-8), platelet activating factor (PAF), leukotrienes (B4, C4, D4, E4), thromboxane A2, prostaglandins (E2, E12), prostacyclin, interferon gamma. The simultaneous and multidirectional action of etiological factors and activated mediators during shock leads to endothelial damage, disruption of vascular tone, vascular permeability and organ dysfunction.
Persistence or progression of shock may result from either ongoing perfusion defects, cellular damage, or a combination of both. Since oxygen is the most labile vital substrate, its inadequate delivery by the circulatory system forms the basis of the pathogenesis of shock, and timely restoration of tissue perfusion and oxygenation often completely stops the progression of shock.
Thus, the pathogenesis of shock is based on deep and progressive disorders of hemodynamics, oxygen transport, humoral regulation and metabolism. The interrelation of these disorders can lead to the formation of a vicious circle with complete depletion of the body’s adaptive capabilities. Preventing the development of this vicious circle and restoring the body's autoregulatory mechanisms is the main task of intensive care for patients with shock.
Stages of shock
Shock is a dynamic process that begins with the action of the aggression factor, which leads to systemic circulatory disorders, and, as the disorders progress, ends with irreversible damage to organs and death of the patient. The effectiveness of compensatory mechanisms, the degree of clinical manifestations and the reversibility of the resulting changes make it possible to distinguish a number of successive stages in the development of shock.
Preshock stage
Shock is usually preceded by a moderate decrease in systolic blood pressure, not exceeding 20 mm Hg. Art. from normal (or 40 mm Hg if the patient has arterial hypertension), which stimulates the baroreceptors of the carotid sinus and aortic arch and activates the compensatory mechanisms of the circulatory system. Tissue perfusion is not significantly affected and cellular metabolism remains aerobic. If the influence of the aggression factor ceases, then compensatory mechanisms can restore homeostasis without any therapeutic measures.
Early (reversible) stage of shock
This stage of shock is characterized by a decrease in systolic blood pressure below 90 mmHg. Art. , severe tachycardia, shortness of breath, oliguria and cold clammy skin. At this stage, compensatory mechanisms are independently unable to maintain adequate CO and satisfy the oxygen needs of organs and tissues. Metabolism becomes anaerobic, tissue acidosis develops, and signs of organ dysfunction appear. An important criterion for this phase of shock is the reversibility of the resulting changes in hemodynamics, metabolism and organ functions and a fairly rapid regression of developed disorders under the influence of adequate therapy.
Intermediate (progressive) stage of shock
This is a life-threatening critical situation with a systolic blood pressure level below 80 mmHg. Art. and pronounced but reversible organ dysfunction with immediate intensive treatment. This requires artificial pulmonary ventilation (ALV) and the use of adrenergic drugs to correct hemodynamic disorders and eliminate organ hypoxia. Prolonged deep hypotension leads to generalized cellular hypoxia and critical disruption of biochemical processes, which quickly become irreversible. It is on the effectiveness of therapy during the first so-called “golden hour” that the patient’s life depends.
Refractory (irreversible) stage of shock
This stage is characterized by severe disorders of central and peripheral hemodynamics, cell death and multiple organ failure. Intensive therapy is ineffective, even if the etiological causes are eliminated and blood pressure temporarily increases. Progressive multiorgan dysfunction usually leads to irreversible organ damage and death.
Diagnostic testing and monitoring for shock
Shock does not leave time for an orderly collection of information and clarification of the diagnosis before starting treatment. Systolic blood pressure during shock is most often below 80 mmHg. Art. , but shock is sometimes diagnosed at higher systolic blood pressure if there are clinical signs of a sharp deterioration in organ perfusion: cold skin covered with clammy sweat, mental status changes from confusion to coma, oligo- or anuria, and insufficient skin capillary refill. Rapid breathing during shock usually indicates hypoxia, metabolic acidosis and hyperthermia, and hypoventilation indicates depression of the respiratory center or increased intracranial pressure.
Diagnostic tests for shock also include a clinical blood test, determination of electrolytes, creatinine, blood clotting parameters, blood group and Rh factor, arterial blood gases, electrocardiography, echocardiography, and chest radiography. Only carefully collected and correctly interpreted data helps make the right decisions.
Monitoring is a system for monitoring the vital functions of the body, capable of quickly notifying about the occurrence of threatening situations. This allows you to start treatment on time and prevent the development of complications. To monitor the effectiveness of shock treatment, monitoring of hemodynamic parameters, heart, lung and kidney activity is indicated. The number of controlled parameters must be reasonable. Monitoring for shock must necessarily include recording of the following indicators:
- Blood pressure, using intra-arterial measurement if necessary;
- heart rate (HR);
- intensity and depth of breathing;
- central venous pressure (CVP);
- pulmonary artery wedge pressure (PAWP) in severe shock and unknown cause of shock;
- diuresis;
- blood gases and plasma electrolytes.
To approximate the severity of shock, you can calculate the Algover-Burri index, or, as it is also called, the shock index - the ratio of the pulse rate per minute to the value of systolic blood pressure. And the higher this indicator, the greater the danger to the patient’s life. The inability to monitor any of the listed indicators makes the correct choice of therapy difficult and increases the risk of developing iatrogenic complications.
Central venous pressure
Low central venous pressure is an indirect criterion of absolute or indirect hypovolemia, and its rise above 12 cm of water. Art. indicates heart failure. Measuring central venous pressure and assessing its response to a low fluid load helps to select a fluid therapy regimen and determine the appropriateness of inotropic support. Initially, the patient is given a test dose of liquid over 10 minutes: 200 ml at an initial CVP below 8 cm aq. Art. ; 100 ml – with a central venous pressure within 8-10 cm aq. Art. ; 50 ml – with a central venous pressure above 10 cm aq. Art. The reaction is assessed based on the rule “5 and 2 cm aq. Art. ": if the central venous pressure increases by more than 5 cm, the infusion is stopped and the question of the advisability of inotropic support is decided, since such an increase indicates a breakdown of the Frank-Starling contractility regulation mechanism and indicates heart failure. If the increase in central venous pressure is less than 2 cm water. Art. – this indicates hypovolemia and is an indication for further intensive fluid resuscitation without the need for inotropic therapy. Increase in central venous pressure in the range of 2 and 5 cm aq. Art. requires further infusion therapy under the control of hemodynamic parameters.
It must be emphasized that CVP is an unreliable indicator of left ventricular function, since it depends primarily on the condition of the right ventricle, which may differ from the condition of the left. More objective and broader information about the condition of the heart and lungs is provided by monitoring hemodynamics in the pulmonary circulation. Without its use, the hemodynamic profile of a patient with shock is incorrectly assessed in more than a third of cases. The main indication for catheterization of the pulmonary artery in shock is an increase in central venous pressure during infusion therapy. The response to the introduction of a small volume of fluid when monitoring hemodynamics in the pulmonary circulation is assessed according to the rule “7 and 3 mm Hg. Art. "
Hemodynamic monitoring in the pulmonary circulation
Invasive monitoring of blood circulation in the pulmonary circulation is performed using a catheter installed in the pulmonary artery. For this purpose, a catheter with a floating balloon at the end (Swan-Gans) is usually used, which allows you to measure a number of parameters:
- pressure in the right atrium, right ventricle, pulmonary artery and pulmonary artery, which reflects the filling pressure of the left ventricle;
- SV by thermodilution method;
- partial pressure of oxygen and oxygen saturation of hemoglobin in mixed venous blood.
Determination of these parameters significantly expands the possibilities of monitoring and assessing the effectiveness of hemodynamic therapy. The resulting indicators allow:
- differentiate cardiogenic and non-cardiogenic pulmonary edema, identify pulmonary embolism and rupture of the mitral valve leaflets;
- assess blood volume and the state of the cardiovascular system in cases where empirical treatment is ineffective or is associated with an increased risk;
- adjust the volume and rate of fluid infusion, doses of inotropic and vasodilator drugs, and the value of positive end-expiratory pressure during mechanical ventilation.
Decreased oxygen saturation of mixed venous blood is always an early indicator of inadequate cardiac output.
Diuresis
A decrease in diuresis is the first objective sign of a decrease in blood volume. Patients with shock must have a permanent urinary catheter installed to monitor the volume and rate of urination. When carrying out infusion therapy, diuresis should be at least 50 ml/hour. During alcohol intoxication, shock can occur without oliguria, since ethanol inhibits the secretion of antidiuretic hormone.
Clinical manifestations
Transfusion shock develops immediately after transfusion, within several hours after it. The clinic is accompanied by bright characteristic symptoms, but there may be no clear picture. Therefore, after each blood transfusion, the patient should be under medical supervision. The patient's well-being and laboratory signs of transfusion shock are checked. Early detection of complications of blood transfusion requires emergency measures to save the patient's life.
Initial symptoms are:
- short-term excited state of the patient;
- the appearance of shortness of breath, a feeling of heaviness when breathing;
- bluish color of the skin and mucous membranes;
- chills, trembling from feeling cold;
- pain in the lower back, abdomen, chest, and muscles.
The doctor always asks the patient about lower back pain during and after blood transfusion. This sign serves as a “marker” of beginning changes in the kidneys.
Increasing circulatory changes cause further:
- tachycardia;
- pale skin;
- sticky cold sweat;
- sustained decrease in blood pressure.
Less common symptoms include:
- sudden vomiting;
- high body temperature;
- the skin has a marbled tint;
- cramps in the limbs;
- involuntary passage of urine and feces.
In the absence of medical care during this period, the patient develops:
- hemolytic jaundice with a yellow color of the skin and sclera;
- hemoglobinemia;
- acute renal-liver failure.
Features of clinical manifestations of shock if the patient is under anesthesia in the operating room:
- the anesthesiologist records the drop in blood pressure;
- surgeons notice increased bleeding in the surgical wound;
- urine with flakes resembling “meat slop” flows through the outlet catheter into the urinal.
Under anesthesia, the patient does not complain, so all responsibility for the early diagnosis of shock falls on the doctors
Course of the pathology
The severity of shock depends on:
- the patient's condition before blood transfusion;
- volume of blood transfusion.
The doctor can use the level of blood pressure to determine the degree of shock. It is generally accepted to distinguish 3 degrees:
- first - symptoms appear against a background of pressure over 90 mm Hg. Art.;
- the second is characterized by systolic pressure in the range of 70–90;
- the third corresponds to a pressure below 70.
In the clinical course of blood transfusion shock, periods are distinguished. In the classical course, they follow each other; in severe shock, a fleeting change of signs is observed, not all periods can be noticed.
- Transfusion shock itself is manifested by disseminated intravascular coagulation syndrome and a drop in blood pressure.
- The period of oliguria and anuria is characterized by the development of renal block and signs of renal failure.
- The stage of restoration of diuresis occurs when quality medical care is provided and the filtration capacity of the renal tubules is restored.
- The rehabilitation period is characterized by normalization of indicators of the coagulation system, hemoglobin, bilirubin, and red blood cells.
Types of treatment procedures
All therapeutic measures for blood transfusion shock are divided into 3 stages:
Emergency anti-shock therapy - to restore normal blood flow and prevent serious consequences. It includes:
- infusion therapy;
- intravenous administration of antishock drugs;
- extracorporeal methods of blood purification (plasmapheresis);
- correction of the function of systems and organs;
- correction of hemostasis (blood clotting);
- treatment of acute renal failure.
Symptomatic therapy – carried out after stabilization of the patient’s condition during the recovery period (recovery).
Preventive measures - identifying the cause of the development of shock and eliminating similar errors in the future, strict adherence to the sequence of transfusion procedures, conducting compatibility tests, etc.
Primary measures to assist the patient
If characteristic patient complaints or signs of transfusion shock are detected, the doctor must immediately stop the transfusion if it has not yet been completed. As soon as possible you need to:
- replace the transfusion system;
- install a more convenient catheter for further treatment in the subclavian vein;
- establish the supply of humidified oxygen through a mask;
- begin to control the amount of urine excreted (diuresis);
- call a laboratory assistant to urgently draw blood and determine the number of red blood cells, hemoglobin, hematocrit, fibrinogen;
- Submit the patient's urine sample for full urgent analysis.
If possible:
- measurement of central venous pressure;
- analysis of free hemoglobin in plasma and urine;
- electrolytes (potassium, sodium) in plasma, acid-base balance are determined;
- ECG.
The Baxter test is performed by experienced doctors without waiting for laboratory test results. This is a fairly old method that allows you to determine the incompatibility of transfused blood. After injecting about 75 ml of donor blood into the patient, after 10 minutes 10 ml is taken from another vein, the tube is closed and centrifuged. Incompatibility can be suspected by the pink color of the plasma. Normally it should be colorless. This method was widely used in field hospitals in military settings.
Treatment options
Treatment of hemolytic shock and emergency care involve several types of procedures:
- Methods of infusion therapy (infusion of rheopolyglucin, polyglucin, gelatin preparations to stabilize blood circulation and restore microcirculation). Treatment includes the administration of a 4% soda solution to create an alkaline reaction in the urine, which prevents the formation of hemin.
Depending on the level of central venous pressure, an appropriate volume of polyion solutions is transfused, removing free hemoglobin and preventing fibrin degradation.
- Medication methods are used as first aid. They involve the use of classical drugs to recover from a state of shock - prednisolone, aminophylline, Lasix. Antiallergic medications, for example, tavegil, and narcotic analgesics (promedol) are also used.
- Extracorporeal method. This treatment involves removing free hemoglobin, toxins and other products that disrupt the functions of body systems from the patient’s body. Plasmapheresis is used.
- Correcting the functions of systems and individual organs - the use of medications depending on the pathology.
- Correction of the blood coagulation system in renal failure - treatment to restore kidney function.
Prevention of hemolytic shock consists of:
- strict adherence to the rules of blood transfusion;
- storing it correctly;
- thorough examination of donors;
- correct conduct of serological tests.
Prevention is a very important condition when carrying out blood transfusions!
Treatment
Treatment of transfusion shock is determined by the amount of diuresis (based on the amount of urine collected in the urine bag per hour). The schemes are different.
If diuresis is sufficient (more than 30 ml per hour), the following is administered to the patient over 4–6 hours:
- Reopoliglyukin (Polyglyukin, Gelatinol);
- sodium bicarbonate solution (soda), Lactasol for alkalizing urine;
- Mannitol;
- glucose solution;
- Lasix to support diuresis of 100 ml or more per hour.
In total, at least 5–6 liters of liquid must be poured within the specified period.
To relieve vasospasm, the following are indicated: Eufillin, No-shpa, Baralgin
- Drugs that stabilize the permeability of the vascular wall: Prednisolone, ascorbic acid, troxevasin, sodium ethamsilate, Cytomac.
- Heparin is first injected into a vein, then subcutaneously every 6 hours.
- Inhibitors of protease enzymes (Trasilol, Kontrikal) are indicated.
- Antihistamines (Diphenhydramine, Suprastin) are necessary to suppress the rejection reaction.
- Disaggregants such as nicotinic acid, Trental, Complamin are used.
If the patient is conscious, Aspirin can be prescribed.
Reopoliglucin, a soda solution, is administered, but in a much smaller volume. The remaining drugs are used in the same way.
For severe pain, narcotic analgesics (Promedol) are indicated.
Increasing respiratory failure with hypoventilation of the lungs may require a transition to artificial respiration.
If possible, a plasmapheresis procedure is performed - blood is taken, purified by passing through filters and injected into another vein.
If urine output is less than 30 ml per hour, the amount of fluid should be limited to 600 ml + urine output
If disturbances in the electrolyte composition are detected, potassium and sodium preparations are added to treatment.
If acute renal failure is diagnosed, urgent hemodialysis is a measure of help; more than one procedure may be required.
Is it necessary to have a blood transfusion?
The question of the appropriateness of transfusions, as the most significant point in the prevention of transfusion shock, should be considered by the attending physicians before prescribing the procedure. Blood transfusions for anemia are actively used in hematology clinics. In addition to this pathology, absolute indications are:
- large blood loss due to injury or during surgery;
- blood diseases;
- severe intoxication due to poisoning;
- purulent-inflammatory diseases.
Contraindications are always taken into account:
- decompensation of heart failure;
- septic endocarditis;
- cerebrovascular accident;
- glomerulonephritis and renal amyloidosis;
- allergic diseases;
- liver failure;
- tumor with decay.
You should definitely tell your doctor about:
- allergic manifestations experienced in the past;
- reactions to blood transfusions;
- for women about unsuccessful childbirth, children with hemolytic jaundice.
Indications and contraindications for blood transfusion
There are several categories of people who need transfusions. Refusing blood transfusion to people without indications or with contraindications to it is already a prevention of shock.
Indications for transfusion are:
- Massive blood loss during surgery or injury.
- Diseases of the circulatory system (leukemia, etc.)
- Various types of anemia (sometimes transfusion is part of therapeutic measures).
- Severe intoxication leading to the destruction of blood cells.
- Systemic purulent-inflammatory diseases.
- HEMORRHAGIC SHOCK IN OBSTETRICS – Med24info.com
Blood leukemia
Contraindications to transfusion are as follows:
- Heart failure during decompensation (irreversible impairment of heart function).
- Septic endocarditis is inflammation of the inner lining of the heart wall.
- Pathologies of cerebral circulation.
- Allergies.
- State of liver failure.
- Glomerulonephritis (kidney disease, with characteristic damage to the glomeruli).
- Tumor neoplasms in the stage of decay.
You can help your doctor by telling him about any allergic reactions you have and your experience with previous blood transfusions. Women should also talk about the difficult course of childbirth and the presence of hereditary blood pathologies in children.