In cardiological practice, Magnesia to lower blood pressure is used to relieve attacks of arterial hypertension, since it is one of the fastest-acting antihypertensive drugs. The medicine provides rapid expansion of the vascular lumen, thereby reducing blood pressure. Timely stabilization of blood pressure (blood pressure) helps prevent the development of acute vascular complications such as stroke and acute heart failure. Magnesia is used as a first aid remedy to eliminate an attack. What is the mechanism of action of the drug and what are the features of its use?
Composition and release form
Magnesia is an effective medicine that contains one active substance – magnesium salt of sulfuric acid. There are no additional or auxiliary components.
The drug has numerous pharmacological effects, which depend on the route of administration into the body. There are the following dosage forms for using the drug:
- ampoules of 10 ml at a concentration of 25%;
- 5 ml ampoules at a concentration of 25%;
- powder for preparing a suspension;
- tablets in combination with B vitamins.
Pharmacological properties for hypertension
Experts often recommend administering magnesia at high blood pressure due to the rapid achievement of the pharmacological effect. The drug has a wide range of pharmacological effects, namely:
Blood pressure medication Amlodipine
- reduces blood pressure levels;
- expands the vascular lumen;
- stabilizes myocardial activity;
- normalizes heart rhythm disturbances;
- reduces the excitability of the nervous system;
- removes waste products from the body.
The effect of the drug manifests itself immediately after administration into the body, due to which blood pressure levels quickly normalize. The maximum pharmacological effect appears after 30-60 minutes. The therapeutic effect lasts for 3-4 hours.
Effect of magnesium on the body
Magnesia, when administered orally by injection, affects the body as follows:
- sedative, relieving irritation, calming and depressing the central nervous system;
- diuretic (diuretic);
- vasodilator. Vasodilation occurs due to relaxation of muscle tissue in the walls of blood vessels;
- anticonvulsant. Action that reduces skeletal muscle tone. This action is based on a decrease in acetylcholine, a neurotransmitter that ensures the transmission of impulses from nerve endings to muscle fibers, leading to their mechanical movement;
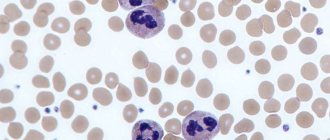
- antiarrhythmic, normalizing heart rate. Positive magnesium ions reduce the excitability of cardiomyocytes and restore ionic balance in cells, stabilizing cell membranes;
- hypotensive, lowering blood pressure. This action is based on vasodilation;
- antispasmodic effect based on the removal of spastic, convulsive contractions of the smooth muscles of internal organs;
- the tocolytic effect is achieved due to inhibition of the contractility of the muscular layer of the uterus, increases blood flow to the uterus due to vasodilation. regulates metabolic processes.
After a certain time, magnesium sulfate is excreted from the body by the kidneys.
In what cases is it used?
Thanks to the rapid stabilizing effect of Magnesia, it is possible to achieve the necessary hypotensive effect during a hypertensive crisis or a condition preceding an attack. However, the use of the drug is limited; it can be used to relieve acute conditions that require emergency care, so its passive use is contraindicated.
Indications for use of the drug:
- Hypertensive crisis (elimination of vascular spasm).
- Epileptic seizure (relaxation of smooth muscles).
- Tachycardia, arrhythmia (normalization of heart rate).
- Nervous excitement (stabilization of the nervous system).
Important! Magnesia to reduce blood pressure is administered intravenously or intramuscularly, depending on the patient's condition. Infections are prescribed by the attending physician, since the drug has many contraindications.
Magnesia for a hangover: how to take the drug
Persons suffering from frequent hangovers with a pronounced reaction of the body to poisoning by alcohol breakdown products are recommended to use magnesium in powder form . Frequency of application – 2-3 times, keeping a break of 50-60 minutes. Within 30 minutes a person can feel an improvement, namely:
- swelling will begin to disappear;
- heart rate will be restored and blood pressure will normalize;
- migraine will ease;
- a sedative effect will be felt;
- Symptoms of intoxication from alcohol metabolites will disappear.
If you decide to use magnesium for a hangover in ampoules or in another form on an ongoing basis, it is recommended that you first consult a doctor to avoid dangerous health consequences.
Features of the action
We need to start with the fact that ethyl alcohol has a detrimental effect on the liver; the enzymes it produces under the influence of alcohol turn into toxic compounds that poison the entire body. They disrupt the function of the entire body, which is why a person with a hangover feels very bad. Since magnesia has a diuretic and laxative effect, it allows you to speed up the process of evacuation of harmful toxins from the body, which leads to a significant and noticeable improvement in your condition.
In general, a person can feel lightness in the body due to the weakening of swelling, the subsidence of headaches, and the normalization of heart rate . Since magnesia also has a sedative effect, it helps eliminate the unpleasant psychological consequences of drinking alcohol:
- depression;
- shame and guilt;
- sudden mood swings due to hormonal changes;
- increased irritability;
- excessive anxiety.
The use of the drug also helps protect the liver and gallbladder from the effects of toxins and breakdown products of alcohol-containing substances.
Mechanism of action for high blood pressure
What mechanism of action does magnesium have, does it reduce blood pressure or not? With high blood pressure, magnesium helps to dilate the blood vessels of the brain, which allows you to normalize blood pressure in a short time. The drug acts when an active substance enters the body, which expands the vascular bed, relieves convulsions and reduces swelling of brain tissue.
The effect of the medicine is also that magnesium is a calcium antagonist. As a result of the penetration of magnesium into the body, it displaces calcium ions, which leads to a reduced concentration of acetylcholine, a substance that regulates vascular tone and the transmission of nerve impulses.
The drug is a cardioprotector, promoting the expansion of coronary arteries and preventing the formation of blood clots
Magnesium sulfate has a sedative effect and also accelerates renal filtration, as a result of which the volume of urine increases, thereby removing excess fluid. The medication is able to quickly and effectively stabilize blood pressure, so the opinion that it increases tonometer readings is erroneous.
Magnesia for hangovers: why is it effective?
Magnesium sulfate is an effective remedy that has long been used by doctors to relieve patients from withdrawal symptoms. As a rule, it is advisable to use it after drinking too large doses of alcoholic beverages.
The main effect of the drug is to replenish magnesium deficiency , which occurs against the background of a hangover. Other related factors can also lead to a deficiency of this substance:
- physical exercise;
- frequent stress;
- lack of vitamins and minerals, monotonous food;
- taking medications for a long time.
At what pressure are injections prescribed?
Why is Magnesia used as an emergency remedy? Before starting use, hypertensive patients should know that hypertension requires long-term treatment with special antihypertensive drugs, and Magnesia is prescribed at the first signs of a hypertensive crisis, when the attack should be quickly eliminated. The medication can greatly reduce blood pressure, but after a few hours it rises again.
It is contraindicated to inject Magnesia at night, as blood pressure may increase in the morning, which increases the risk of developing heart failure. Therefore, arterial hypertension is not treated with the drug. Emergency assistance with Magnesia during a hypertensive crisis is provided at a pressure of 160/110 mm. rt. Art. Sudden increase in blood pressure from 25 to 45 mm. rt. Art. from the usual norm is considered the beginning of an attack at which the drug can be administered.
Magnesia for high blood pressure is administered against the background of the following conditions:
- Eclampsia (a critical form in which a pregnant woman’s blood pressure reaches critical levels).
- Aortic aneurysm dissection.
- Hypertensive encephalopathy (may occur after a hypertensive crisis).
- Brain stroke.
- Cerebral hemorrhage due to hypertension.
When these conditions develop, Magnesia is administered as an adjuvant.
What conclusions can be drawn
In fact, the product does an excellent job of serving its purpose. As reviews of Magnesia for a hangover testify, it perfectly relieves all symptoms of withdrawal symptoms. This occurs due to the rapid removal of all toxic substances formed after the breakdown of ethyl alcohol, which helps all body systems return to normal much faster.
Magnesia can be taken at the same time as drinking alcohol, but this should be done with extreme caution, and the correct solution would be to avoid such phenomena. Doctors' recommendations should not be ignored, and before using the drug it is recommended to consult a specialized doctor.
Features of application
Experts do not recommend using a drip with Magnesia solution to treat arterial hypertension. When the solution is administered by drip, the patient develops more side effects. Therefore, to normalize the indicators, the patient is given intramuscular and intravenous injections. The product can be used only according to indications, as it is quite harmless. Patients are contraindicated to use the solution on their own; it must be administered by a specialist.
In some cases, magnesium sulfate is used for low blood pressure, despite the fact that it is contraindicated in hypotensive conditions. As a rule, with low blood pressure, it is used as a sedative for several days, subject to strict adherence to the administration algorithm, ensuring the absence of side effects.
Intravenous injection to normalize blood pressure
With intravenous administration of Magnesia, the therapeutic effect appears instantly. Experts prescribe an injection of medication to eliminate a hypertensive attack, myocardial infarction, and in the complex treatment of arrhythmia and angina pectoris. In most cases, pathological conditions are accompanied by high tonometer values.
The dose is selected depending on the achievement of the required clinical effect and the concentration of magnesium in the bloodstream. The blood pressure medication is administered intravenously very slowly. The daily dose is from 5 to 20 ml of a 25% solution of the product. The introduction is jet, lasting 5-7 minutes.
With the rapid administration of magnesium sulfate, the patient develops complications:
- dizziness attack;
- increased sweating;
- difficulty breathing;
- hot flash.
If complications develop, the rate of administration must be reduced. The clinical effect lasts for 30 minutes.
Intramuscular injection to lower blood pressure
Magnesia intramuscularly under pressure is used according to the scheme: 1 ampoule of a 25% solution in an amount of 10 ml. Since intramuscular injection is accompanied by painful sensations, the drug is combined with Lidocaine or Novocaine. You can also give an anesthetic injection before directly administering magnesium sulfate. For one ampoule of magnesium sulfate, use an ampoule of anesthetic drug.
Under pressure, the drug is administered intramuscularly according to the following algorithm:
- The patient takes a horizontal position on his side or stomach.
- The needle is inserted into the upper quadrant of the buttock.
- The injection site is treated with an alcohol solution.
- The medicine is administered slowly over 2 minutes.
- The placement of the needle is deep, at a right angle.
Important! With an intramuscular injection of magnesium, there is a high risk of the formation of infiltrates. Therefore, elderly patients are given a reduced dosage, since their kidney filtration capacity is reduced.
The effect of intramuscular administration of the drug is weak, especially for relieving a hypertensive attack. In some situations, this method is used in a hospital with a pronounced increase in blood pressure that is not amenable to antihypertensive medications. The therapeutic effect is observed, but it is insignificant. Therefore, most doctors do not use this medication to reduce indicators.
Modern approaches to the management of patients with back pain
P.R. Kamchatnov
Russian State Medical University, Moscow
One of the most common clinical syndromes is pain in the lumbosacral region (back pain), caused by vertebrogenic pathology. Back pain occurs in 60–80% of the adult population and is one of the most common causes of temporary disability. Episodes of back pain occur annually in half of the working population, with individuals aged 35–55 years most commonly affected. The number of such patients is extremely high, especially in outpatient neurological settings. It is believed that in the vast majority of cases (about 90%), the duration of the pain syndrome does not exceed 6 weeks, however, in other patients the pain becomes chronic. There is a tendency towards an increase in the incidence of musculoskeletal diseases. Thus, in the Russian Federation, the number of such patients over the past 10 years (1988–1997) has increased from 7.7 to 11.2 million (by more than 40%). It should be taken into account that the actual prevalence of these diseases is probably much higher.
The main causes of back pain are degenerative changes in the spine, in particular osteochondrosis, dysfunction of the facet joints, partial tear of the fibrous ring, prolapsed intervertebral discs, in some cases complicated by the formation of a disc herniation, spondylolisthesis, spinal canal stenosis, osteoporosis. It must be taken into account that in some patients the source of pain may be inflammatory changes in the vertebrae or adjacent tissues (spondylitis, osteomyelitis, epidural abscess), including those caused by the influence of a specific pathogen (for example, Koch's bacillus). The cause of pain may be a primary or metastatic tumor of the vertebrae, meninges or spinal roots. Finally, back pain may not be associated with spinal pathology, but be reflected in a wide range of somatic diseases affecting the pelvic organs, hip joint, descending aorta, etc. The variety of causes of pain requires exceptional care when making a diagnosis and developing treatment tactics. In addition to a detailed analysis of the clinical picture of the disease and radiological examination (including the use of computed tomography - CT and magnetic resonance imaging - MRI), there is often a need for an in-depth somatic examination of the patient.
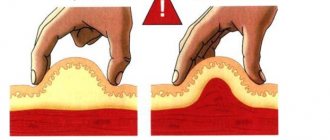
Significant risk factors for the development of intervertebral disc damage are a sedentary lifestyle with a lack of physical activity or, conversely, increased physical activity with repeated microtrauma to the spine, exposure to vibration, excess body weight, high growth, and repeated pregnancies. Production factors play a major role - long stays in vehicles, frequent hypothermia, a discrepancy between the physical capabilities of the individual and the amount of stress experienced. Congenital structural features of the skeleton (asymmetry of leg length, abnormalities in the structure of the hip joints, lumbarization or sacralization, etc.) can also be considered as factors predisposing to the occurrence of degenerative lesions of the spine. There is information about the genetic determinism of intervertebral disc damage, in particular due to impaired production of type 1X collagen.
The presence of long-term chronic pain in the back or lumbar region is closely associated with the development of depression and anxiety disorders, while the frequency of depressive disorders among patients with spondylogenic dorsopathies is 3–4 times higher than in the general population. There is a relationship between the severity and duration of the pain syndrome and the severity of subsequent violations of the motor stereotype and emotional disorders. The presence of depressive and anxiety disorders, especially in combination with pain, can not only cause a decrease in the quality of life of patients, but also lead to permanent disability. Even when acute pain is relieved, emotional disorders can persist for quite a long time, causing maladaptation of the patient.
Management of the patient in the acute period
The main objectives of managing a patient in the acute period of pain as part of spondylogenic dorsopathy are pain relief, restoration of normal spinal biomechanics, and creation of conditions for a full course of rehabilitation measures. The earliest and complete relief of pain syndrome can prevent the fixation of a pathological motor stereotype and provide the opportunity for early rehabilitation measures. In addition, timely elimination of pain provides, on the one hand, the opportunity for early involvement of movement therapy and its activation, and on the other, prevents the development of emotional disorders. Currently, the advisability of choosing a therapeutic tactic that prevents the chronicization of the pathological process is beyond doubt.
In order to eliminate pathogenic physical factors that can cause increased pain, it is recommended to provide a gentle motor regimen, completely eliminate or limit physical activity (“it’s better to lie down for three days than to be treated for a week”). It is advisable to provide a gentle regimen at home or in a neurological hospital. The patient should avoid flexor or rotational movements of the lumbar spine, especially those performed at a fast pace or with additional physical activity. If hospitalization is impossible, immobilization of the corresponding part of the spine should be ensured using orthoses, fixing belts (corsets) equipped with vertical stiffeners. In the acute stage of the disease, characterized by the presence of severe pain, it is, as a rule, inappropriate to carry out active gymnastic exercises, manual massage, as well as the use of thermal procedures and manual therapy sessions. At the same time, with relatively mild exacerbations, in the case of moderate pain syndrome, with a predominance of muscle-tonic disorders, a positive effect can be achieved by performing post-isometric relaxation.
NSAIDs and analgesics
Today, there is no doubt about the advisability of using non-steroidal anti-inflammatory drugs (NSAIDs) for the treatment of patients with spondylogenic dorsopathy. The effectiveness of this approach has been established in a number of clinical studies. A characteristic feature of the pharmacological action of these drugs is the ability to inhibit the activity of cyclooxygenase-2 (COX-2), a key enzyme in the synthesis of prostaglandins, prostacyclins and thromboxanes. The role of COX-2 is known as a major catalyst in the metabolism of arachidonic acid, which is accompanied by the formation of mediators of edema and inflammation. By influencing pain endings at the site of injury, prostaglandins increase their sensitivity to bradykinin, a peptide formed in tissues during inflammation and at the same time being a stimulator of pain endings.
However, inhibition of COX-2 activity during pain syndromes associated with varying degrees of severity of the inflammatory process is not the only analgesic mechanism of NSAIDs. The different severity of the ability to suppress prostaglandin synthesis observed in drugs of this group, the dissociation between the anti-inflammatory and analgesic effects of NSAIDs suggest the existence of other mechanisms for the implementation of analgesic effects in spondylogenic dorsopathies. In addition, no direct relationship was found between the degree of suppression of the synthesis of inflammatory mediators, on the one hand, and the analgesic activity of the drugs, on the other.
The undoubted advantages of the pharmacokinetics of drugs in this group are a short half-life, lack of accumulation and enterohepatic recirculation, and long-term accumulation in the area of inflammation. Thanks to these qualities, drugs have a good benefit/risk ratio. The rapidity of onset of the analgesic effect serves as the basis for prescribing these drugs primarily for the relief of acute pain syndromes of varying intensity. The most common drugs in this group are diclofenac, ketorolac, oxicam derivatives (piroxicam, lornoxicam), propionic acid derivatives (ibuprofen, flurbiprofen, ketoprofen, naproxen).
The widely used diclofenac is characterized by good tolerability, combined with a pronounced analgesic effect. In clinical practice, it is convenient to use a prolonged form of diclofenac retard containing 100 mg of the active substance. Food intake does not have a clinically significant effect on the absorption of the active substance from retard tablets and its systemic bioavailability. The degree of absorption is directly dependent on the dose of the drug. The average maximum concentration of the drug in plasma is achieved on average after 4 hours and persists for 24 hours.
Propionic acid derivatives have a short half-life of about 4 hours and are well tolerated with a relatively low risk of side effects. These drugs are quickly absorbed in the intestine and quickly eliminated; they do not accumulate when metabolic processes are disrupted. They have moderate inhibitory activity on prostaglandin synthesis, and therefore are inferior in their anti-inflammatory effect to diclofenac, indomethacin and phenylbutazone. In this regard, it is advisable to use them for relatively mild dorsopathies with moderate pain.
Unfortunately, the vast majority of NSAIDs have an ulcerogenic effect, which forces the question of the appropriateness of their use and the method of administration into the body to be decided in each individual case. The absence of gastrointestinal diseases allows for oral administration. It is believed that the risk of gastropathy caused by taking NSAIDs is significantly higher in people over the age of 65 years, with long-term (more than 3 months) use of NSAIDs, especially when using two or more drugs from this group, while taking corticosteroids and indirect anticoagulants and , respectively, in patients with a history of gastric ulcer. Possible risk factors are female gender, smoking, alcohol abuse, and the presence of Helicobacter pylori infection. As preventive measures to reduce the risk of damage to the gastric mucosa, proton pump inhibitors (omeprazole 20 mg once a day) or H2-histamine receptor blockers (ranitidine 300 mg per day), as well as antacid drugs, can be used.
If NSAIDs are poorly tolerated, the presence of chronic gastritis, or previous peptic ulcer disease, the use of tablet dosage forms is excluded. In this case, parenteral (intramuscular) or rectal (in the form of suppositories) administration is possible. The use of rectal suppositories is characterized by a high absorption rate (it may correspond to that of oral administration or be slightly lower). Thus, after rectal administration of 50 mg of diclofenac, its maximum concentration in plasma is achieved on average within 1 hour. Unfortunately, the threat of exacerbation of gastrointestinal pathology is not completely excluded in this situation.
Recently, transdermal forms of NSAIDs (ointments, creams, gels) have become widespread. It is necessary to clearly understand that the bioavailability of drugs when administered locally is usually an order of magnitude lower than when administered orally. A serious disadvantage of transdermal dosage forms is the low concentration of the active substance and the limited passage of the drug directly to the pathological focus. Most researchers recognize the advisability of using transdermal forms for moderate pain syndromes, while for severe pain syndromes their effectiveness is clearly insufficient. A pronounced analgesic effect of the treatment can be achieved with repeated (at least 4-6 times a day) application of the drug.
Selective COX-2 inhibitors, which provide inhibition of the synthesis of inflammatory mediators and do not affect the production of prostanoids (celecoxib, nimesulide), attract much attention. The undoubted advantage of these drugs is the relatively low risk of damage to the mucous membrane of the stomach and duodenum. However, their analgesic effect in the acute stage of spondylogenic dorsopathy is not always sufficient, which requires prolongation of the course of therapy or increasing doses of drugs.
In accordance with modern ideas about the formation of pain syndromes, an important role in the formation and regulation of pain is assigned to opioid and non-opioid analgesic systems. Based on this, it can be assumed that one of the most specific and reliable options for pain management is to influence the central mechanisms of pain formation. To reduce the severity of pain in patients with back pain, it is extremely rare to use narcotic drugs. However, in some cases, a positive result is achieved through the use of non-narcotic analgesics. One of them is acetaminophen (paracetamol), an effective pain reliever with a complex mechanism of action. There is reason to believe that analgesia with its use is achieved by increasing the threshold of pain sensitivity, although the central effect of the drug cannot be excluded. It must be borne in mind that in large doses, acetaminophen can have nephro- and hepatotoxic effects, and the risk increases with alcohol intake and other exogenous intoxications.
The timing of use of NSAIDs and analgesics is determined by the intensity of the pain syndrome; the course of their use is stopped as the effect is achieved. It should be noted that the “prophylactic” use of NSAIDs in patients with spondylogenic dorsopathies in the absence of pain is inappropriate - no convincing evidence of a preventive effect has been obtained, while the risk of complications increases significantly.
Increasing the effectiveness of the use of NSAIDs can be achieved by combining drugs that affect various parts of the pathogenesis of pain. The observed potentiation of the effect makes it possible to use relatively low doses of drugs and minimize the pharmacological load on the patient’s body. For this purpose, in some patients, intravenous drip administration of a mixture of painkillers, sedatives, and diuretics can be used. In addition to the mutually potentiating effect of adequately selected components of the “cocktail,” the psychotherapeutic effect of this method of treatment cannot be excluded.
Muscle relaxants
A combination of painkillers with muscle relaxants that reduce the severity of muscle-tonic manifestations has a good therapeutic effect. This complex can be effective for both compression and reflex syndromes. Benzodiazepine derivatives (diazepam, tetrazepam), tolperisone, and tizanidine are used as drugs that reduce increased muscle tone. Tizanidine, in addition to its relaxing effect on striated muscles, has a moderate gastroprotective effect. The mechanism of this effect is not entirely clear, although there is evidence that the drug, acting through central alpha-adrenergic pathways, inhibits the production of gastric secretions, prevents changes in glycoproteins caused by the action of acetylsalicylic acid or NSAIDs, and damage to the gastric mucosa. Considering that almost all muscle relaxants have a sedative effect to one degree or another, the patient should be informed about possible side effects - drowsiness, decreased concentration, lethargy. Often the severity of these effects limits the use of this group of drugs in outpatient settings.
Decongestant therapy
In some cases, compression syndrome is accompanied by local venous congestion, swelling of the root and surrounding tissues, which makes it advisable to include diuretics (saluretics or osmotic) and, in some severe cases, corticosteroids in the therapeutic complex. Hormonal drugs usually use prednisolone (40–60 mg per day) or dexamethasone (4–8 mg per day) for 3–5 days, followed by rapid withdrawal. The increased risk of gastrointestinal complications must be taken into account when corticosteroids and NSAIDs are used concomitantly. Epidural corticosteroids are used in a number of countries. Data were obtained on the effectiveness of this method of treatment in patients with acutely developed pain syndrome. Less justified is the epidural administration of drugs for moderate pain in the lower back and lower back, as well as for their chronic or subacute nature.
Combination drugs
A successful combination of drugs that have analgesic and anti-edematous effects, which have a positive effect on metabolism in the peripheral nerve and surrounding tissues, is the drug “Ambene”. Available in the form of a ready-to-use two-chamber syringe for injection, the first chamber of which contains 2 ml of phenylbutazone solution (375 mg) and 3.5 mg of dexamethasone, the second - 1 ml of cyanocobalamin (2.5 mg). In addition, Ambene contains lidocaine, the addition of which reduces pain directly at the injection site. Solutions are mixed immediately before use. The therapeutic effects of the components included in Ambene are potentiated, thereby ensuring a quick and lasting analgesic effect.
Phenylbutazone is a pyrazolone-type NSAID, which, by inhibiting COX activity, reduces the production of prostaglandins and has an analgesic and anti-inflammatory effect. The pronounced analgesic effect is combined with good tolerability, so the daily dose can be up to 1200–1600 mg. Dexamethasone is a synthetic glucocorticoid with powerful anti-inflammatory, antiallergic, desensitizing, and anti-edematous effects. The main clinical effects are realized due to inhibition of the release of inflammatory mediators by eosinophils, membrane-stabilizing effects, and a decrease in the number of mast cells. Cyanocobalamin (vitamin B12) is involved in the metabolism of a number of biologically active substances and has high biological activity, including in relation to metabolic processes in the peripheral nervous system.
Ambene has a pronounced analgesic effect in patients with spondylogenic dorsopathy, and is well tolerated. The drug is administered intramuscularly once a day, no more than once every 2–3 days. It should be borne in mind that individual components of the drug can cause unwanted side effects. Like other NSAIDs, phenylbutazone has an ulcerogenic effect; skin manifestations (urticaria, dry eczema) are relatively rare. Dexamethasone is characterized by a low incidence of side effects, however, it is necessary to keep in mind the possibility of reducing glucose tolerance and increasing the risk of developing erosive and ulcerative lesions of the stomach and duodenum. Based on this, Ambene should not be used in patients with acute diseases of the stomach and duodenum, impaired carbohydrate metabolism (decreased glucose tolerance), or individual intolerance to its individual components.
Relief of both compression and reflex pain syndromes can be achieved by blocking painful muscle groups or trigger points. Technically correctly performed, these manipulations are quite effective and do not cause significant complications. Care is required when performing paravertebral blocks to avoid trauma to the spinal roots. Combinations of anesthetic solution (novocaine, lidocaine) and a small dose of corticosteroid (hydrocortisone suspension, betamethasone dipropionate) are used. Local administration of drugs that have a systemic rather than local effect (antiplatelet agents, vasoactive drugs, muscle relaxants, etc.), and also do not have the ability to be deposited in tissue, is impractical. Unfortunately, the effect of blockades on pain is not lasting, and therefore there is a need for repeated manipulations.
In some cases, the use of NSAIDs, even in combination with muscle relaxants, does not have the desired positive effect. Chronic pain syndrome is accompanied by emotional disorders, in particular with a predominance of depressive reactions, which dictates the need to expand the pharmacotherapeutic arsenal. Research in recent years has convincingly demonstrated that the chronicity of pain in patients with lumbar pain is due to psychological rather than biomechanical reasons (i.e., directly related to the pathology of the spine and roots). The consequence of this is an increase in the recovery process, a sharp limitation in the possibility of motor rehabilitation of patients, and disruption of interaction in the “doctor-patient” system. The reasons that complicate the recovery process are the patient’s belief in the presence of progressive organic damage to the spine, the need to completely limit physical activity, impairment of social functions associated with the disease, orientation towards passive (medicinal, physiotherapeutic) but not active treatment (dosed physical activity, special exercises). A powerful therapeutic tool in this situation is conducting explanatory psychotherapy, developing optimistic views in the patient about the prospects for treatment, developing a behavior strategy for the future (optimal volume and nature of work and household stress, carrying out preventive measures, etc.).
Antidepressants and anticonvulsants
In this situation, antidepressants can be added to treatment, and it is advisable to use drugs that have a sedative and muscle relaxant effect (for example, amitriptyline). Carbamazepine, an effective anticonvulsant from the group of iminostilbene derivatives, has an analgesic effect. The drug inactivates sodium channels, inhibits the release of excitatory neurotransmitters into the synaptic cleft, causing a decrease in synaptic transmission. In addition to the main anticonvulsant and analgesic effect, the drug has antipsychotic and antimanic effects. It has been suggested that the positive effect of carbamazepine in patients with spondylogenic dorsopathies may be mediated by its effect on central nociceptive mechanisms and normalization of muscle tone. Dosing of the drug is carried out individually, depending on tolerability, as well as on the nature of the motor mode. Side effects (primarily drowsiness, impaired concentration) require care in selecting the dose of the drug, especially in an outpatient setting. The likelihood of these disorders increases with the simultaneous prescription of sedatives, antidepressants, and some muscle relaxants. Convincing data on the advisability of using other anticonvulsants has not been obtained, although studies of this kind are being conducted.
The complex of therapeutic measures should also include non-drug treatment methods - physiotherapy (phono- or electrophoresis of drugs, exposure to electric currents of a specially selected configuration, frequency and voltage, low-energy laser radiation). Reflexology in various modifications (traditional acupuncture, electro- and laser puncture) has an analgesic effect. It should be noted that there are significant difficulties in comparing the results of using various physiotherapeutic treatment methods, and the obvious lack of research on their effectiveness that meets the requirements of evidence-based medicine.
Currently available data indicate the existence of a significant arsenal of pharmacotherapeutic and non-drug methods for relieving pain in patients with spondylogenic dorsopathies. It seems desirable to make an individual choice of therapeutic tactics using a combination of different drugs, their dosages and routes of administration. The combined use of various treatment methods can increase the effectiveness of treatment and reduce the pharmacological load on the body. As the pain syndrome is relieved, it is absolutely necessary to use methods of restorative therapy, therapeutic exercises aimed at forming a muscle corset, strengthening the muscles of the abdominal wall and back. Equally important is teaching the patient the skills of daily physical activity - the formation of a motor stereotype that prevents the occurrence of pain.
Source: https://www.consilium-medicum.com/media/consilium/04_08/557.shtml :: Wednesday, 10-Nov-2004 21:25:33 MSK
Use during pregnancy
To normalize blood pressure during pregnancy, experts recommend taking milder antihypertensive drugs. However, if during the period of bearing a child a persistent increase in blood pressure is registered in a woman, then Magnesia is prescribed in the form of intravenous injections.
Administration of the drug is contraindicated in early pregnancy, since the active substance negatively affects the formation of the fetus
Intravenous administration of magnesium sulfate can normalize blood pressure and eliminate seizures. To reduce the risk of miscarriage, intramuscular injections are used, which relaxes the smooth muscles of the uterus and eliminates hypertonicity.
Magnesium sulfate is used during pregnancy for the following indications:
- persistent and prolonged increase in blood pressure values;
- eclampsia;
- gestosis;
- threat of premature birth;
- magnesium deficiency in the body.
How much solution should be administered to stabilize the indicators? For severe hypertension, the dose is calculated depending on the woman’s condition, characteristics of the course of pregnancy, and the presence of chronic diseases. As a rule, to normalize the tonometer values, 20 ml of a 25% magnesium sulfate solution is prescribed. The concentration of the active substance after injection will be equal in both mother and child, so the woman’s condition should be monitored to prevent adverse reactions.
What is the drug
This is a medicine whose main active ingredients are magnesium sulfuric acid salts. The drug is also known under other names, such as: Epsom salts, magnesium B6, magnesium sulfate. It is successfully used in various areas of healthcare due to its wide spectrum of action. Magnesia copes well with the following tasks:
- calms the nervous system;
- causes a mild diuretic effect;
- dilates blood vessels;
- causes a laxative effect;
- relaxes the muscles of the uterus;
- stabilizes heartbeat;
- improves bile flow;
- relieves spasms;
- has an analgesic effect.
Magnesia is initially a powder from which suspensions are prepared. In pharmacies it is possible to purchase a ready-made solution for injection. It is the method of administration of the solution that determines what properties the drug will exhibit.
For maximum effect, it is recommended to administer it intramuscularly or intravenously. In this case, it will have an anticonvulsant, antispasmodic and sedative effect. When intramuscularly , it must be injected deeply using the two-step method. If magnesium sulfate is administered intravenously, it should be done slowly. Regardless of the type of injection, the effect of the medication is aimed at:
- exclusion of cardiac arrhythmia;
- vasodilation;
- elimination of seizures;
- eliminating anxiety.
If the dose is exceeded, it can have a hypnotic and narcotic effect on humans. Intramuscular administration manifests its effect after 60-90 minutes and can last up to 4 hours. Intravenous treatment begins to act almost instantly, but its effect lasts for 30 minutes, after which it weakens significantly.
If you plan to use the oral method of taking the medicine, it will cause a laxative and choleretic effect within half an hour to an hour after its use. The effect lasts up to 6 hours.
An effective remedy for severe poisoning with salts of heavy metals, for example, mercury, arsenic, lead. MgSO4 combines with toxic substances and promotes their rapid elimination from the body due to its diuretic and laxative effect.
However, Magnesia is not always used internally. It has found application in external treatment. It can be used to perform antiseptic treatment of wounds. It is successfully used for electrophoresis, preparing lotions, and healing baths. When compresses with magnesium sulfate are applied, blood flows to this area, providing relief from inflammatory reactions and pain relief.