Varieties, reasons
Brain edema occurs:
- vasogenic;
- cytotoxic;
- interstitial;
- osmotic.
The signs of cerebral edema depend on the type of developing pathology.
Causes of disease progression:
- Vasogenic edema occurs due to increased cerebral vascular permeability.
- Cytotoxic is the “swelling” of brain cells due to an increase in the amount of fluid inside them.
- Interstitial edema develops when there is increased pressure of the cerebrospinal fluid in the ventricles of the brain.
- Osmotic edema - with an increase in the osmolarity of brain tissue.
The most common reasons that cause brain swelling are: brain injury and disruption of its tissues in various pathologies.
Brain edema most often occurs in the following pathological conditions of a traumatic nature:
- brain contusion;
- fracture of the base of the skull;
- intracerebral hematoma;
- subdural hematoma. The prognosis of surgery for cerebral edema depends on its size.
The described pathology develops against the background of such organic brain lesions:
- ischemic and hemorrhagic stroke;
- hemorrhage under the arachnoid membrane;
- tumors;
- infectious diseases - encephalitis (inflammation of brain tissue) and meningitis (inflammation of the meninges).
Extracranial causes of cerebral edema can result from:
- Quincke's edema is a severe allergic reaction of the body;
- infectious diseases - scarlet fever, measles, mumps;
- diabetes;
- liver failure;
- alcoholism.
On our website Dobrobut.com you will find more information about the causes of cerebral edema in a newborn child, the development of pathology in the elderly and other facts.
Contraindications to the use of Dexamethasone
- For short-term use for “life-saving” indications, the only contraindication is hypersensitivity; systemic mycosis;
- simultaneous use of live and attenuated vaccines with immunosuppressive doses of the drug;
- sucrose intolerance, isomaltase/sucrase deficiency, glucose-galactose malabsorption; breastfeeding period; children up to 3 years old.
Carefully:
Parasitic and infectious diseases of a viral, fungal or bacterial nature (currently or recently suffered, including recent contact with a patient) –
- herpes simplex, herpes zoster (viremic phase), chicken pox, measles;
- amebiasis, strongyloidiasis (established or suspected);
- active and latent tuberculosis.
Signs of cerebral edema
Symptoms depend on how quickly brain swelling develops.
Signs of acute cerebral edema:
- disturbance of consciousness - from slight stupor to a state of coma with cerebral edema;
- convulsions – occur as swelling progresses;
- muscle atony – develops after seizures;
- membrane symptoms.
Gradual increase in edema – additional symptoms of cerebral edema in adults:
- headache;
- nausea and vomiting that does not bring relief;
- movement disorders;
- visual and speech disorders;
- hallucinatory syndrome.
Signs indicating critical development of the condition:
- paradoxical breathing (deep breaths with long gaps between them);
- a sharp decrease in blood pressure;
- unstable pulse;
- increase in body temperature above 40 degrees Celsius.
The appearance of such signs indicates compression of the brain stem, which leads to death.
Description of the dosage form
Tablets are white, flat-cylindrical with a chamfer.
Pharmacokinetics
Absorption
After oral administration, it is quickly and completely absorbed, the maximum concentration of dexamethasone in the blood plasma is 1-2 hours.
Distribution
In the blood it binds (60–70%) to a specific carrier protein – transcortin. Easily passes through histohematic barriers (including the blood-brain and placental barriers).
Metabolism
Metabolized in the liver (mainly by conjugation with glucuronic and sulfuric acids) to inactive metabolites.
Removal
Excreted by the kidneys (a small amount of dexamethasone passes into breast milk). Half-life is 3-5 hours.
Pharmacodynamics
Dexamethasone is a synthetic glucocorticosteroid (GCS), a methylated derivative of fluoroprednisolone. It has anti-inflammatory, antiallergic, desensitizing, immunosuppressive, antishock and antitoxic effects.
Inhibits the secretion of thyroid-stimulating hormone and follicle-stimulating hormone.
Increases the excitability of the central nervous system, reduces the number of lymphocytes and eosinophils, increases the number of red blood cells (stimulates the production of erythropoietin). Interacts with specific cytoplasmic receptors and forms a complex that penetrates the cell nucleus, stimulates the synthesis of matrix ribonucleic acid (mRNA); the latter induces the formation of proteins, including lipocortin, that mediate cellular effects. Lipocortin inhibits phospholipase A2, suppresses the release of arachidonic acid and suppresses the synthesis of endoperoxides, prostaglandins, leukotrienes, which contribute to inflammation, allergies and others.
Effect on protein metabolism: reduces the amount of protein in plasma (due to globulins) with an increase in the albumin/globulin ratio, increases albumin synthesis in the liver and kidneys; enhances protein catabolism in muscle tissue.
Effect on lipid metabolism: increases the synthesis of higher fatty acids and triglycerides, redistributes fat (fat accumulation mainly in the shoulder girdle, face, abdomen), leads to the development of hypercholesterolemia.
Effect on carbohydrate metabolism: increases the absorption of carbohydrates from the gastrointestinal tract (GIT); increases the activity of glucose-6-phosphatase, leading to an increase in the flow of glucose from the liver into the blood; increases the activity of phosphoenolpyruvate carboxylase and the synthesis of aminotransferases, which leads to the activation of gluconeogenesis.
Effect on water-electrolyte metabolism: retains sodium ions and water in the body, stimulates the excretion of potassium ions (mineralocorticosteroid activity), reduces the absorption of calcium ions from the gastrointestinal tract, “washes out” calcium ions from the bones, increases the excretion of calcium ions by the kidneys.
The anti-inflammatory effect is associated with inhibition of the release of inflammatory mediators by eosinophils; inducing the formation of lipocortins and reducing the number of mast cells that produce hyaluronic acid; with a decrease in capillary permeability; stabilization of cell membranes and organelle membranes (especially lysosomal ones).
The antiallergic effect develops as a result of suppression of the synthesis and secretion of allergy mediators, inhibition of the release of histamine and other biologically active substances from sensitized mast cells and basophils, a decrease in the number of circulating basophils, suppression of the development of lymphoid and connective tissue, a decrease in the number of T and B lymphocytes, mast cells, reducing the sensitivity of effector cells to allergy mediators, suppressing antibody formation, changing the body's immune response.
In chronic obstructive pulmonary disease, the effect is based mainly on inhibition of inflammatory processes, inhibition of development or prevention of swelling of the mucous membranes, inhibition of eosinophilic infiltration of the submucosal layer of the bronchial epithelium, deposition of circulating immune complexes in the bronchial mucosa, as well as inhibition of erosion and desquamation of the mucous membrane. Increases the sensitivity of beta-adrenergic receptors of small and medium-caliber bronchi to endogenous catecholamines and exogenous sympathomimetics, reduces the viscosity of bronchial secretions due to inhibition or reduction of its production.
Antishock and antitoxic effects are associated with an increase in blood pressure (due to an increase in the concentration of circulating catecholamines and restoration of the sensitivity of adrenergic receptors to them, as well as vasoconstriction), a decrease in the permeability of the vascular wall, membrane protective properties, and activation of liver enzymes involved in the metabolism of endo- and xenobiotics.
The immunosuppressive effect is due to inhibition of the release of cytokines (interleukin-1, interleukin-2; interferon gamma) from lymphocytes and macrophages. Suppresses the synthesis and secretion of adrenocorticotropic hormone (ACTH), and secondarily the synthesis of endogenous GCS.
The peculiarity of the action is significant inhibition of pituitary function and the almost complete absence of mineralocorticosteroid activity. Doses of 1-1.5 mg/day inhibit the adrenal cortex; biological half-life is 32-72 hours (duration of inhibition of the hypothalamic-pituitary-adrenal cortex system).
In terms of the strength of glucocorticoid activity, 0.5 mg of dexamethasone corresponds to approximately 3.5 mg of prednisolone, 15 mg of hydrocortisone or 17.5 mg of cortisone for oral dosage forms.
Diagnostics
Cerebral edema should be suspected if impairment of consciousness increases, meningeal symptoms are observed, and the patient's condition worsens.
Instrumental methods that are used to confirm the diagnosis of cerebral edema:
- computed tomography (CT);
- magnetic resonance imaging (MRI). This is an important diagnostic method - you can detect swelling of the spinal cord on MRI, and not just the brain.
Of the laboratory research methods, general and biochemical blood tests are important.
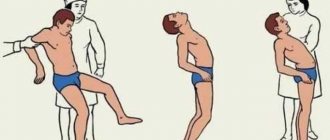
It is dangerous to perform a lumbar puncture for diagnostic purposes - displacement of brain structures and jamming of the brain stem in the occipital foramen of the skull may occur.
Composition and release form
Tablets - 1 tablet:
- Active ingredient: Dexamethasone – 0.0005 g
- Excipients: potato starch – 0.0340 g; sucrose (sugar) – 0.1140 g; stearic acid – 0.0015 g.
Tablets weighing 0.15 g.
Tablets 0.5 mg.
10, 14 tablets in a blister pack made of polyvinyl chloride film and aluminum foil.
5, 10 blister packs of 10 tablets each or 4 blister packs of 14 tablets each with instructions for use in a cardboard pack.
Treatment of cerebral edema
The main principles of treatment for cerebral edema are:
- dehydration;
- improvement of metabolic processes in the brain;
- etiotropic treatment;
- symptomatic therapy.
What consequences of cerebral edema during stroke and other pathologies will accompany the patient depends on the timeliness and competence of the therapy.
Dehydration therapy
Its purpose is to remove excess fluid from brain tissue. Based on the appointments:
- osmotic diuretics (diuretics);
- magnesium sulfate and glucose solution - they enhance the effect of diuretics and also improve brain nutrition;
- L-lysine escinate - the drug is not a diuretic, but removes fluid.
Improving brain processes
For this purpose the following are appointed:
- metabolic drugs;
- glucocorticosteroids;
- oxygen therapy.
Etiotropic therapy
When treating cerebral edema, it is necessary to eliminate the causes of the development of the pathology and “destroy” the mechanism of edema formation. Destination:
- antibiotics;
- removal of tumors and hematomas;
- shunt operations, after which cerebral blood supply improves
This treatment is carried out after the patient’s condition has stabilized.
Symptomatic therapy
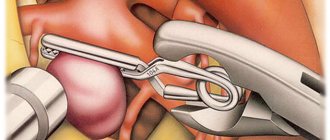
It is aimed at eliminating cramps, vomiting, pain, and so on. In addition to conservative therapy, surgical treatment can be used:
- decompression craniotomy;
- Ventricular drainage.
Use of Dexamethasone during pregnancy and children
Dexamethasone crosses the placenta (can reach high concentrations in the fetus) and into breast milk. During pregnancy, especially in the first trimester, or in women planning pregnancy, the use of Dexamethasone is indicated only if the expected therapeutic effect outweighs the risk of negative effects on the mother or fetus. GCS should be prescribed during pregnancy only for absolute indications. With long-term therapy during pregnancy, the possibility of fetal damage cannot be excluded. If used in the third trimester of pregnancy, there is a risk of atrophy of the adrenal cortex in the fetus, which may require replacement therapy in the newborn. If it is necessary to carry out treatment with the drug during breastfeeding, breastfeeding should be stopped.
How to quickly relieve facial swelling in adults
If this is physiological swelling of the face, not associated with serious pathologies that require medical supervision and the use of selected medications, excess fluid can be eliminated through certain simple measures and actions.
Taking a contrast shower or washing with cold/hot water. This method refreshes, increases tissue tone, enhances the outflow of fluid from the skin and reduces swelling.
Using ice – a couple of pieces of ice will help deal with swelling on the face quickly and effectively. In addition, you can prepare herbal decoctions with a tonic effect in advance and freeze them, using them for washing.
Facial massage is an effective remedy that helps improve microcirculation and swelling. Manual massage, the use of rollers, ice cubes, and cold spoons help. Sometimes you can first wipe your face with green tea and apply compresses with it to your face and eye area.
Dexamethasone dosage
Orally, in individually selected doses, the amount of which is determined by the type of disease, the degree of its activity and the nature of the patient’s response.
The average daily dose is 0.75-9 mg. In severe cases, large doses can be used, divided into 3-4 doses. The maximum daily dose is usually 15 mg. After achieving a therapeutic effect, the dose is gradually reduced (usually by 0.5 mg every 3 days) to a maintenance dose of 2-4.5 mg/day. The minimum effective dose is 0.5-1 mg/day.
Children (depending on age) are prescribed 83.3-333.3 mcg/kg or 2.5-10 mg/sq.m/day in 3-4 doses.
The duration of dexamethasone use depends on the nature of the pathological process and the effectiveness of treatment and ranges from several days to several months or more. Treatment is stopped gradually (at the end several injections of corticotropin are prescribed).
For bronchial asthma, rheumatoid arthritis, ulcerative colitis – 1.5-3 mg/day; for systemic lupus erythematosus – 2-4.5 mg/day; for oncohematological diseases – 7.5-10 mg.
For the treatment of acute allergic diseases, it is advisable to combine parenteral and oral administration: 1 day – 4-8 mg parenterally; Day 2 – orally, 4 mg 3 times a day; 3, 4 days – orally, 4 mg 2 times a day; 5, 6 days – 4 mg/day, orally; Day 7 – drug withdrawal.
Dexamethasone test (Liddle test). It is carried out in the form of small and large tests. For a small test, dexamethasone is given to the patient 0.5 mg every 6 hours during the day (that is, at 8 a.m., 2 p.m., 8 p.m., and 2 a.m.). Urine for the determination of 17-hydroxycorticosteroids or free cortisol is collected from 8 a.m. to 8 a.m. 2 days before the administration of dexamethasone and also 2 days at the same time intervals after taking the indicated doses of dexamethasone. These doses of dexamethasone inhibit the formation of corticosteroids in almost all apparently healthy individuals. 6 hours after the last dose of dexamethasone, plasma cortisol levels are below 135-138 nmol/l (less than 4.5-5 mcg/100 ml). Reducing the excretion of 17-hydroxycorticosteroids below 3 mg/day, and free cortisol below 54-55 nmol/day (below 19-20 mcg/day) excludes hyperfunction of the adrenal cortex. In persons suffering from Cushing's disease or syndrome, no changes in the secretion of corticosteroids are observed during a small test.
When conducting a large test, dexamethasone is prescribed 2 mg every 6 hours for 2 days (that is, 8 mg dexamethasone per day). Urine is also collected to determine 17-hydroxycorticosteroids or free cortisol (if necessary, determine free cortisol in plasma). With Itsenko-Cushing's disease, there is a decrease in the excretion of 17-hydroxycorticosteroids or free cortisol by 50% or more, while with adrenal tumors or adrenocorticotropic-ectopic (or corticoliberin-ectopic) syndrome, the excretion of corticosteroids does not change. In some patients with adrenocorticotropic-ectopic syndrome, a decrease in the excretion of corticosteroids is not detected even after taking dexamethasone at a dose of 32 mg/day.