General information
Cerebral edema is one of the manifestations of various critical conditions and is quite often encountered in clinical practice with various kinds of diseases and the development of pathologies. There are edema of the brain, spinal and bone marrow.
Brain swelling
Brain edema is an increase in its volume, caused by the accumulation of fluid in the intercellular space (interstitium) and accompanied by an increase in the volume of brain tissue. While an increase in brain volume due to intracellular fluid is defined by the term “swelling” of the brain. However, these processes (edema/swelling) can develop simultaneously and transform into each other, therefore both of these concepts can be defined as cerebral edema. ICD-10 cerebral edema code: G93.6
Edema syndrome develops as a nonspecific reaction of the body to the influence of many pathogenic factors. Possible in a number of diseases/pathological conditions that occur with damage to the nervous system - traumatic brain injury , acute cerebrovascular , infectious diseases, hypoxia , intoxication , brain tumors ( perifocal edema ), acute somatic diseases accompanied by impaired water-salt balance / hemodynamics, with endocrine disorders, blood diseases, after surgical interventions, exposure to ionizing radiation, etc. Brain edema is often one of the manifestations of critical conditions and the direct cause of death of the patient.
As a rule, cerebral edema at an early stage (with timely medical correction) is a reversible process, while with inadequate/late treatment, pathological processes increase and often end with the degeneration of brain nerve cells with disruption of their function and, in general, functional failure of brain structures.
Due to the accumulation of fluid in the interstitium of the brain, an increase in brain volume occurs in conditions of limited intracranial space with the development of mass effect (pathological effect of expanding tissue on neighboring structures, causing compression, deformation, displacement, atelectasis), which is primarily manifested by the development of intracranial hypertension (ICP) ) with a controlled increase in cerebral ischemia , and in severe cases - with displacement of brain structures and infringement of the stem sections in the tentorium of the cerebellum, accompanied by dysfunction of vital centers.
Spinal cord swelling
Most often, swelling of the spinal cord develops with traumatic injuries to the spine. Pathological disorders are formed both as a result of traumatic injury and compression of the spinal cord structures due to its edema-swelling, which is accompanied by ischemia of the brain substance, inflammatory changes and a high risk of developing irreversible disorders of the function/structure of the spinal cord. Compression of the spinal cord causes the formation of primary/secondary softening lesions in the spinal cord and is accompanied by neurological symptoms. Clinical manifestations are determined by the level of localization of edema, its severity and duration. With severe edema, it manifests itself as a syndrome of partial/complete disruption of spinal cord conduction.
Bone marrow edema (trabecular bone marrow edema)
There are subchondral and trabecular edema of the bone marrow. Trabecular edema - what is it? Spongy substance (syn. trabecular tissue) of bone consists of loose partitions/plates, the spaces between which are filled with bone marrow, which ensures hematopoiesis in the human body and the formation of immune chains. Edema of the spongy tissue is manifested by the accumulation of exudate (interstitial fluid) in the trabecular plates. At the same time, the liquid level increases from 10 to 20% or more. In most cases, the diagnosis is made late, since there are no specific symptoms and the disease is detected only on MRI.
According to the literature, bone marrow edema occurs more often in middle-aged patients and mainly affects large joints, the condyles of the tibia/femur. The most common (trabecular edema of the lateral condyle of the femur, bone marrow edema of the hip joints, bone marrow edema in the diaphysis of the radius, swelling of the condyle of the femur, etc.). Spinal bone marrow edema is much less common .
The causes of bone marrow edema are extremely diverse ( bruises / fractures , vitamin D deficiency , rheumatoid arthritis , osteoarthritis , benign / malignant tumors , osteomyelitis , spondylitis , arthrosis deformans , endocrine pathologies accompanied by impaired cellular metabolism, status epilepticus , acute neuroinfections , etc.) . The mechanisms of development of bone marrow edema are poorly understood. It is assumed that its development is facilitated by microvascular trauma, abnormal mechanical loads on bones/joints, metabolic disorders, and venous obstruction. Due to the small volume of the article, only cerebral edema will be considered.
Consequences of cerebral edema
As one of the critical conditions, cerebral edema very often ends in the death of the patient. The occurrence of edema marks either decompensated changes in the body of a general nature, or damage to brain tissue that is practically incompatible with life. All this makes cerebral edema an extremely unpredictable pathology, which may not respond to improvement with treatment. Among all the possible outcomes of cerebral edema, only three can be distinguished.
Progression of edema with transformation into brain swelling and death
A similar scenario, unfortunately, occurs in half of cases of cerebral edema of any origin. The danger of the situation is that as swelling progresses, a critical accumulation of fluid occurs in the brain tissue. This causes their pronounced swelling and increase in volume. As long as there is space in the cranial cavity to be filled with edematous cells, the condition of the patients remains relatively stable. But as soon as the free space is filled, compression of the brain occurs. As edema progresses, dense brain structures move into softer ones, which is called dislocation. Its typical variant is the wedging of the cerebellar tonsils into the brain stem, which ends in cessation of breathing and heartbeat.
Complete elimination of edema without consequences for the brain
This scenario is very rare and is possible only when cerebral edema occurs in young somatically healthy people due to intoxication with alcohol or other compounds toxic to the brain. If such patients are delivered on time to specialized toxicology or general intensive care units, and the dose of toxins turns out to be compatible with life, then the cerebral edema will be stopped and will not leave any pathological symptoms.
Elimination of cerebral edema with patient disability
The second most common outcome of this disease. Possible in patients with meningitis, meningoencephalitis of moderate severity, as well as with traumatic brain injuries in the form of small, timely diagnosed and operated on intracranial hematomas. Sometimes the neurological deficit is so minimal that it does not cause any visual manifestations.
Pathogenesis
The development of edema is initially based on microcirculatory disorders. Almost immediately after neuronal damage, regardless of its cause (hemorrhage, trauma, ischemia, tumor, inflammation), cytotoxic perifocal cerebral edema develops, and later, against its background, dysfunction of the capillary epithelium develops with accumulation of fluid in the interstitial space. In the development of endothelial dysfunction, several stages are distinguished, which are accompanied initially by functional (ion edema), then anatomical (vasogenic edema/hemorrhagic transformation) failure, as well as failure of the blood-brain barrier.
The development of cytotoxic edema is based on the accumulation of osmotically active substances inside cells (potassium/sodium/chlorine ions and glutamate molecules), which along the osmolarity gradient contribute to the movement of fluid from the interstitium into the intracellular space. That is, during this phase, cerebral edema is formed due to the trans-epithelial flow of sodium from the vascular bed, along with which chloride ions (to maintain electroneutrality) and water (to maintain osmoneutrality) move. At this stage, there is only a functional impairment of the permeability of the anatomically intact blood-brain barrier. At the same time, against this background, conditions are formed that contribute to the development of the next stages of cerebral edema (in particular, a drop in the concentration of interstitial sodium). The stage of cytotoxic edema does not lead to an increase in the volume of brain tissue and intracranial hypertension.
Developing vasogenic edema is characterized by more pronounced disturbances in the homeostasis of the interstitial space, which leads to disruption of the function/activity of neurons. As a result of increased permeability of the BBB, water accumulates in the intercellular space, which provokes the development of hypoxia and causes a malfunction of the cellular ion pumps of the brain, leading to the passive penetration of sodium ions into the cell, followed by water (the process of cell swelling).
The accumulation of fluid in a limited space according to the Monroe-Kelly formula leads to an increase in intracranial pressure , and in damaged glia (due to edema) the processes of exchange/capture of transmitter amino acids are disrupted. With the development of severe intracranial hypertension, it leads to displacement of the cerebral structures of the increased volume of the brain with herniation of the cerebellar tonsils/stem parts into the foramen magnum. And further compression of blood vessels further aggravates microcirculatory disorders/ischemia of brain cells. Dysfunction of the cardiovascular/respiratory/thermoregulatory centers located in the brain stem is a common cause of death.
As endothelial dysfunction progresses, it is accompanied by pronounced necrosis of epithelial cells and a sharp increase in the size of the intercellular space, which facilitates the passage of blood cells and leads to hemorrhagic saturation of brain tissue, which causes severe disruption of interstitial homeostasis, incompatible with the functioning of neurons and the development of hemorrhagic necrosis , which is associated with severe outcome of cerebral edema. The figure above shows the pathogenesis of cerebral edema.
Questions and answers
What causes pulmonary edema?
There are dozens of factors that contribute to the development of this pathology. They are associated with other diseases of different body systems. Clinical recommendations for pulmonary edema are largely determined by the situation.
Can pulmonary edema lead to death?
Yes, the risk of death in the case of such a pathology is very high, and for the fulminant form it is the only possible outcome of events. This is an extremely dangerous condition that requires immediate professional help.
How to treat pulmonary edema?
This is done exclusively in medical institutions, most often in intensive care. Only doctors know everything you need to know about the symptoms and treatment of pulmonary edema in adults or children - the pathology cannot be eliminated without special knowledge and skills.
What are the features of pulmonary edema in children?
Unlike adults, this pathology occurs much less frequently in children due to other diseases. The underlying cause is usually allergies or exposure to toxins. Or the cause may be congenital anomalies of various body systems.
Classification
Due to the specific development of cerebral edema, 4 types are distinguished:
- Cytotoxic OGM - develops as a result of ischemia , hypoxia , exo/endogenous toxic effects on brain cells, causing changes in the permeability (osmoregulation) of cell membranes and dysfunction of glial cells (disorders of cellular metabolism). Cytotoxic edema is reversible within 6-8 hours due to reactivation of the ion pump, which is achieved by restoring cerebral blood flow.
- Vasogenic OGM is based on an increase in the permeability of the blood-brain barrier . Occurs perifocally in the area of ischemia , abscess , tumor, traumatic brain injury, surgery. The main role is played by the transition of fluid from the vessels to the white medulla. Due to the increase in capillary permeability, fluid partially passes from the vessels into the interstitial space), causing an increase in its volume.
- Osmotic OGM develops when the osmolarity of brain tissue increases without disrupting the blood-brain barrier. Occurs with metabolic encephalopathies , hypervolemia , drowning , inadequate hemodialysis and polydipsia .
- Interstitial OGM is the result of a rapid increase in ventricular pressure.
- It is formed when the walls of the cerebral ventricles sweat from the liquid part of the cerebrospinal fluid in the periventricular zone.
According to the degree of compensation there are:
- Compensated OGM (characterized by the absence of dislocation syndrome).
- Subcompensated OGM (characterized by the presence of dislocation syndrome in the absence of vital lesions of brain structures).
- Decompensated OGM (presence of dislocation syndrome and disturbances of vital functions).
The table below shows a general classification of OGM and characteristics of its forms.
Causes of head pain and facial swelling
The main cause of swelling is a violation of the outflow of fluid from the intercellular space, a slowdown in blood circulation. Mild swelling causes discomfort and headaches, and gradually decreases during the day. In severe stages, the contours of the face are deformed. The soft tissues acquire a dense consistency, the palpebral fissures narrow, which leads to a sharp deterioration in well-being. Laboratory tests and various diagnostic methods will allow you to determine the cause of edema - treatment is ineffective until an accurate diagnosis is made.
Physiological reasons
Facial swelling can also appear in the absence of various chronic diseases of internal organs. Violation of the daily routine, poor nutrition and other factors cause a deterioration in the outflow of fluid from soft tissues. There are several reasons that can trigger acute headaches and swelling, especially in the first half of the day:
- sleep disturbance, night work, lack of sleep;
- following strict diets;
- use of inappropriate cosmetics for facial skin;
- unhealthy diet, eating foods with a lot of salt and spices;
- sleeping on a large and high pillow - this causes poor circulation in the neck.
If you normalize sleep and nutrition principles, swelling will go away over time. However, the tendency for them to appear remains, so it is important to follow a daily routine. Doctors also recommend drinking plenty of fluids during the day, and before going to bed, eating only light foods with a small amount of salt and spices. This will help maintain fluid balance and speed up blood flow. If swelling appears, it is useful to massage the face and apply a cooling compress.
Endocrine system diseases
Hypothyroidism is a disease of the thyroid gland in which a reduced amount of iodine-containing hormones is recorded in the blood. These include thyroxine and triiodothyronine. These substances are necessary for the proper functioning of metabolism, the absorption and processing of fats, maintaining stable cholesterol levels, and the functioning of the reproductive system. With hypothyroidism, these functions are impaired. There are several types of hypothyroidism. For effective treatment, it is important to determine its exact cause. It can be associated both with insufficiency of the thyroid gland and with disruption of the pituitary gland and hypothalamus, the organs that control it. In addition, hypothyroidism can develop when there is insufficient intake of iodine into the body from food - this is typical for regions where it is practically absent in the soil and drinking water. The following symptoms are characteristic of this disease:
- disruption of the digestive tract, increased appetite or lack thereof, rapid weight gain;
- chronic fatigue and drowsiness during the day, deterioration of memory and concentration;
- pain and aches in the joints, deterioration in the quality of skin, hair and nails;
- swelling of the face, arms and legs, especially in the first half of the day.
Swelling with hypothyroidism may be minor, but in advanced cases the face becomes significantly deformed. Soft tissues acquire a dough-like consistency, and when pressure is applied to them, marks remain. This symptom, like the others, goes away with normalization of hormonal metabolism and replenishment of the concentration of iodine-containing hormones.
Allergy
An allergy is an increased sensitivity of the immune system to certain irritants. They pose no danger to the body, but are recognized as foreign and therefore trigger an immune response. These compounds can enter the body through the air or food, as well as through the skin. Allergies are often caused by plant pollen, animal hair, certain foods, household chemicals and cosmetics, as well as any other environmental substances. A typical manifestation of an allergic reaction is swelling of the mucous membranes and subcutaneous tissues, headaches, and skin rash. There are several main manifestations of allergies, which can occur independently or be combined with each other:
- urticaria - a small rash on the skin and swelling, most often occurs in response to contact of an irritant with the skin;
- contact dermatitis – in the facial area it is often an allergy to cosmetics, after application of which a rash and swelling appears;
- atopic dermatitis is a childhood form of an allergic reaction, which is manifested by swelling, itching and soreness, the appearance of a rash and small blisters;
- bronchial asthma is a chronic disease that can be aggravated by frequent inhalation of polluted air, as well as when allergens (dust, pollen, wool particles) enter the respiratory tract.
The greatest danger is Quincke's edema. It develops at lightning speed, the contours of the face change shape in just a few minutes. This symptom can develop independently or represent one of the stages of anaphylactic shock. In addition to the soft subcutaneous tissues, the mucous membrane of the larynx swells, resulting in impaired respiratory function. In this condition, a person needs urgent medical attention , since swelling is dangerous due to complete closure of the airways. The basis of treatment is antihistamines, which reduce sensitivity to the allergen and relieve the manifestations of an allergic reaction.
Kidney diseases
The appearance of edema is one of the characteristic signs of kidney disease , and they can also appear in the facial area. They are soft, mobile, and when you press on them, no marks remain. The skin in the area of edema does not become bluish - it remains pale and may also acquire a yellowish tint. Their appearance is associated with impaired blood filtration and increased capillary permeability, as a result of which the amount of protein in the blood decreases. There are several kidney diseases that can cause swelling in the face and headaches:
- glomerulonephritis is an inflammatory disease in which periods of exacerbation and remission alternate, and can be treated in the initial stages;
- Kidney amyloidosis is a chronic metabolic disorder in which an increased concentration of protein is detected in the urine;
- nephropathies are non-inflammatory diseases that may be associated with long-term use of medications, acute infectious processes, radiation or chemotherapy;
- chronic renal failure - deterioration of kidney function, which develops slowly over several years or more;
- kidney damage in various systemic diseases, including diabetes mellitus, systemic lupus erythematosus and others.
In the initial stages of kidney disease, morning puffiness under the eyes may be the only symptom. They go away during the day or with cold compresses, so they are not a cause for concern. However, then other symptoms of nephritis, nephropathy or kidney failure develop: lower back pain, pain when urinating, the appearance of blood in the urine. The swelling becomes large and mobile, changing location when turning over to the other side. They can be localized on the extremities, along the veins, as well as on the abdominal wall. They resolve after comprehensive treatment and support of kidney function.
Diseases of the heart and blood vessels
Cardiac edema often differs from renal edema in appearance and consistency. They most often appear on the lower extremities, but in some patients they also occur in the face. They are denser, colder, and the skin at the site of their appearance often acquires a bluish tint. This symptom is characteristic of cardiomyopathies, sclerotic changes, congenital and acquired heart defects, arrhythmias, chronic hypertension, amyloidosis and other cardiac disorders. It is also important to pay attention to additional symptoms:
- headaches and dizziness, weakness during the day;
- increase or decrease in blood pressure;
- chest pain;
- uneven pulse, including skipping heartbeats, fastening or slowing down.
Cardiac edema slowly resolves. To get rid of them, comprehensive treatment of the underlying disease and supportive therapy for the heart are carried out. In the absence of medical attention, swelling will increase. The accumulation of fluid and the deterioration of its excretion increase the load on the myocardium, which is dangerous due to exacerbation of diseases. As maintenance therapy, diuretics (diuretics) are prescribed, which stimulate the removal of excess fluid from the body in a natural way.
Intoxication
Toxins enter the human body every day. They are found in large quantities in the polluted air of large cities and industrial enterprises, as well as in drinking water and products. Their presence has a detrimental effect on the state of the lymphatic system, making it difficult to remove excess fluid. This leads to swelling under the eyes in the morning and chronic headaches. In some cases, poisoning causes rapid swelling of the tissues in the facial area. This may be due to a number of violations:
- bites of poisonous insects - the cause of acute pain, severe swelling, headache, a sharp deterioration in health and an increase in body temperature;
- consumption of alcoholic beverages - ethanol is a toxin that makes it difficult to remove fluid and can also affect the condition of blood vessels, internal organs and the brain;
- smoking is another cause of intoxication;
- consumption of toxic substances or their entry into the body through the skin or respiratory tract - some of them have a nephrotoxic effect and adversely affect the functioning of the kidneys (vinegar in high concentrations).
Alcoholism is a chronic disease characterized by swelling in the facial area. They can have a neutral, purple or yellow tint, and intensify in the morning or after drinking alcohol. Headaches are caused by the toxic effects of ethyl alcohol metabolism products on the nervous system and brain.
Causes
The causes of cerebral edema are quite numerous, according to which cerebral and extracerebral causes of AMS are distinguished.
Cerebral causes of cerebral edema:
- Brain injuries ( subdural hematoma , brain contusion , basal skull fracture , diffuse axonal injury , intracerebral hematoma ), brain surgery.
- Primary brain tumors ( glioma , medulloblastoma , astrocytoma , hemangioblastoma , etc.) or metastatic lesions of brain tissue that promote displacement of brain structures/disturb the process of outflow of cerebrospinal fluid.
- Cerebrovascular accidents - against the background of arterial hypertension (with a stroke of ischemic / hemorrhagic origin ) or systemic atherosclerosis .
- Neuroinfections ( encephalitis , bacterial meningitis ), purulent processes of the brain (for example, subdural empyema ).
Extracerebral causes:
- Infectious diseases ( influenza , scarlet fever , measles , scarlet fever , toxoplasmosis , mumps , etc.).
- Poisoning with drugs (quinine, antidepressants, neuroleptics, antihistamines, etc.) or various neurotoxic poisons (cyanides, phenols, gasoline, etc.).
- Radiation exposure.
- Development of an allergic reaction ( anaphylactic shock , Quincke's edema ).
- Encephalopathy due to liver/ renal failure , diabetes mellitus , alcohol poisoning.
- A sharp climb without the required acclimatization (mountain edema).
In newborns, cerebral edema can be caused by intracranial birth trauma, severe toxicosis of the pregnant woman, prolonged labor, or entanglement of the umbilical cord.
Cerebral edema in newborns
The relationship between brain tissue and the cranial cavity in newborns is structured completely differently than in adults. This is due to the characteristics of the developing organism and age-related changes in the nervous system. In newborns, cerebral edema is characterized by lightning-fast progression due to imperfect regulation of vascular tone, liquor dynamics, and maintaining intracranial pressure at a stable level. The only thing that saves a newborn is the peculiarities of the joints of the skull bones, which are represented either by soft cartilaginous bridges or are located at a distance from each other (large and small fontanelles). If not for this anatomical feature, any cry of the child could result in the development of compression of the brain and its swelling.
Causes
In newborns, the causes of cerebral edema can be:
- Intrauterine hypoxia of any origin;
- Difficult childbirth and birth trauma;
- Congenital malformations of the nervous system;
- Intrauterine infections;
- Meningitis and meningoencephalitis as a result of infection during or after childbirth;
- Congenital tumors and abscesses of the brain.
Symptoms of cerebral edema in newborns
You can suspect cerebral edema in a newborn based on the following manifestations:
- Restlessness and loud crying;
- Lethargy and drowsiness;
- Breast refusal;
- Tension or swelling of the large fontanel when the child is at rest;
- Vomit;
- Convulsive seizures.
Characterized by a very rapid increase in symptoms and a progressive deterioration in the general condition of the child. In many cases, cerebral edema in newborns cannot be reversed and ends in death.
The presence of risk factors for the development of cerebral edema in a newborn is a reason for clinical observation by specialized specialists. Such a child must be examined by a pediatric neurologist to exclude any signs of intracranial pathology. Mothers should be very attentive during the month after giving birth and respond to any changes in the child’s behavior!
Symptoms
Symptoms of cerebral edema in adults are extremely variable and are caused by dysfunction of various brain structures, disorders of metabolic processes/microcirculation and a developing increase in the volume of brain tissue, especially accompanied by displacement/herniation of certain brain structures, disruption of cerebrospinal fluid dynamics/blood flow in the vessels of the brain. The localization of edema in areas of the brain also plays a significant role, which determines its effect on specific brain structures and forms, in addition to general cerebral symptoms, focal neurological symptoms depending on the affected brain structures. Clinical symptoms of cerebral edema vary significantly depending on the stage of its development, according to which the following are distinguished.
General cerebral syndrome
Clinical signs at this stage are caused by an increase in ICP (intracranial pressure), and their manifestations/severity are determined by the rate of its increase.
headache appears vomiting may occur , often without preceding nausea. The intensity of pain after vomiting usually decreases. Transient dizziness . A common symptom is congested optic discs/transient episodes of visual impairment. Changes in the cardiovascular system are noted: bradycardia , increased systolic blood pressure, decreased breathing (the so-called “Cushing triad).” Characterized by slowly increasing changes in the psyche according to the type of disinhibition: irritability, anxiety, moodiness. Objective symptoms of intracranial hypertension with a slow increase in ICP are congestion of the veins/swelling of the optic disc, radiographically - thinning of the bones of the cranial vault, osteoporosis of the sella turcica.
With a rapid increase in ICP, severe pain of a paroxysmal/paroxysmal nature appears, often bursting pain, accompanied by vomiting, which does not bring relief with the subsequent development of coma . Bradycardia , oculomotor disorders appear Against the backdrop of ICP progression, mental inhibitions are noted, which is manifested by decreased memory, severe drowsiness , non-communication of the patient, and slower speech/thinking.
Syndrome of rostrocaudal diffuse increase in neurological symptoms
Clinical signs of cerebral edema at this stage are determined by the gradual involvement of certain brain structures in the pathological process. As a rule, the pathological process first involves the cortical, later the subcortical, and ultimately the structures of the brain stem. Edema of the cerebral hemispheres is characterized by impaired consciousness and the appearance of generalized clonic seizures.
The spread of the process to the subcortical/deep structures of the brain occurs with psychomotor agitation, the development of grasping/protective reflexes, hyperkinesis , and an increase in epileptic paroxysms .
When the pathological process moves to the hypothalamic region/upper parts of the brain stem, the degree of impairment of consciousness increases sharply, manifesting as coma / stupor with initial manifestations of impaired breathing and function of the cardiovascular system. A posture of decerebrate rigidity (installation of the limbs in an extension position). The convulsions are of a stem nature ( opisthotonus / hormetonia ), mydriasis (dilated pupils) with a sluggish reaction to light is noted.
Swelling of the tegmentum of the cerebral pons causes specific breathing disorders in the form of periodic breathing, maximum bilateral miosis (constriction of the pupils), truncal gaze paresis and leads to the disappearance of the oculovestibular/oculocephalic reflexes. As the edema moves to the medulla oblongata (lower part of the brainstem), disturbances in vital functions increase, which is manifested by a slower pulse/decreased blood pressure and breathing. Neurological examination reveals areflexia of deep reflexes , diffuse muscle hypotonia , lack of pupillary response to light, immobility of the eyeballs.
Phase of dislocation of brain structures
It is based on the process of dislocation and temporo-parietal/occipital herniation of brain structures, which is manifested by characteristic focal symptoms, the main of which are brainstem symptoms ( bradycardia , decerebrate rigidity , dysphagia etc.) with damage to the oculomotor nerves ( mydriasis , ptosis , divergent strabismus ). Often there is sudden vomiting, stiffness of the neck muscles, convulsions of the extensor muscles, lack of pupillary response to light, a decrease in body temperature, a decrease in heart rate and the development of life-threatening conditions - a sharp drop in blood pressure, depression of consciousness (coma), breathing disorders (cessation).
The particular danger of displacement/herniation of supratentorial structures is determined by the high risk of developing vascular disorders and occlusion of the cerebrospinal fluid outflow pathways, which sharply intensifies the primary pathological processes, which turn from potentially reversible disorders into irreversible ones.
Brain swelling
What is cerebral edema -
Cerebral edema is a condition of the brain that occurs under the influence of certain infections or excessive stress, develops rapidly, at an equally rapid pace and disappears if adequate measures are taken.
Typically, to eliminate cerebral edema, you need to remove excess fluid or apply ice as quickly as possible. Also, cerebral edema is a condition that in some cases is caused by infectious diseases or injury, then treatment is delayed. Brain swelling is also known as “cerebral edema,” another name is “increased intracranial pressure.”
With the development of this condition, pressure rises inside the skull, which leads to cerebral circulation disorders. If this process continues for a certain period of time, brain cells begin to die. The consequences can be the most tragic.
What provokes / Causes of cerebral edema:
Among the most typical causes of cerebral edema are:
- infectious diseases
- traumatic brain injury
- brain tumor
- a disease that causes problems with brain function
- hemorrhage inside the skull
If a traumatic brain injury occurs, mechanical damage to the brain occurs. In some cases, fragments of crumbled or broken bone enter the brain. Then cerebral edema forms, and obstacles begin to interfere with the normal outflow of fluid from the brain tissue.
When might such a situation happen?
- work injury
- car accident
- strong head blow
- injury from extreme sports
- falling from height
- assault causing grievous bodily harm, etc.
The blood vessels become clogged with blood clots, causing a cerebrovascular accident called an ischemic stroke. As a result, cerebral edema occurs in children or adults. The result of a stroke is a lack of oxygen in brain cells, which leads to their starvation and, as a result, death.
infectious diseases most often cause cerebral edema :
Inflammation begins in the lining of the brain under the influence of a virus or certain medications.
Inflammation caused by a virus begins in the brain. Viruses that cause encephalitis in humans are transmitted mainly by insects.
This is an infectious disease caused by the protozoan organism Toxoplasma.
- Subdural empyema
This is a brain infection with a purulent complication.
In some cases, swelling is caused by a tumor in the brain . The cells grow quite quickly and begin to put pressure on normal brain cells. In newborns, cerebral edema is diagnosed as a result of trauma received during birth. Also, in some cases, the diagnosis in question is provoked by illnesses the mother suffered during pregnancy.
The so-called mountain cerebral edema occurs in climbers when they climb mountains above 1.5 km. The reason in these cases is a sharp change in altitude, which is abnormally tolerated by the human body, causing various disorders.
Rarely, but still, the cause of cerebral edema can be alcoholism. A person becomes addicted, called withdrawal syndrome. Vascular permeability increases sharply, and the electrolytic balance in the body is disrupted. The cardiac and respiratory centers are affected. This can be fatal; such cases have occurred in clinical practice in our country and abroad.
Pathogenesis (what happens?) during cerebral edema:
To date, researchers have clearly identified the main mechanisms of brain dysfunction during brain swelling. The brain becomes larger in volume, but the intracranial space cannot increase, which causes a mass effect. Secondary damage occurs—compression of the brain. Accordingly, an increase in intracranial pressure, a decrease in cerebral perfusion pressure is recorded, and blood circulation in the brain is disrupted. This means that cerebral ischemia has occurred. The metabolism of its tissue switches to the anaerobic type.
The following factors play a role in the pathogenesis of the disease in question: :
- vascular
- circulatory
- tissue
Vascular factor means a violation of vascular permeability, which causes the penetration of blood plasma components and proteins into the brain tissue. As a result, the osmolarity of the intercellular fluid increases and cell membranes are damaged.
Researchers divide the circulatory factor An increase in blood pressure and dilation of the arteries of the brain cause a significant increase in pressure in its capillaries. Water is filtered from them into the intercellular space, resulting in tissue damage. The second link is damage to tissue elements; there is a tendency to accumulate water due to insufficient blood supply to the brain.
The concept of the pathogenesis of cerebral edema was presented in the form of a progression model according to the fundamental concept of Monroe-Kelly, which states that there is a connection between the components of the rigid skull (blood, brain, cerebrospinal fluid). That is, if one of the components increases, then the others decrease in the same proportion, this allows the body to maintain normal pressure inside the skull.
In an adult man or woman, the pressure inside the skull in the supine position ranges from 3 to 15 mmHg. It can reach 50–60 mmHg. if there are such factors:
- sneezing
- cough
- sharp rise in intra-abdominal pressure
Such fluctuations do not last long, and therefore do not cause disturbances in the human central nervous system.
Intracranial pressure refers to the uniformly distributed pressure in the cranial cavity. In an adult, the brain and the tissues surrounding it have a certain constant volume, which is limited by the rigid bones of the skull. The contents of the cranial cavity are conventionally divided into 3 parts:
- brain parenchyma,
- liquor,
- intravascular volume of arterial and venous blood
Of 100% of the intracranial volume, 80–85% is brain matter. Liquor takes up 5–15%, and blood accounts for 3–6%.
Degrees of intracranial hypertension:
- I – pressure inside the skull is increased from 15 to 20 mm Hg;
- II – 20-40 mmHg;
- III – from 40 mm Hg.
At each stage of progression of intracranial hypertension there is a corresponding mechanism of the cerebral protection system. The complex of compensation mechanisms is determined by the ability to adapt to an increase in the volume of the craniospinal system.
Cerebral edema in adults and children is divided according to the pathogenetic mechanism into the following types: :
- cytotoxic
- vasogenic
- interstitial
- osmotic
The most common is the vasogenic type . which appears when the function of the blood-brain barrier is impaired. The pathogenesis is dominated by the release of plasma into the extracellular space and an increase in the volume of the white matter of the brain. When a person has suffered a traumatic brain injury, swelling can form within 24 hours. It develops around abscesses, tumors, surgical sites, areas of inflammation, and ischemic areas. This swelling is perifocal. It can lead to compression of the brain.
The cytotoxic species results from hypoxia. ischemia and intoxication. It occurs inside cells due to disturbances in astroglial metabolism. A disorder of osmoregulation of brain cell membranes, which depends on the sodium-potassium pump, is recorded. Edema is mainly observed in the gray matter of the brain. It can result from toxic-hypoxic encephalopathy, viral infections, carbon monoxide poisoning, ischemic stroke, poisoning of the body with hemoglobin breakdown products or cyanide.
The osmotic appearance results from hyperosmolarity of brain tissue when the functionality of the blood-brain barrier is not impaired. This happens when:
- drowning in fresh water,
- metabolic encephalopathies,
- improper hemodialysis,
- polydipsia,
- hypervolemia.
Interstitial OGM becomes a consequence of water permeating through the walls of the lateral ventricles into the brain tissue and develops around them.
Factors in the development of cerebral edema . allocated in 1979 by WF Ganong and team:
- increase in filtration pressure
- positive water balance
- increasing capillary permeability
- decrease in the osmotic pressure gradient between the blood and the intercellular environment
- disturbance of the nervous and humoral regulation of water and electrolyte metabolism
- violation of lymph outflow
Damage to the vascular endothelium is important in the pathogenesis of AGM. The endothelium has a high level of metabolism; it plays an important role in the system of homeostasis processes. Cerebral edema is divided into local or generalized according to its prevalence. In the local form, processes occur in a small area of the brain, and in the generalized form, even 2 hemispheres can be completely covered.
Pathological picture of cerebral edema
Brain specimens from AGM have characteristic pathological changes. Macroscopically, the following changes are observed: brain moisture, clouding of the surface of the hemispheres, unclear boundaries between the gray and white matter on the section.
With severe edema, the volume of the brain increases, which leads to a displacement of its areas under the falciform process of the dura mater, the tentorium of the cerebellum, or into the foramen magnum; strangulation impressions appear in the corresponding zones. There is flabbiness of the brain tissue; on the section it is too moist; swelling of the pia mater and local plethora are recorded. A clear liquid drains from the surface of the meninges. When swelling occurs, the density of the brain substance increases and it becomes dry.
Symptoms of cerebral edema:
Typical symptoms include severe headaches. A person can take painkillers, which provide a short-term effect, and then the pain begins again. This is a bad sign that you should pay attention to, especially if this has not happened before or you have recently suffered a head injury. Typical symptoms of cerebral edema include nausea and/or vomiting, as well as dizziness.
A person's vision is usually impaired, as is orientation in space. You may notice that the person begins to walk unevenly, cannot confidently turn around his axis - he looks as if he is “lost in space.” Breathing becomes uneven. One minute a person can take deeper breaths, and the next minute the breathing becomes barely audible, shallow. The interval between inhalations is constantly changing.
A typical symptom of cerebral edema in children and adults is difficulty speaking and stupor. If you are not aware of other symptoms, this manifestation may appear as a mental disorder. Also, cerebral edema is characterized by loss of consciousness, short-term convulsions and forgetfulness. If you notice two or more of the above listed and described symptoms in yourself or someone else, this is a reason to immediately consult a doctor. Edema is diagnosed using MRI and CT; more details about the diagnosis will be written below. The cause of the disease can be determined by conducting a laboratory blood test.
Cerebral edema: consequences
Typical consequences include:
- absent-mindedness
- sleep disorders
- frequent headaches
- physical activity disorder
- failure of communication skills
- depressive state
The outcome and course of the disease depend on what measures were taken and at what time. Brain edema is a dangerous condition that can cause a malfunction of the centers responsible for blood dynamics, respiratory processes, heart activity, etc. A weak supply of oxygen to the brain leads to damage to its cells. If brain tissue has died, then any therapy will not help it recover. Due to increased ICP, a person’s body is paralyzed, which leads to disability.
An increase in herniation and subsequent swelling can lead to falling into a coma and complete cessation of breathing. If important brain centers are affected, the result is death of the patient. With slight swelling of the brain, the symptoms may go away on their own, or the disease can be cured quite quickly.
Diagnosis of cerebral edema:
The choice of diagnostic methods depends on the manifested symptoms and preliminary diagnosis. Often used:
- Neurological examination
- Examination of the cervical spine
- MRI of the brain
- CT scan of the brain
- Blood test (finding out the causes of edema)
Treatment of cerebral edema:
Mountain and minor swelling may go away on its own in 2-4 days. In other cases, qualified medical assistance is required. To supply the brain with oxygen, medication and surgery will be needed.
Modern therapeutic methods for cerebral edema:
- Infusion of intravenous medications
- Oxygen therapy
- Taking special medications
- Reducing body temperature (today the method is losing its relevance)
- Ventriculostomy - drainage of cerebrospiral fluid from the ventricles of the brain using a catheter - helps reduce ICP
The operation is needed for the following purposes:
- remove the cause of edema (eliminate a neoplasm, restore a damaged vessel, etc.)
- remove a fragment of skull bone, which reduces the pressure inside the skull
Prevention of cerebral edema:
You need to follow safety rules in everyday life:
- Everyone in the car must wear seat belts
- When riding a bicycle, skateboard, or rollerblades, you must wear a helmet
- When performing construction work where there is a risk of head injury, you must wear a helmet and follow special safety precautions
- get rid of bad habits
- control and normalize blood pressure
- When climbing mountains, you need to allow time for acclimatization to the altitude
Which doctors should you contact if you have cerebral edema:
Tests and diagnostics
Cerebral edema is an urgent condition that requires urgent medical care in a hospital setting (intensive care/resuscitation department), therefore, the initial diagnosis of acute brain injury should be as fast as possible and carried out during treatment. The primary guideline for diagnosing AGM is clinical symptoms, however, it must not be forgotten that at this stage they can be minimally pronounced. If OGM is suspected, a neurological/ophthalmological examination is carried out, during which pain, verbal-acoustic, behavioral reactions, ocular/pupillary reflexes, the condition of the optic nerve head, and intraocular pressure indicators are assessed. A clinical/biochemical blood test and lumbar puncture are required.
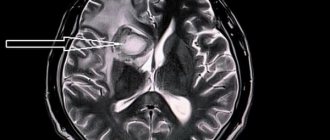
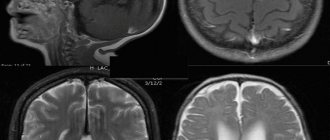
The main methods of instrumental diagnostics are computed tomography and nuclear resonance imaging, which allow one to visualize the localization/extension of the area of hyperhydration and identify signs of compression syndrome. According to indications, ultrasound of the skull in different projections, echoencephalography/electroencephalography, neuroophthalmoscopy, and cerebral angiography can be performed.
Differential diagnosis is carried out with thromboembolism of cerebral vessels , metabolic disorders , and status epilepticus .
Diagnostics
If the symptoms of pulmonary edema are not pronounced, additional studies are required in parallel with emergency care:
- biochemical screening. This is a blood test;
- study of blood gases;
- ECG, ultrasound of the heart;
- X-ray of the chest area;
- pulmonary artery catheterization.
In many cases, diagnosis of pulmonary edema is possible immediately - only based on the signs that appear visually in the patient and without additional examination.
Diet
Nutrition in the first 1-3 days of AGM is carried out parenterally, for which protein hydrolysates, glucose solutions, amino acids, plasma, albumin, a complex of vitamins, and special nutritional mixtures are administered. The timing of the start of enteral nutritional support through a tube is determined depending on the patient's condition, however, to restore gastrointestinal motility, it should begin as early as possible. For this purpose, special quickly digestible high-calorie nutritional mixtures are used, enriched with vitamins/microelements, a set of essential/essential amino acids in optimal dosages ( Nutrizon Energy , Nutrizon , Berlamin , Nutrizon Protein , etc.). It is recommended to use highly concentrated mixtures to reduce the volume of fluid administered, but at the same time provide the body with the necessary amount of calories. The patient can begin eating by mouth after regression of brain disorders.
Causes of pulmonary edema
A mixture of edematous fluid (transudate) and a liquid substance that “lines” the alveoli of the lungs from the inside (it is called “pulmonary surfactant”) enters the lumen of the alveoli, where it combines with air. This leads to the formation of foam, which creates an obstacle to the flow of oxygen. Lack of oxygen provokes the development of shortness of breath, due to which the pressure inside the chest decreases and blood flow to the right side of the heart increases.
Pulmonary edema causes infiltration of the alveoli and is manifested by symptoms that indicate oxygen starvation, which is dangerous for tissues. The patient requires emergency care due to the high risk of death due to suffocation.
Prevention
There is no specific prevention of cerebral edema, since it develops secondary. Among the general recommendations, we can only cite the need to follow some rules:
- Minimize the risk of head injury: use protective devices when moving (protective helmet when rollerblading/biking/skating, skiing; seat belts when driving in a car, do not jump your head into a body of water, etc.).
- Treat infectious/somatic diseases in a timely manner.
- Monitor your blood pressure .
- Lead a healthy lifestyle.
- When climbing to altitude (mountains), do not forget about the need to acclimatize to the altitude.
Prevention of strokes
Hereditary predisposition to stroke, the presence of cardiac diseases, pathology of blood vessels and blood composition, age over 40 years, obesity and diabetes require a number of preventive measures:
- Maintaining normal blood pressure, taking antihypertensive drugs as prescribed by a doctor, monitoring blood pressure.
- Maintaining a normal level of physical activity, exercise, walking 30-40 minutes a day (for example, walking the dog).
- Conducting preventive examinations, including a standard set of laboratory parameters. During a preventive examination, the following tests are additionally required: gene diagnosis of CADASIL syndrome using the PCR method, plasma factors of the blood coagulation system, antibodies to prothrombin of the IgG and IgM classes to determine the risk of thrombosis, determination of polymorphisms associated with the risk of arterial hypertension, diabetes mellitus, lipid disorders exchange, in order to identify a predisposition to diseases that increase the risk of stroke, von Willebrand factor (a glycoprotein that ensures the formation of blood clots), complex laboratory tests for preclinical diagnosis of cardiovascular diseases are offered (“ELI-ANKOR-Test-12”, “Cardiorisk”).
- Avoiding chronic and acute stress, maintaining mental hygiene.
- Normalization of weight (BMI <25 kg/m2).
- Healthy eating (for example, Mediterranean diet, limiting salt to 5 5 g/day).
- Quitting smoking and taking psychoactive substances.
- Treatment of diseases that are a risk factor for stroke [8, 11].
Consequences and complications
The consequences of cerebral edema, even in cases of rapid relief, can manifest as long-term consequences (absent-mindedness, disturbances in sleep/motor activity, communication abilities, depression). In severe cases, the consequences of cerebral edema can develop in the form of:
- decerebral syndrome (characterized by persistent extensor muscle rigidity, strabismus, severe mental defect);
- decortication syndrome (characterized by impairment/disappearance of speech, motor and mental skills;
- posthypoxic encephalopathy (characterized by dysfunction of the cortex with the development of a cerebral intellectual-mnestic defect).
The most severe complication is death from cerebral edema.
Consequences of a stroke
There are transient ischemic attack (less than a day), minor stroke (from 1 day to 3 weeks) and stroke with persistent residual effects. The consequences of a stroke are expressed mainly in motor and sensory disorders, the formation of muscle contractures (pronounced constant restriction of movements in the joints), speech and swallowing disorders. General symptoms may also remain, including confusion, disturbances in thinking, will, and emotional regulation. Complications can develop: from epilepsy to bedsores, encephalopathy and anxiety-depressive syndrome [1, 3].
Forecast
The prognosis for acute hypertension can vary significantly depending on its etiology, severity, localization, level of intracranial hypertension , and the presence of brain dislocation. Brain edema in the initial stage is a reversible process; as it increases, neuronal death/destruction of myelin fibers develops, leading to irreversible changes in brain structures.
However, even in surviving patients after cerebral edema, in the vast majority of cases there are residual effects, which can vary significantly from subtle manifestations in the form of increased intracranial pressure , frequent headaches , forgetfulness, irritability, absent-mindedness, depression , sleep disturbances, emotional disorders, slowness intellectual processes) to severe disorders of motor/cognitive functions, mental sphere, leading to the patient’s disability.
Severe complications develop especially often during stroke and coma . Accordingly, the prognosis for cerebral edema after a stroke, like the prognosis for coma, is disappointing, at best with disability due to impaired coordination/motor disorders and mental disorders, at worst the patient’s death occurs. Mortality rates for cervical edema, depending on the etiology and severity, vary between 35-70%.
Cerebral edema in alcoholism: methods of treatment and prevention
Contents: [hide]
Alcoholism is a disease that leads to very unpleasant consequences. But not everyone knows their seriousness.
Alcohol abuse causes many pathologies in the body.
Among them is cerebral edema. This disease is accompanied by the accumulation of large amounts of fluid in all tissues and cells of the brain.
Causes of cerebral edema
Every disease appears for some reason. This also applies to the brain. Symptoms of the occurrence and development of cerebral edema appear for the following reasons:
- Trauma to the skull in the form of a fracture of its base. This can happen in accidents with head injuries, falls, blows. Edema occurs as a result of injuries to the brain from bone fragments.
- Brain hemorrhage.
- Some infectious diseases.
- Encephalitis and viral infections with inflammatory processes.
- Purulent formations inside the membrane of the brain.
- Diseases that block the supply of oxygen to brain cells.
- Sudden changes in altitude.
- Alcohol abuse.
A brain tumor must be treated immediately after it occurs. The slightest symptom is a reason to consult a doctor. Lost time can lead to death. The best way to prevent the disease is to completely abstain from drinking alcohol.
Signs of a brain tumor
Swelling of the brain occurs suddenly. Its signs:
- Pain in the head.
- Pain in the cervical region, numbness of the skin.
- Vomit.
- Frequent nausea.
- Breathing disorders.
- Dizziness.
- Visual impairment.
- Memory loss (partial or complete).
- Impaired balance and gait (ataxia).
- Cramps, sometimes severe.
- Speech difficulties.
- Loss of consciousness.
- Decreased consciousness – stupor.
- Intracranial pressure is increased.
- Partial paralysis of the body.
- Some fundus changes.
- Pupil dilation.
- Slow heart rate.
- Drowsiness.
These symptoms manifest differently in each person. This depends on the stage of the disease and the characteristics of the body. Diagnosis of brain disease is carried out by electroencephalography, echoencephalography, pneumoencephalography and other methods.
Treatment of cerebral edema
It is impossible to cure cerebral edema at home. If signs of this disease appear, you should consult a doctor. Only a qualified specialist can make an accurate diagnosis and prescribe treatment. Delay often leads to death.
At best, a person remains disabled forever. Modern medicine can cure cerebral edema completely and relatively quickly. To treat brain pathology in alcoholism, various combinations of surgical methods and medications are used:
- Oxygen therapy is a very effective procedure. Through an inhaler, as well as with the help of other devices, a person breathes oxygen. This method enriches the blood with oxygen, and in this enriched form it enters the vessels of the brain.
- Intravenous infusion of drugs helps maintain normal blood pressure and blood flow in general, and helps the body fight infections.
- Ventriculostomy is an operation during which cerebrospinal fluid is sucked out of the brain and its ventricles. As a result, intracranial pressure decreases and the process of brain swelling stops.
- Hypothermia is the process of artificially lowering body temperature. The procedure is relatively new and not yet widely used. It significantly reduces the size of the brain tumor.
- Your doctor may prescribe medications to relieve swelling. They can be tablets and injections. But they will bring benefits only after recovery from alcoholism, since drunkenness and treatment of this disease are incompatible.
- Barbiturates help reduce swelling and reduce cramps.
- Drugs from the group of corticosteroids help restore blood flow in the area of edema.
Many other drugs are used for treatment. As a last resort, surgical intervention is used, as a result of which you can:
- restore blood vessels damaged by the disease;
- remove tumors;
- remove some fragments of the cranial bone to reduce intracranial pressure.
Typically, swelling of the brain develops very quickly, but goes away quite quickly with timely medical care. She should be contacted immediately after symptoms of the disease are noticed. This disease can occur as a result of head injuries, infectious diseases and other reasons.
Swelling may be complicated by bone fragments lodged in the brain. This happens as a result of road accidents, severe head injuries, and falls from a height. Swelling can be caused by encephalitis after bites of certain insects such as ticks, meningitis. Newborns can get it as a result of birth trauma. For climbers, it can occur as a result of changes in altitude. A common cause of edema is the consumption of large doses of alcohol. The consequences of edema can be very different:
- Sleep disturbance.
- Pain in the head.
- Absent-mindedness.
- State of depression.
- Impaired physical activity.
- Impairment (complete or partial) of communication abilities.
With alcoholism, which provokes cerebral edema, breathing and cardiac activity are impaired, and brain cells are affected. Dead cells are not restored. This can ultimately cause paralysis and disability, as well as respiratory arrest and death.
Swelling following a mild concussion may not require treatment. But in other cases, qualified assistance must be provided immediately. Among medications, furosemide can be prescribed for dehydration. panangin, potassium chloride and asparkam. Glycerol, mannitol, dexamethasone help. The doctor prescribes the use of various means depending on the individual characteristics of the patient and his condition. There are no universal recipes for treating a brain tumor.
To maintain the necessary water and electrolyte balance, an isotonic sodium chloride solution or a hypertonic glucose solution is prescribed together with potassium chloride.
Brain disease caused by alcohol addiction usually manifests itself in the following forms:
- Alcohol psychosis.
- Alcoholic encephalopathy and dementia.
- Convulsive seizures.
- Paroxysmal disorders.
- Cognitive dysfunction.
Disease prevention
You can prevent such a dangerous disease if you follow the simplest safety rules:
- You need to monitor your blood pressure and try to maintain it within normal limits.
- It is better to give up all bad habits, especially drinking alcohol.
- If possible, use protective equipment to protect your head from injury.
List of sources
- Pavlenko, A.Yu. Cerebral edema: conceptual approaches to diagnosis and treatment / A.Yu. Pavlenko // Emergency Medicine. - 2007. - No. 2 (9). — P. 11-15.
- Principles and methods of diagnosis and intensive therapy of cerebral edema and swelling: method. recommendations / V.I. Cherny [and others]. - Donetsk, 2003. - 49 p.
- Slynko E.I. Traumatic injuries of the spine and spinal cord / E.I. Slynko, A.N. Honda. - K.: PP Gamma-Print, 2010. - 288 p.
- Martynov V.A., Zhdanovich L.G., Karaseva E.A., Ageeva K.A., Khasanova L.A. Edema-swelling of the brain: tactics of patient management // Infectious diseases: news, opinions, training. 2018. – T. 7. – No. 1. – S. 124-13.
- Zadvornov A.A., Golomidov A.V., Grigoriev E.V. Clinical pathophysiology of cerebral edema. Part 2 // Bulletin of anesthesiology and resuscitation. – 2021. – T. 14. – No. 4. – S. 52-60.
Treatment of headaches and facial swelling
Treatment tactics will depend on the exact diagnosis. It will include drugs to eliminate the underlying cause of the disorders, as well as to symptomatically eliminate swelling. The doctor will prescribe a medication regimen, which may include the following steps:
- for diseases of the cardiovascular system - cardiac glycosides, drugs for vasoconstriction, adrenergic blockers and anticoagulants;
- kidneys and excretory system - antibiotics as necessary, supportive agents;
- for allergies - antihistamines and hormonal anti-inflammatory drugs;
- hypothyroidism - iodine preparations, as well as levothyroxine;
- intoxication - gastric lavage and infusion therapy may be necessary.
Diuretics are prescribed to remove excess fluid. They are used for diseases of the cardiovascular system and for slowing down lymphatic drainage. However, such measures are temporary, so it is important to choose an effective treatment regimen that will eliminate the main cause of edema.
What diseases are there a risk of edema?
Pathology indicates a complication of the underlying disease, increases its duration and worsens the prognosis of treatment. The most dangerous from the point of view of pulmonary edema include:
- Heart diseases. Respiratory failure often occurs against the background of pathologies of the heart and blood vessels. Cardiogenic pulmonary edema is a life-threatening complication that develops with myocardial infarction, aneurysm, endocarditis and myocarditis, severe hypertension, and pathological conditions caused by congenital or acquired heart defects.
- Pulmonary diseases. At risk are patients with injuries and severe diseases of the respiratory tract. Respiratory edema develops against the background of exacerbation of chronic bronchitis and bronchial asthma, tuberculosis, and lobar pneumonia. The risk is increased by tumor lesions of the lung tissue, pleurisy, and chest injuries, which are accompanied by pneumothorax. If a person is connected to a ventilator for a long time and receives a mixture with a high concentration of oxygen, this also leads to an imbalance of pressure in the pulmonary capillaries and the release of exudate.
- Infectious diseases. In severe cases or inadequate treatment of whooping cough, scarlet fever, influenza, diphtheria and other infectious diseases, edema develops, followed by acute pulmonary failure. In young children, this clinical syndrome can cause acute laryngitis and the proliferation of adenoids.
- Pathologies of intrauterine development and difficult childbirth. Severe pregnancy, prematurity, oxygen hypoxia, fetal bronchopulmonary dysplasia - these factors increase the risk of developing pulmonary failure in newborns. In pregnant women, pulmonary failure can develop due to eclampsia. The same phenomenon occurs with ovarian hyperstimulation syndrome against the background of stimulation of ovulation by hormonal drugs.
- Foreign bodies entering the respiratory tract. Mechanical asphyxia is one of the possible causes of acute respiratory failure. Pathology occurs when foreign objects enter the respiratory tract, after drowning or attempted hanging, or blockage of the respiratory tract with vomit.
- Diseases of the urinary system and gastrointestinal tract. Nephrogenic pulmonary edema can be complicated by acute inflammatory diseases, which are accompanied by renal dysfunction and the development of severe renal failure. In gastroenterology, patients with liver cirrhosis, severe pancreatitis, and intestinal obstruction have to deal with respiratory failure.
- Neurological diseases. Traumatic brain injuries, meningitis, encephalitis, neoplasms, cerebral hemorrhages, complications after brain surgery - all this leads to neurogenic pulmonary edema.
- Allergies, injuries, poisoning. Acute respiratory failure can be caused by the ingestion of various toxic substances into the body. Pulmonary edema is encountered by patients with alcohol and drug intoxication, poisoning with drugs, salts of heavy metals, and toxic gases. Pulmonary insufficiency is diagnosed in case of blood poisoning, burns with a large affected area, acute allergic reactions.
Predictions and prevention
Pulmonary edema is a deadly condition; Mortality with this clinical syndrome is up to 50%. Patients with anaphylactic shock most often develop fulminant or acute pulmonary edema, which in more than 90% leads to death.
The consequences of acute pulmonary failure are no less serious than the disease itself. Many patients who have suffered pulmonary edema experience ischemic damage to internal organs, the appearance of areas of pneumosclerosis, and congestive pneumonia. This affects the functioning of the respiratory system, in the organs of which irreversible changes occur. The pathology is manifested by shortness of breath, chest pain, and cough. Pneumosclerosis and other consequences of pulmonary edema require long-term treatment, can lead to disability and shorten the patient's life expectancy.
The likelihood of a favorable prognosis and outcome of the disease with pulmonary edema increases if the diagnosis was made in a timely manner and doctors began to stop the attack at the initial stage.