Pulmonary infarction - what is it?
According to statistics, pulmonary infarction accounts for approximately 10-25% of all cases of pulmonary embolism (PE).
Quite often the diagnosis is not made during the patient’s lifetime. The fatal outcome from the disease is recorded according to various sources in 5-30% of patients. The risk of death from pulmonary embolism increases if there is no proper treatment and there are concomitant background pathologies. It should be noted that infarction of the right lung is twice as common as that of the left. The lower lobes of the organ are affected four times more often than the upper ones.
Pulmonary infarction - classification of the disease
Depending on how strongly the lumen of the pulmonary artery is blocked by thromboembolism, the following types of pulmonary infarction are distinguished:
- Submassive thromboembolism (blockage at the level of segmental and lobar branches is diagnosed).
- Massive thromboembolism (thrombus blocks the main trunk or main branches of the pulmonary artery).
- Thromboembolism of small pulmonary arteries.
Pulmonary infarction can also be:
- primary (it is not known where the thromboembolus came from) and secondary (in addition to pulmonary embolism, the patient has venous thrombophlebitis);
- extensive (large area of damage) and limited (only subsegmental branches of the pulmonary artery are blocked);
- complicated (sepsis, hemoptysis, pleural empyema, abscess formation) and uncomplicated.
Hemorrhagic pulmonary infarction
Thromboembolism of the pulmonary arteries often leads to ischemia of the pulmonary parenchyma. As a result, the damaged lung tissue is filled with blood, which comes from areas with normal vascularization. A hemorrhagic pulmonary infarction develops.
At the site of inflammation, optimal conditions are created for the development of infection, which provokes the occurrence of symptoms of heart attack-pneumonia. If a branch of the pulmonary artery is blocked by an infected thrombus, destruction of the parenchyma is noted and a lung abscess is formed.
1.General information
According to the definitions existing in modern medicine, a heart attack is a rapid, one-stage focal necrosis (death, death) of a large number of parenchymal, i.e. the main, functionally specialized cells of any tissue or organ. The cause is ischemia, a pathological state of oxygen and trophic starvation due to a lack of blood supply. Outside of medicine, the most famous example of such a scenario is myocardial infarction, while in clinical practice, infarctions of the spleen, brain (stroke), kidneys and other organs are also encountered.
Due to the peculiarities of the anatomical structure and vasculature (blood supply) of the organs of the human respiratory system, pulmonary infarction in most cases develops on the right side and in the lower lobes.
A must read! Help with treatment and hospitalization!
Causes of pulmonary infarction
Most often, pulmonary infarction develops in people who suffer from diseases of the cardiovascular system:
- mitral stenosis;
- atrial fibrillation;
- coronary heart disease;
- myocardial infarction;
- infective endocarditis;
- cardiomyopathy;
- vasculitis;
- heart failure;
- atrial maxomas, etc.
In this case, blood clots form in the appendage of the right atrium and are carried with the blood flow into the arteries of the pulmonary circle.
Also, the causes of pulmonary infarction can be:
- thrombophlebitis of the deep pelvic veins;
- thrombosis of leg veins.
In these two diseases, floating thrombi that are attached to the distal part of the venous vessel are dangerous.
Other causes of pulmonary embolism include:
- fracture of tubular bones, due to which the patient is forced to remain in bed for a long time;
- caesarean section, natural childbirth;
- extensive thoracic, abdominal and gynecological operations;
- hemorrhoidectomy.
The risk of pulmonary infarction is high in people over 60 years of age, as well as in:
- recurrent venous thrombosis;
- hereditary burden of pulmonary embolism;
- taking hormonal contraceptives;
- the presence of a pancreatic tumor;
- obesity;
- pulmonary hypertension.
Dangerous background pathologies are considered:
- DIC syndrome;
- sickle cell anemia;
- polycythemia;
- heparin-induced thrombocytopenia.
Complications of pulmonary embolism
Most people with PE are treated successfully and have no serious complications. However, serious complications are possible, including:
- Collapse - due to the effect of a blood clot on the heart and circulation. This can cause cardiac arrest and can be fatal. PE can cause heart strain. This can lead to a condition called heart failure, where the heart pumps less than normal.
- Recurrence of pulmonary embolism. Blood clots may occur again later (called recurrent PE). Treatment with anticoagulants helps prevent this.
- Bleeding. Complications due to treatment. Treatment with anticoagulants may have side effects. The main one is bleeding in various locations, for example, from a stomach ulcer. Approximately 3 in 100 patients will have significant bleeding due to treatment of PE with anticoagulants. This type of bleeding can usually be treated successfully. However, it is almost always safer to take anticoagulants to prevent recurrent PE, which can be even more severe.
- Chronic pulmonary hypertension. If small PEs recur, they may contribute to the development of a condition in which there is increased pressure in the blood vessels of the lungs (pulmonary hypertension).
Signs of pulmonary infarction
The first symptoms of a pulmonary infarction appear two to three days after a branch of the pulmonary artery is blocked by a thrombus. The patient feels sudden pain in the chest, which intensifies when coughing, deep breathing, or bending over. Discomfort in the chest area is explained by reactive pleurisy in a necrotic area of the lung.
With a reaction of the diaphragmatic pleura, an “acute abdomen” is possible. In 30% of patients, hemoptysis is observed or “rusty” streaks appear in the sputum. Pulmonary hemorrhage occurs in 2-5%.
Also, pulmonary infarction can manifest itself:
- increase in body temperature to 38-39°C;
- severe shortness of breath;
- arrhythmia;
- cyanosis and pallor of the skin;
- arterial hypotension;
- hiccups;
- vomiting, nausea.
Half of the patients develop hemorrhagic or serous pleurisy. Occasionally, cerebral disorders occur. Their symptoms:
- jaundice;
- fainting;
- coma.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Diagnosis of pulmonary infarction
Pulmonologists and cardiologists diagnose pulmonary embolism. During a physical examination, the following is revealed:
- small wheezing;
- decreased breathing;
- pleural friction noise;
- systolic murmur;
- shortening of percussion sound;
- gallop rhythm;
- splitting and emphasis of the second tone on the aorta.
While palpating the abdomen, the doctor notes an enlarged and painful liver.
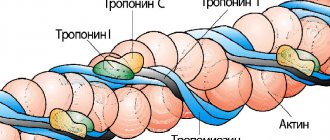
Blood biochemistry, general blood test and blood gas analysis during pulmonary infarction show:
- moderate leukocytosis;
- arterial hypoxemia;
- total bilirubin with normal transaminase values;
- increased activity of lactate dehydrogenase.
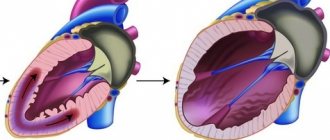
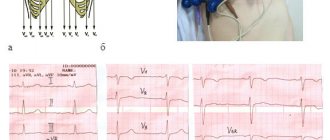
Pulmonary infarction on the ECG is manifested by signs of overload of the right heart parts, incomplete blockade of the right bundle branch. EchoCG markers of pulmonary embolism may include:
- hypokinesia and dilatation of the right ventricle;
- increased pressure in the artery of the lung;
- detection of a blood clot in the right side of the heart.
Ultrasound scanning of the veins of the lower extremities during pulmonary infarction diagnoses deep vein thrombosis. An x-ray of the lungs in lateral and frontal projections shows:
- deformation and expansion of the lung root;
- a wedge-shaped area of decreased transparency;
- effusion in the pleural cavity.
Pulmonary angiography for pulmonary embolism reveals narrowing of the lumen of the pulmonary artery due to intra-arterial filling defects. Scintigraphy is used to confirm the presence of areas of decreased pulmonary perfusion.
Pulmonary infarction must be differentiated from:
- atelectasis;
- lobar pneumonia;
- spontaneous pneumothorax;
- pericarditis;
- myocardial infarction;
- rib fracture;
- myocarditis.
4.Treatment
First aid for suspected pulmonary infarction consists of relieving intense pain and immediate hospitalization of the patient. Further, according to indications (and in the absence of contraindications), anticoagulants, antiplatelet agents, thrombolytics, hormonal vasopressors, and supportive oxygen therapy are used; if there is a reasonable or confirmed suspicion of post-infarction infection, broad-spectrum antibiotics are used in effective doses. In some severe cases, the method of choice, which does not have a reasonable life-saving alternative, becomes thoracic surgical intervention.
It should be emphasized that in case of pulmonary infarction, the time factor is critical. The prognosis is favorable if you seek help in a timely manner and apply an adequate protocol for its provision, when it is possible to quickly and accurately diagnose the cause and prevent possible complications.
How to treat pulmonary infarction
Treatment of pulmonary infarction in children and adults involves the use of:
- non-narcotic or narcotic analgesics for pain relief;
- direct (Frakiparin, Heparin) and indirect coagulants to prevent further thrombus formation (coagulants are contraindicated in cases of bleeding, duodenal/gastric ulcers, hemorrhagic diathesis, malignant tumors);
- fibrinolytic therapy with Urokinase, Streptokinase or tissue plasminogen activator to dissolve existing blood clots.
If a pulmonary infarction is complicated by arterial hypertension, vasopressors (Dopamine, Norepinephrine), Reopoliglucin are administered intravenously. At the first symptoms of heart attack-pneumonia, antibiotics are prescribed. Also, patients with pulmonary embolism require oxygen inhalation through a special nasal catheter.
If conservative treatment does not provide improvement in well-being, thromboembolectomy is performed from the pulmonary artery - a vena cava filter is installed in the inferior vena cava system.
Prevention of pulmonary infarction
Prevention of pulmonary infarction is carried out taking into account the reasons that provoked the development of the disease. To avoid pulmonary embolism, cardiologists and pulmonologists recommend:
- promptly treat thrombophlebitis;
- wear compression stockings for pathologies of the veins of the lower extremities;
- do therapeutic exercises daily;
- observe the timing of the use of intravenous catheters during infusion therapy;
- follow the doctor’s recommendations after undergoing surgical treatment.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
What are the prospects for pulmonary embolism?
This depends on the type of pulmonary embolism and the presence of concomitant diseases.
If PE is treated correctly and promptly, the prognosis is good and most patients can make a full recovery.
The prognosis is worse if there is a serious disease that contributed to the embolism, such as advanced cancer. Massive PE is more difficult to treat and is life-threatening. PE is a serious condition and can have a high risk of death, but this is greatly reduced with early treatment.
The most dangerous time for complications or death is the first few hours after an embolism. In addition, there is a high risk of developing a new pulmonary embolism within six weeks of the first one. Therefore, treatment must be started immediately and continued for at least six months.