Characteristics of the drug
Heparin is a drug that interferes with the formation of the high molecular weight protein fibrin in order to prevent the formation of blood clots in the coronary arteries. In addition, the action of the medication is aimed at stopping the growth of already formed fibrin clots and reducing the activity of blood clotting factors.
The drug for injection is available in bottles with a dosage of 5 ml
The administration of the drug in small quantities can slightly increase the properties of blood aimed at dissolving formed blood clots, and in large doses heparin causes a slowdown in the process of dissolving blood clots.
To reduce the risk of coronary heart disease and restore the normal balance of the liquid part and formed elements of the blood, doctors prescribe Heparin injections. The treatment regimen and dose of the administered drug are selected individually, since the drug can accumulate on the inner surface of blood vessels, which leads to an increase in the negative charge of blood cells. Due to this, surface adhesion decreases and platelet gluing process is inhibited.
Analogs
Level 4 ATC code matches:
Girudoproct
Heparoid Zentiva
Heparin ointment
Gepatrombin G
Lyoton
Trombless
Venolife
Hepatrombin
Gel analogues: Heparin-Acrigel 1000 , Lyoton 1000 , Lavenum , Trombless .
Generic injection forms: Heparin J , Heparin-Ferein , Heparin-Sandoz .
Drugs with a similar mechanism of action: tablets - Piyavit , Angioflux , Wessel Due F ; solution - Angioflux , Hemapaxan , Antithrombin III human , Wessel Due F , Fluxum , Anfibra , Fraxiparine , Enixum .
Pharmacological properties
Most patients have a question: why is it necessary to prescribe Heparin injections? The drug is used in the form of a solution for injection, as this promotes rapid penetration of the active substance into the bloodstream and instantly slows down the process of coagulation of biological fluid.
The drug causes a moderate vasodilator effect
The drug exhibits the following effects in the body:
- increases renal blood supply;
- increases the tone of cerebral vessels;
- slows down enzymatic activity of the brain;
- reduces the rate of excess aldosterone synthesis in the adrenal glands;
- promotes the activation of parathyroid hormone;
- controls the level of adrenaline in the blood.
In complex therapy for patients diagnosed with coronary insufficiency, administration of the solution helps prevent the development of the following pathologies:
- acute thrombosis of coronary vessels;
- reducing the number of relapses of myocardial infarction;
- reduction in the number of deaths after coronary heart disease.
A low dosage of the drug is used to prevent the formation of blood clots inside blood vessels and in patients after surgery. Large doses of the drug are intended for the treatment of pulmonary arterial thromboembolism or venous blockage.
Contraindications
Heparin containing ointments (Heparin, Heparin-Acrigel 1000, etc.) are contraindicated in cases of hypersensitivity to the components they contain, as well as in diseases accompanied by ulcerative-necrotic processes, and injuries that are accompanied by violations of the integrity of the skin.
Heparin gel (ointment) should be used with caution in case of thrombocytopenia and increased tendency to bleeding.
Contraindications to the use of the injection form of the drug:
- hypersensitivity;
- diseases accompanied by increased bleeding ( vasculitis, hemophilia , etc.);
- bleeding;
- aortic dissection , intracranial aneurysm;
- antiphospholipid syndrome;
- traumatic brain injury;
- hemorrhagic stroke;
- uncontrolled hypertension;
- liver cirrhosis , accompanied by pathological changes in the veins of the esophagus;
- threatened miscarriage;
- menstrual period;
- pregnancy;
- childbirth (including recent);
- lactation period;
- erosive and ulcerative lesions of the stomach and intestinal tract;
- recent surgical interventions on the prostate gland, brain, eyes, bile ducts and liver, as well as the condition after lumbar puncture .
Heparin injections should be prescribed with caution to patients with polyvalent allergies (including bronchial asthma ), diabetes mellitus , arterial hypertension , active tuberculosis , endo- and pericarditis , chronic renal failure, liver failure ; patients undergoing dental procedures or radiation therapy; persons over 60 years of age (especially women); women using an IUD.
Indications for use
Patients with impaired blood clotting function are recommended to undergo a course of Heparin injections. The drug has a broad pharmacological effect, so in medicine it is used not only as an anticoagulant.
To prevent blood clotting, the drug is used during the hemodialysis procedure.
Administration of the solution is indicated in the presence of the following conditions:
- progressive form of angina;
- IHD in the acute phase;
- prevention and treatment of thrombosis of various origins;
- after operations related to pathology of the heart and blood vessels;
- pathology of the valve apparatus;
- inflammation of the heart valves;
- blockage of the renal vein by a thrombus;
- inflammatory kidney diseases;
- bronchial asthma;
- systemic inflammatory conditions;
- cleaning of venous catheters.
Good results are obtained by using the solution for prophylactic purposes, in case of clot formation in the lumen of peripheral arteries and after surgery in the heart area.
Use in pediatrics
Heparin for children in various release forms is prescribed by the attending physician if there are indications for use. Injections are often used to prevent blood clots after surgery. There are no age restrictions, but before reaching 3 years of age, injections are prescribed only if necessary.
The drug in the form of an ointment is prescribed to children from one year of age, despite the fact that the instructions prohibit the use of the drug under 3 years of age. If you are prone to bleeding or are at risk of developing it, Heparin is contraindicated in children.
Duration of pharmacological effect
If the solution is administered by intradermal injection into the abdominal area, the patient should know that they must be done frequently, since the pharmacological effect occurs quickly and its duration is short-lived. When the drug is administered intravenously, an almost instantaneous inhibition of blood clotting is observed, while its effect lasts up to 5 hours.
To prevent the formation of fibrin clots, the duration of action of the drug increases slightly
After an injection into the muscle, the therapeutic effect occurs after 30 minutes and lasts for 6 hours. The effect of intradermal administration occurs within 40 minutes and lasts up to 8 hours.
special instructions
Due to the risk of hematoma formation at the injection site, the solution should not be injected into the muscle.
The solution may acquire a yellowish tint, which does not affect its activity or tolerability.
When prescribing the drug for therapeutic purposes, the dosage should be selected taking into account the aPTT value.
During treatment with the drug, organ biopsies and other medications should not be administered intramuscularly.
To dilute the solution, only 0.9% NaCl solution can be used.
The gel should not be applied to mucous membranes or open wounds. In addition, it is not used in the presence of purulent processes. The use of ointment is not recommended for DVT.
Unfractionated Heparin
Heparin with an average molecular weight of 12-16 thousand daltons, which is isolated from bovine lung or the mucous membrane of the intestinal tract of pigs, is called unfractionated. It is used in the production of drugs that have local and systemic effects (heparin containing ointments and solutions for parenteral administration).
The drug, through interaction with AT III (indirectly), inhibits the main enzyme of the blood coagulation system, as well as other coagulation factors, and this in turn leads to antithrombotic and anticoagulation effects.
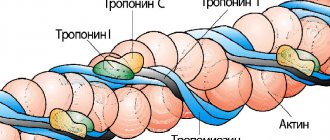
Endogenous heparin in the human body can be found in muscles, intestinal mucosa, and lungs. In structure, it is a mixture of glycosaminoglycan fractions, which consist of sulfatide residues of D-glucosamine and D-glucuronic acid with a molecular weight of 2 to 50 thousand daltons.
Fractionated Heparin
Fractionated (low molecular weight) heparins are obtained by enzymatic or chemical depolymerization of unfractionated heparins. This Heparin consists of polysaccharides with an average molecular weight of 4-7 thousand daltons.
LMWHs are characterized as weak anticoagulants and highly effective direct-acting antithrombotics. The action of such drugs is aimed at compensating hypercoagulation processes.
LMWH begins to act immediately after administration, while its antithrombotic effect is pronounced and prolonged (the drug is administered only 1 time per day).
Classification of low molecular weight Heparins:
- drugs used to prevent thrombosis/thromboembolism ( Klivarin , Troparin , etc.);
- drugs used to treat unstable angina and MI without a pathological Q wave, thrombosis and thromboembolism , acute DVT, PE ( Fragmin , Clexane , Fraxiparine );
- drugs used to treat severe vein thrombosis ( Fraxiparine Forte );
- drugs used to prevent thrombus formation and coagulation during hemofiltration and hemodialysis ( Fraxiparine , Fragmin , Clexane ).
Methods of administration
Complex therapy of acute venous and arterial thrombosis involves continuous intravenous drip administration of Heparin solution for several days. If there are possible contraindications to intravenous infusion, the drug must be administered subcutaneously or intramuscularly.
The optimal route for administering Heparin is considered to be the abdominal wall.
After surgery or directly during the operation, the solution is injected into the artery or intravenously. Then, during the first days after surgery, the administration of Heparin is continued intravenously.
In ophthalmology, in case of acute blockage of the vessels of the retina or dystrophic changes inside its membrane, the drug is administered intravenously, and then intramuscular injections are used.
Features of dosage selection
The dose of the administered solution depends on the degree of thrombosis, the severity of symptoms and the individual sensitivity of the patient to the drug. In patients, it is necessary to constantly monitor coagulogram parameters, since if the dose is incorrectly selected, the blood clotting period can significantly exceed the norm, which can lead to bleeding.
Before discontinuing the drug, the daily dosage must be reduced so that there is no increase in the intervals between injections
According to the instructions for use, the dosage of the drug is prescribed depending on the route of administration:
- Intravenous drip infusions. The daily dosage is selected at the rate of 400 U/kg.
- Intramuscular and subcutaneous injections. The dose of the solution should not exceed 600 units/kg per day.
- Intravenous administration. Single dose – 100 units/kg.
After completing the course of Heparin therapy, anticoagulant treatment with indirect-acting drugs is prescribed, the administration of which begins one day before the first reduction in the dose of the active substance.
Overdose
Symptoms of overdose with parenteral use are bleeding of varying severity.
Treatment: for minor bleeding caused by an overdose of the drug, it is enough to stop using it. If bleeding is extensive, protamine sulfate (1 mg per 100 IU of heparin) is used to neutralize excess heparin.
Please note that heparin is eliminated quickly. Thus, if protamine sulfate is administered 30 minutes after the previous dose of heparin, it should be administered at half the dose; The highest dose of protamine sulfate is 50 mg.
It is not excreted by hemodialysis.
Cases of overdose with external use of the drug have not been described. Due to the low systemic absorption of the drug, an overdose is considered unlikely. With prolonged use on large surfaces, hemorrhagic complications .
Treatment: discontinuation of the drug, if necessary, use of a one percent solution of protamine sulfate (heparin antagonist).
Use of the product during pregnancy
During pregnancy, women's blood viscosity may change. An increase in the number of platelets leads to increased coagulability of biological fluid. According to statistics, 10% of pregnant women are susceptible to homeostatic disorders. Therefore, some doctors prescribe Heparin during pregnancy, when the therapeutic effect of the drug is higher than the possible side effects.
Long-term use of heparin may increase a pregnant mother's risk of bleeding
According to clinical studies, the drug does not penetrate the transplacental barrier, which means it does not pose a threat to the fetus. The treatment regimen for a pregnant woman is somewhat different, for example, the calculation of the dose of the injected solution depends on the woman’s weight category, and the frequency of injections is limited to two.
The use of Heparin should be carried out under the strict supervision of specialists, since spontaneous labor may develop. In case of long-term treatment, it is recommended to take a blood test for coagulation once every two days, and with heparin therapy for more than 7 days, the test is taken once every 3 days.
The use of the medication may interfere with the distribution of calcium in the body. Thus, a pregnant woman may experience acute calcium deficiency, so along with the use of Heparin, supplements containing all the necessary microelements should be taken.
USE OF HEPARINS IN CLINICAL PRACTICE
The paper deals with the prevention and treatment of thromboses and microcirculatory disorders, outlines heparins, direct-acting anticoagulants, which are widely used clinical practice all over the world.
Prof. V.A. Makarov, T.B. Kondratyev Hematology Center VGNTs, Moscow Medical Academy named after. THEM. Sechenov Prof. VA Makarov, TB Kondratyeva All-Russian Heparinology Research Center, IM Sechenov Moscow Medical Academy
P
The problems of prevention and treatment of thrombosis, as well as microcirculation disorders, are important for clinical practice.
In Russia and the CIS countries there is a steady increase in the number of patients with diseases accompanied by thrombosis and embolism. Such diseases include myocardial infarction, thrombosis of blood vessels in the limbs, brain, lungs, eyes, etc. Thrombosis often occurs after surgical interventions, especially with the use of artificial blood circulation machines. It has been shown that the cause of thrombosis can be not only damage to the vascular wall, but also pathological changes in blood clotting enzymes and natural anticoagulants. Activation of the blood coagulation system (i.e., enzymes that activate fibrin formation) is also characteristic of DIC syndrome. The latter is the most common form of hemostasis pathology. It often occurs in many diseases and pathological conditions, in particular in infectious diseases, shock, traumatic surgical interventions, terminal conditions, obstetric pathology, malignant tumors, destructive processes in organs and tissues, immune and immune complex pathologies, acute allergic reactions, after heavy bleeding , massive blood transfusions, overdose of drugs with procoagulant activity, etc. [1]. In this regard, in these clinical situations there is a need to use substances that prevent fibrin formation, i.e., anticoagulants. The most widely used in clinical practice around the world are heparins, which belong to the group of direct-acting anticoagulants (i.e., interacting directly with blood clotting factors). Heparins are glycosaminoglycans of varying molecular weight, consisting of sulfated residues of D-glucosamine and D-glucuronic acid. These polymers are formed in the body of humans and animals and are found mainly in mast cells. They were first discovered in 1916 by J. McLean. In 1918, W. Howel and E. Holt isolated this anticoagulant from dog liver (hence the name “heparin”). The clinical use of heparin became possible after 1930, when its sodium salts were obtained. The mechanism of the anticoagulant action of heparins depends on the molecular weight. In unfractionated drugs (first generation drugs) called heparin, high molecular weight fractions of glycosaminoglycan predominate. The effect of these drugs is due to the fact that they form a complex with antithrombin III, leading to an increase in the latter’s ability to inhibit thrombin, Hageman factor, factors IX, X, XI, etc. Low molecular weight fractions of heparin (less than 6 kDa), contained in drugs such as nadroparin, dalteparin, enoxyparin, reviparin, etc., have a different mechanism of anticoagulant action. The latter is mainly associated with inhibition of factor Xa activity. To a lesser extent, these drugs affect the activity of factor IIa (thrombin) and other blood clotting factors. It should be noted that for the prevention of thrombus formation, inhibition of factor Xa activity is more beneficial than influencing the underlying phases of fibrin formation (see figure), since it requires less drug. For a long time, heparins were isolated from the liver and lungs of cattle, then from the intestines of pigs, which turned out to be more profitable. Low molecular weight heparins are produced by depolymerization of high and medium molecular weight polymers. Currently, the main indications for heparin therapy are venous thrombosis, pulmonary embolism, disseminated intravascular coagulation, unstable angina, acute infarction, and ischemic stroke.
For prophylactic purposes, heparin preparations are used during surgical interventions, in case of circulatory failure, and to prevent blood clotting when using extracorporeal circulation. Thus, heparin preparations are used in a significant proportion of patients. Despite the fact that heparin therapy has been carried out for 6 decades and heparin preparations still dominate today over other direct-acting anticoagulants, treatment with heparins is associated with the risk of a number of complications. First of all, this is the occurrence of bleeding. Bleeding during heparin therapy is associated not only with excessive inhibition of fibrin formation, but also with the fact that thrombocytopenia develops during this therapy. In this case, two variants of thrombocytopenia are possible. In the first option, short-term thrombocytopenia that quickly resolves after discontinuation of heparin is associated with its ability to activate the aggregation function of platelets, potentiate the effect of other aggregation stimulators and weaken the antiaggregation effect of prostacyclin. In the second immune variant, along with increased intravascular aggregation and consumption of platelets into microthrombi, specific autoantibodies to certain platelet receptors are detected. Other complications of heparin therapy include allergic reactions, osteoporosis, priapism, and decreased antithrombin III levels. In recent years, a large number of comparative studies have been conducted to evaluate the effectiveness, safety and ease of clinical use of unfractionated and low-molecular-weight heparin preparations. It has been established that low molecular weight heparins have greater bioavailability (more than 3 times) when administered subcutaneously than unfractionated drugs. The half-life of low-molecular-weight heparins is 2–4 times longer, which helps to extend the duration of the drug. In this regard, low molecular weight heparin preparations can be administered 1–2 times a day. The differences in pharmacokinetics are explained by the lower tendency of low molecular weight heparins to bind to plasma proteins, such as histidine-rich glycoprotein, platelet factor 4, vitronectin, fibronectin, von Willebrand factor, etc. Thus, unfractionated heparin preparations are eliminated in two phases: the rapid saturation phase, i.e. protein binding, and the phase of renal clearance. Low molecular weight heparins are almost completely eliminated by the kidneys. Unfractionated heparin preparations are administered intravenously, in the form of drip infusions, subcutaneously, intramuscularly. Low molecular weight heparins are administered subcutaneously, intramuscularly, and some drugs are administered orally. The advantages of low molecular weight heparins include a lower likelihood of developing thrombocytopenia. This may be largely due to the fact that when using these drugs, a lower percentage of hemorrhagic complications is observed. Based on these patterns, treatment with low molecular weight heparins does not require such careful laboratory monitoring as treatment with unfractionated drugs.
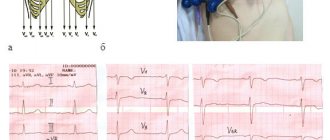
Often, as a laboratory control of the effectiveness of the drug, the coagulation and recalcification time of whole blood, partial thromboplastin time in various modifications, and activated coagulation time are determined. However, these techniques are not highly sensitive. They are little sensitive to low concentrations of heparin in the blood. The activated partial thromboplastin time (aPTT) test, as well as thrombin (and preferably thrombin-calcium) time, are somewhat more sensitive. When using the APTT test, it is shown that with heparin therapy (non-fractionated heparin), to achieve a therapeutic effect, it is necessary to lengthen the time by 1.5 - 2.5 times. More specific are methods based on measuring the activity of thrombin when it is inhibited by the plasma of a patient treated with heparin (i.e., the anti-IIa-antithrombin activity of heparin is determined). The sensitivity of the method increases with this formulation, when thrombin of increased activity is introduced into the plasma and the activity is recorded using a chromogenic substrate (for example, S-2288). When monitoring treatment with low molecular weight heparins, the determination of plasma anti-Xa activity is of particular importance. It is advisable to use chromogenic substrates as reaction indicators. In this regard, it is interesting to compare the ratio of antithrombin and anti-Xa activities in different heparin preparations. For unfractionated heparin, it is approximately equal to 1. For unfractionated heparins, this ratio is: for dalteparin – 2.2, logiparin – 1.5, nadroparin – 3.5, enoxoparin – 3.9 [2]. Issues of dosing heparin drugs and monitoring treatment for various diseases are presented in many publications, reference books and guidelines [3 – 6]. In recent years, a number of studies have been carried out with the analysis of large groups of patients to comparatively evaluate the clinical effectiveness of unfractionated and low molecular weight heparin preparations. According to J. Hirst [7], when treating venous thrombosis with unfractionated heparins and oral anticoagulants, repeated venous thromboembolism was noted in 0.8% of cases, when treating with an unfractionated drug and oral anticoagulants - in 3.2%. The mortality rate in the first case was 3.2%, including due to pulmonary embolism - 0.1%, and in the second case - 5.9%, including due to pulmonary embolism - 0.2%. Severe bleeding during treatment with low molecular weight heparins was 3%, and with unfractionated heparins - 6.7%, minor bleeding in the first case was 11%, in the second - 9.9%. The improvement in venogram indicators in the first case was 65.3%, in the second – 52%. According to FJJ Turpie [8], mortality in the treatment of venous thrombosis with unfractionated heparin was 7.1%, and in treatment with low molecular weight heparin – 3.9%. In unstable angina, unfractionated heparin and low molecular weight heparin have similar effects in terms of preventing death, myocardial infarction, revascularization, etc. [9]. There is evidence in the literature that low molecular weight heparins are safer in terms of hemorrhagic complications than unfractionated heparins in cerebrovascular accidents [10]. Summarizing the above, we can conclude that at present, most researchers consider low molecular weight heparins to be not inferior in potency to unfractionated heparin. However, as stated earlier, they have a number of advantages. This explains the fact that after 13 years of clinical use, small molecule drugs are gradually replacing unfractionated heparin in many areas of medicine.
The appearance of low molecular weight heparins in the clinic coincided with the introduction of other new direct-acting anticoagulants. We are talking primarily about hirudin, its derivatives, as well as synthetic and peptide thrombin inhibitors. These drugs do not require endogenous cofactors, in particular antithrombin III. However, it should be taken into account that if there is a danger of hemorrhage, poisoning with these drugs is more difficult to stop, since they do not yet have specific antagonists. Meanwhile, the effect of heparins is removed by specific antagonists - protamine sulfate, polybrene, etc. Based on the advantages that heparins have, the search for new direct-acting anticoagulants is actively being carried out among sulfated polymers. In particular, polysulfates of pentosan, dermatan, etc. are also used abroad in clinical practice. However, they are inferior to heparins in specific activity and safety of use. In the laboratory of pathology and pharmacology of hemostasis of the Hematology Research Center of the Russian Academy of Medical Sciences [11], a new anticoagulant chitorin is being developed, which is a mixture of heparin and chitosan polysulfate of a certain molecular weight and degree of sulfation. This composition is due to the fact that the authors were the first to demonstrate the ability of chitosan polysulfate to potentiate the anticoagulant effect of heparin. Chitorin, having a specific activity close to heparin, has less effect on the concentration of platelets in the blood and has less hemorrhagic activity. Completing preclinical trials indicate the low toxicity of chitorin. Thus, over 60 years of clinical use, heparin preparations have shown high effectiveness in the prevention and treatment of thrombosis and disseminated intravascular coagulation syndrome. Over the past 13 years, it has been possible to identify the advantages of low-molecular-weight heparin preparations over unfractionated drugs. Heparins serve as the basis for the development of new direct-acting anticoagulants.
Literature:
1. Barkagan Z.S. Hemorrhagic diseases and syndromes. M., Med., 1988. 2. Annotation: low molecular weight heparin (S). Brit J Haematol 1995;90:1. 3. Barkagan Z.S. In the book: Guide to Hematology, ed. A.I. Vorobyova, M., Med., vol. 2, 1985, p. 160. 4. Bokarev I.N., Shchepotin B.M., Ena Ya.N. Intravascular blood coagulation. Kyiv, Health, 1989. 5. Study of the blood system in clinical practice. Ed. G.I. Kozinets and V.A. Makarova, M. Triada-X, 1997. 6. Mashkovsky M.D. Medicines. v.1, Kharkov, Torsing, 1997, p.462. 7. Hirsh J, et al. Low molecular weight heparin in the treatment of patients with acute venous thromboembolism. Thrombos Haemostas 1995;74(1):360. 8. Turpie AJJ. New therapeutic opportunities for heparins: what does low molecular weight heparin offer? Thrombosis and Thrombolysis 1996;3:145. 9. Fragmin During Instability in Coronary Artery Disease (FRJSC) Study Group. Low molecular weight heparin during instability in coronary artery disease. The Lancet 1996;347:561. 10. Kay R, Wong KS, Yu YL, et al. Low molecular weight heparin in ischemic stroke. Fiss study. N Engl Med 1995;333(4):1588. 11. Drozd N.N., Makarov V.A., Bashkov G.V. and others. The effect of joint administration of heparin and chitosan sulfate on the function of hemostasis. Exp. and wedge. Pharmakol, 1996, 59, 1, 30.
Special Recommendations
Heparin therapy is carried out under strict control of hemocoagulation parameters. A coagulogram is carried out in the first week of treatment with the drug and immediately after surgery, the optimal number of studies is 1 time every 2-3 days. With fractional administration of the solution, a blood test is done immediately before the injection.
It is not recommended to abruptly interrupt the course of treatment with Heparin, as this may lead to the initiation of thrombus formation. Therefore, it is necessary to gradually reduce the dosage of the drug with the parallel use of indirect anticoagulants. The only exceptions are cases of individual intolerance to some components of the solution.
Despite the possibility of intramuscular injection of the solution, experts do not recommend it due to the fact that bruises form at the injection site.
Compound
The injection solution contains sodium heparin at a concentration of 5 thousand units/ml.
The auxiliary components of the drug include sodium chloride, benzyl alcohol, and water. 1 gram of gel contains 1 thousand units of sodium heparin , as well as auxiliary components: 96% ethanol, carbomer , dimethyl sulfoxide, propylene glycol, dietanolamine, methyl and propylparaben (additives E 218, E 216), lavender oil and purified water.
Algorithm for the correct administration of Heparin
Injections of the drug are carried out strictly as prescribed by a specialist. Injections of the drug are made at a strictly defined time of day, so patients often practice self-injections of the solution into the abdominal area. This route of administration is considered the most convenient at home.
Insulin syringes are used for injections, since a thin needle causes minimal pain.
Algorithm for how to give injections in the abdominal area:
- Perform hand hygiene using soap and antiseptic.
- Before manipulation, prepare a bottle of solution, a syringe, sterile cotton wool, and alcohol.
- Using a special nail file, open the bottle and collect the required amount of solution.
- Disinfect the injection site. Use your thumb and forefinger to form a fold of skin on your abdomen.
- Insert a needle into the fold formed, press the plunger and slowly inject the medicine.
- Remove the needle and apply cotton wool to the injection site.
Side effects
If you follow the Heparin treatment regimen, the symptoms of the disease gradually decrease, but situations arise when taking the medicine causes side effects:
- allergic reaction;
- migraine headaches;
- osteoporosis;
- dysfunctions of the digestive tract;
- diarrhea;
- hyperthermia;
- skin rashes;
- bleeding;
- impaired renal function.
The most common complications of taking the medication are nausea and vomiting.
As a rule, side effects occur due to uncontrolled or prolonged use of the medication. To reduce the risk of negative effects, it is necessary to observe the dosage of the solution and adhere to the treatment regimen.
What can be replaced
An analogue of Heparin is also a solution of a drug, but from a different production.
The following solution analogues exist:
- Sodium Brown.
- Richter.
- Frayn.
The use of these funds should be carried out after consultation with a specialist.
Thus, Heparin is a good drug for thinning the blood and preventing the development of blood clots inside blood vessels. However, during its use it is necessary to carefully monitor blood clotting parameters and follow the chosen therapeutic course.
Drug interactions
The therapeutic effect of the described medication is enhanced when combined with non-steroidal anti-inflammatory drugs and antiplatelet agents. When used simultaneously with Tetracycline, antiallergic drugs, nicotine, the effect of Heparin is reduced.
When using the drug, its drug interactions must be taken into account.
Reviews
Ivan, 50 years old I had a myocardial infarction several years ago. This was followed by a long recovery period, during which I was prescribed daily Heparin injections. After the course of treatment, hemostasis indicators were restored, however, to prevent further thrombus formation, I periodically take injections of the drug.
Svetlana, 42 years old I have problems with blood clotting, it has become too thick. Against this background, I developed a thrombosis in my leg, which is why I have a severe limp when walking. The doctor ordered me to take Heparin injections in the stomach for 1 month. Thanks to this medication, everything went away, although bruises formed on my stomach during the course, but this is not so important.
Igor, 28 years old My mother was diagnosed with varicose veins in her lower extremities; a vessel was blocked in one of her legs, so she was prescribed surgical treatment. In the postoperative period, she was prescribed to undergo heparin treatment. The result is obvious, the condition of the veins has improved significantly. At the moment, the disease is not progressing; my mother periodically undergoes medication treatment, as this also serves as a good prevention of myocardial infarction.
Pharmacodynamics and pharmacokinetics
What is Heparin?
Heparin (INN: Heparin) is an acidic mucopolysaccharide with Mr about 16 kDa. A direct anticoagulant that helps slow down the formation of fibrin .
The gross formula of heparin is C12H19NO20S3.
Pharmacodynamics
The mechanism of action of heparin is based primarily on its binding to AT III (its plasma cofactor). Being a physiological anticoagulant , it potentiates the ability of AT III to suppress activated coagulation factors (in particular, IXa, Xa, XIa, XIIa).
When used in high concentrations, heparin also inhibits thrombin activity .
Suppresses activated factor X, which is involved in the internal and external blood coagulation system.
The effect occurs when significantly lower doses of heparin are used than are required to inhibit the activity of coagulation factor II ( thrombin ), which promotes the formation of fibrin from the plasma protein fibrinogen .
This justifies the possibility of using small doses of heparin (subcutaneously) for prophylactic purposes, and large doses for treatment.
Heparin is not a fibrinolytic (i.e., it is capable of dissolving blood clots), but it can reduce the size of the blood clot and stop its expansion. Thus, the blood clot is partially dissolved under the action of fibrinolytic enzymes of natural origin.
Suppresses the activity of the enzyme hyaluronidase, helps reduce the activity of surfactant in the lungs.
Reduces the risk of developing MI, acute thrombosis of myocardial arteries and sudden death. In small doses it is effective for the prevention of VTE, in high doses it is effective against venous thrombosis and pulmonary embolism .
Deficiency of AT III at the site of thrombosis or plasma may reduce the antithrombotic effect of the drug
When applied externally, the product has a local antiexudative , antithrombotic and moderate anti-inflammatory effect .
Promotes the activation of fibrinolytic properties of blood, inhibits the activity of hyaluronidase, and blocks the formation of thrombin. Gradually released from the gel and passing through the skin, heparin helps reduce inflammation and has an antithrombotic effect .
At the same time, the patient’s microcirculation improves and tissue metabolism is activated and, as a result, the processes of resorption of blood clots and hematomas are accelerated, and tissue swelling is reduced.
Pharmacokinetics
When used externally, absorption is negligible.
After injection under the skin, TCmax is 4-5 hours. Up to 95% of the substance is in a state bound to plasma proteins, Vp - 0.06 l/kg (the substance does not leave the vascular bed due to strong binding to plasma proteins).
It does not penetrate the placental barrier or into breast milk.
Metabolized in the liver. The substance is characterized by rapid biological inactivation and short duration of action, which is explained by the participation of the antiheparin factor in its biotransformation and the binding of heparin to the macrophage system.
T1/2 - 30-60 minutes. Excreted by the kidneys. Up to 50% of the substance can be excreted unchanged only if high doses are used. It is not excreted by hemodialysis.