Myocardial infarction
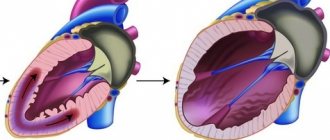
is an acute form of coronary heart disease. The essence of the pathology is a sharp disruption of the blood supply to the tissues of the heart and the appearance of an area of necrosis. Modern techniques make it possible to respond to the disease in a timely manner; there are endovascular and medicinal methods of restoring blood flow. The question of timely diagnosis remains open - after all, the initiation of effective therapeutic measures depends on this. In order to determine the presence of a heart attack, a number of techniques are used, including assessment of the clinical picture, instrumental and laboratory methods.
Clinical picture of the pathology
Symptoms of a heart attack can vary. The first and main symptom is pressing pain behind the sternum, which has a compressive nature; patients often note that it is burning and very intense. Pain occurs at the height of emotional stress or physical activity. Its sudden occurrence leads to general weakness and interruptions in breathing.
In addition to pain, the following symptoms may be observed:
- nausea;
- loss of consciousness;
- weakness;
- increased sweating;
- pallor.
The pain is usually localized behind the sternum, but can radiate to the left arm, shoulder, interscapular area, jaw, and upper abdomen. This depends on the location of necrosis.
There are clinical forms of heart attack:
- asthmatic
The patient has a dry cough, shortness of breath, and chest pain.
- abdominal
The pain is located in the upper abdomen, and severe nausea is observed.
- arrhythmic
There is an abnormal heart rhythm, weakness, and short-term loss of consciousness.
cerebral
The patient complains of severe headache.
There are asymptomatic forms of heart attack; they are observed in diabetes mellitus, as well as in patients who abuse alcohol. In this case, general weakness and disturbances of consciousness may be observed, but there is no typical pain that is characteristic of a heart attack.
Soluble tumorigenicity inhibitor 2
The source of sST2 is the interleukin-1 family receptor, which is expressed in cardiomyocytes and fibroblasts under mechanical stress and is thus considered as a biomarker of myocardial fibrosis, cardiac distension and cardiovascular remodeling [19–21]. sST2 has been found to have diagnostic and prognostic value in patients with destabilized HF, acute coronary syndrome [21], and severe chronic HF, and was included in the 2013 American Heart Association guidelines for additional risk stratification in patients with acute and chronic HF [ 23]. However, the diagnostic utility of sST2 in patients with HFpEF has not been well studied. K. B. Shah et al. [19] provided the first evidence that sST2 levels may be important in patients with HFpEF. YC Wang et al. [24] examined 107 patients with hypertension and HFpEF. Among them, 68 had symptoms of HFpEF. Interestingly, sST2 concentration was significantly lower in patients with E/E′ <8 compared to patients who had E/E′ 8–15 or >15. Multivariate analysis showed that sST2 >13.5 ng/ml is associated with the presence of HFpEF. PS Jhund et al. [25] studied 296 patients treated for HFpEF with the angiotensin receptor inhibitor neprilysin and an angiotensin II receptor blocker with sST2 measurements (PARAMOUNT). Higher levels of this biomarker were associated with older age, high HF class, high NT-proBNP, male gender, atrial fibrillation, and lower glomerular filtration rate. Increased sST2 levels were associated with higher E/E′ and larger LA size. PS Jhund et al. [25] also found an association between higher sST2 levels and male gender, increased HF class, and LA volume.
To summarize the studies on the role of sST2 concentration in HFpEF, measurement of its levels is useful for mortality risk stratification and prognosis of patients with HF, in addition to other cardiovascular risk factors [26]. sST2 concentration showed a weak correlation with the functional class of HF, LV ejection fraction, other cardiac parameters and renal function [27, 28]. Thus, soluble tumorigenicity inhibitor can be used as a biomarker to predict HFpEF, but more studies are needed to identify additional correlations between blood sST2 concentrations and other markers of HFpEF.
Modern diagnostic methods
If there is a suspicion of a heart attack, there is anamnestic data about coronary heart disease and characteristic clinical signs, the doctor prescribes a diagnostic program. It consists of the following methods:
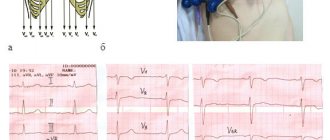
- electrocardiogram;
- laboratory diagnostics.
Let's take a closer look at these research methods.
An electrocardiogram is a graphic representation of the conduction of an impulse along the myocardial fibers. If conductivity is impaired due to necrosis, this will be reflected in the recording. Based on changes in the ECG, the localization of the necrosis zone can be distinguished. Also, on the graph you can see the phase of the infarction - acute or subacute.
General blood analysis
There are no specific changes observed in a general blood test and therefore a diagnosis cannot be made on its basis. During a heart attack, leukocytosis develops, which occurs several hours after the start of the process and reaches a maximum by the end of the day. The elevated level lasts for several days and gradually returns to normal. Leukocytes do not increase significantly, as, for example, with infectious pathology, which allows for differential diagnosis. This is important in case of an atypical clinical picture of myocardial infarction, when the doctor may suspect several pathologies. In a general blood test, you can also see an increased ESR, which remains this way for several weeks. Eosinophils also increase and remain elevated for about a week.
Blood chemistry
Alanine aminotransferase (ALT)
Indicator of destruction of hepatocytes and cardiomyocytes. It increases with hepatitis of various etiologies, heart attack, toxic damage to internal organs. ALT is an active component of liver metabolism, an enzyme that accelerates the metabolism of amino acids. The highest concentration of the substance is found in the cells of the liver, kidneys, heart, as well as in skeletal muscle tissue. Since its localization is the cytoplasm, it is released into the blood when the cell membrane is destroyed. The more massive the area of destruction, the higher the concentration of the enzyme in the blood. The peak activity of the enzyme during a heart attack is 12 hours.
An increase or normalization of ALT levels is a marker of the condition of patients of various profiles with diseases of internal organs and soft tissues. Depending on the disease, ALT can increase moderately or acutely, for example, the highest degree of concentration is observed in hepatitis.
In case of a heart attack, the de Ritis coefficient is used, which consists of comparing the activity of AST and ALT. If the value exceeds the norm, this indicates a heart attack, and if it is below its value, necrosis of the renal tissue or the active phase of hepatitis may have developed. Naturally, a diagnosis is not made based on the ALT indicator. For this, more specific markers are used. The level of transaminases is checked in a general biochemical analysis for differential diagnosis and monitoring of the patient’s general condition.
Aspartate aminotransferase (AST)
Marker of the condition of heart and liver tissues. Increases in viral hepatitis, toxic damage to heart tissue and hepatocytes. It is also used for preventive examination, if necessary, to confirm or exclude a heart attack. This substance is responsible for the exchange of amino acids in cells, so the largest amount is found in the cells of the liver, heart, skeletal muscles and red blood cells. If the cells of these organs are damaged, transaminase is released into the blood, where its increase can be detected. There is an acceptable level of the enzyme in the blood, because organ cells are periodically destroyed, but in pathological conditions this indicator increases several times or tens of times. The peak concentration in the blood is 12 hours after the onset of a heart attack. A comparison of ALT and AST indicators is also used. Each of these enzymes increases in certain pathologies, and during a heart attack their ratio is assessed. AST is not a specific indicator for a heart attack; it complements the overall picture of laboratory testing.
Creatine kinase MB
This substance is an isoenzyme, a marker of the condition of the heart muscle. Takes part in the metabolism of creatine and creatine phosphate. This substance is contained only in the myocardium, and therefore increases in its diseases - myocarditis, heart attack, rhabdomyolysis, pericarditis. The level of the substance is a marker during the acute and subacute phases of the process. A short-term increase in the indicator is observed during cardiac surgery, which reflects the reaction of the myocardium to treatment. The maximum concentration during a heart attack is observed 12 hours after the onset. High activity indicates a significant size of the affected area. The increase in this CPK fraction is compared with the general indicator of the substance in the body. In principle, assessment of the level of CPK MB is used for early diagnosis of myocardial damage, as well as for differentiating the condition from other diseases. An increase in the marker can indicate, in addition to a heart attack, conditions such as shock, poisoning and intoxication, infectious lesions of heart tissue.
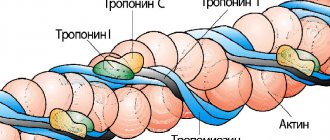
Troponin I
A protein that is found in high quantities in skeletal muscles and myocardium. There are varieties of this protein that are responsible for different phases of muscle contraction. All these proteins are cardiac-specific and indicate the state of the myocardium. Damage to cardiac myocytes leads to the release of the substance into the blood, where it can be detected using laboratory testing. The area of necrosis affects the level of increase in troponin levels in the blood. Troponin I is the most sensitive and specific for infarction. Elevated troponin persists for 5-6 days after the onset of the pathological process.
Myoglobin
This is a protein that is found in muscle cells and contains iron molecules. Similar in structure to hemoglobin, an iron-containing blood protein. The function of myoglobin is also similar - it transports oxygen to myocytes, muscle cells. With necrosis, muscle cells are destroyed, myoglobin is released and enters the bloodstream, where it can be detected. Protein is excreted from the blood along with the kidneys. It can be detected in the blood within a few hours after the onset of the pathological process; within 2-3 days it can still be detected. This marker is one of the first to react, which increases its diagnostic value. With necrotic changes, it increases 7-10 times, depending on the area of necrosis. For comparison, the period of peak increase in other markers is 12 hours, while for myoglobin it is 6 hours. Normalization of analyzes occurs just as quickly. They can remain elevated for longer than a day if complications occur, for example, expansion of the area of necrosis. Sometimes new foci occur, then myoglobin increases again, which requires dynamic monitoring of the indicator. A negative test result is also important, which, in comparison with the clinical picture, allows one to exclude pathology. In addition to a heart attack, myoglobin may indicate long-term compartment syndrome. muscle pathologies, inflammatory processes.
Diversity of biomarkers of myocardial damage and remodeling
Currently, in the diagnosis of HFpEF, much attention is paid to biochemical studies to assess the activity of myocardial damage and remodeling. It has been shown that plasma biomarkers accurately reflect changes in the hemodynamic load on the heart muscle and myocardial fibrosis, so they may be significant for the diagnosis and management of patients with HFpEF [4]. For example, matrix metalloproteinases, their tissue inhibitors and collagen processing proteins, collagen propeptides and collagen telopeptides reflect changes in collagen homeostasis and the transition from hypertension without end-organ damage to clinically symptomatic HFpEF [4, 5]. Galectin-3 and soluble suppression of tumorigenicity 2 (sST2) reflect the overall degree of fibrosis and the severity of HFpEF, which allows them to be used to determine the early stage of development of heart failure caused by fibrosis. In addition to the above-mentioned markers, growth differentiation factor 15 (GDF-15) and microRNAs are promising new biomarkers for detecting fibrosis [4–7]. Let's take a closer look at the most relevant HFpEF biomarkers.
What can influence the result?
The test results are influenced by the time of diagnosis, which has passed since the onset of the disease. Also, changes depend on the extent of the necrosis zone and the localization of the process. Many laboratory indicators that are observed during a heart attack may accompany other pathological conditions. For example, transaminases increase with diseases of internal organs, liver dysfunction, hepatitis of various etiologies, and with alcohol consumption. Troponin increases during inflammatory processes in the myocardium. Creatine kinase and myoglobin can fluctuate when the structure of muscle tissue is disrupted, rhabdomyolysis, various inflammatory processes, and myositis. Many of these indicators remain elevated after surgery, which should be taken into account when collecting anamnesis from the patient.
If possible, it is advisable to take the test on an empty stomach; before donating blood from a vein, you should rest a little. It is good if you can eliminate the use of alcohol, nicotine and physical activity before the study. You need to tell your doctor what medications you took, as they may also affect your test results.
Timely diagnosis of a heart attack allows timely treatment to begin. In the case of a heart attack, this is especially important, since time is sometimes counted by the clock. Effective therapy or surgery can prolong a patient's life, improve its quality and reduce the risk of complications. It is necessary to trust your health to trusted medical institutions, where there are conditions for accurate diagnosis in a short time.
Introduction
Despite the fact that heart failure (HF) with preserved ejection fraction (HFpEF) is a very common disease throughout the world and the number of patients with this pathology is increasing every year, many questions regarding the best diagnostic approach , remain unanswered.
Diagnosis of HFpEF often becomes a clinical challenge, and this is especially true for outpatients at an early stage of the disease without obvious signs of HF [1]. According to the recommendations of the European Society of Cardiology, the necessary components for making a diagnosis of HFpEF are [2]:
increased natriuretic peptide levels (BNP ≥35 pg/ml or NT-proBNP level ≥125 pg/ml);
preserved left ventricular (LV) ejection fraction (EF) more than 50% (LVEF ≥50%);
additional disorders of the structure and/or function of the heart;
left atrial (LA) volume index >34 ml/m2;
LV mass index ≥115 g/m2 for men and ≥95 g/m2 for women;
ratio of E to E′ ≥13, where E is the early diastolic velocity of blood flow on the mitral valve, E′ is the early diastolic velocity of movement of the mitral valve annulus fibrosus according to the results of tissue Doppler sonography;
average E′ in the septum and lateral wall of the LV <9 cm/s.
In case of diagnostic doubt, the patient may undergo stress tests or invasive measurement of elevated LV filling pressure [3].
Adrenomedullin
Noteworthy is a little-studied biomarker associated with sympathetic activity, which has vasodilating, immunomodulatory, antiproliferative and antiapoptotic effects - adrenomedullin (ADM). [39] Currently, there is little data regarding the correlation of ADM and HFpEF. In a large study by F. P. Brouwers et al. [40] reported that the terminal fragment of this molecule, MR-proADM (mid-regional pro-adreomedullin), may help in the diagnosis and identification of new patients with HFpEF, but only after determining the baseline cardiovascular risk profile in the HFpEF population. CM. Yu et al. [41] showed that ADM may specifically respond to diastolic dysfunction.
Growth differentiation factor 15
Another biomarker that may be useful in diagnosing HFpEF is GDF-15, a member of the transforming growth factor superfamily of cytokines and markers of cell damage and inflammation. GDF-15 can be used as a new biomarker to assess myocardial fibrosis. In a study by YM Zhou et al. [42] after linear correlation analysis, GDF-15 expression was found to be positively associated with the degree of cardiac fibrosis in patients with atrial fibrillation. In patients with end-stage nonischemic dilated cardiomyopathy, serum GDF-15 levels correlated with the severity of myocardial fibrosis [43]. GDF-15 expression is highly induced in cardiomyocytes in response to metabolic stress such as cardiac ischemia, tissue injury, or pressure overload conditions [12, 44, 45]. Y. Izumiya et al. [8] found a positive correlation between serum GDF-15 concentrations and HF functional class, as well as plasma BNP levels and serum high-sensitivity troponin T levels in 150 patients with HFpEF.
C. Sinning et al. [9] proposed a formula for calculating an index based on the concentrations of C-reactive protein (CRP), GDF-15, sST2 and NT-proBNP, which allows distinguishing HFpEF from HFrEF:
(CRP + GDF – 15 + sST2) / NT-proBNP.
The prognostic value of GDF-15 has also been confirmed in recent studies. GDF-15 remained a significant independent predictor of HF even after adjustment for important clinical predictors, including high-sensitivity troponin T and NT-proBNP [46, 47]. Overall, GDF-15 may serve as a biomarker to help differentiate between HFpEF and HFrEF, as well as an additional indicator of the prognosis of cardiovascular events.