The myocardium is a muscle that controls the contractions of the heart and regulates blood supply to the entire body. For uninterrupted operation, it needs regular nutrition and oxygen, supplied through the coronary arteries.
If for some reason the breathing and nutrition of the myocardium are disrupted, muscle cells begin to die. Necrosis of one or another part of the heart muscle is called myocardial infarction .
Myocardial infarction often entails complete or partial disability, and this is not the worst thing. In 10-12% of cases it threatens the patient’s very life!
17.5 million - according to statistics, this is how many people die every year in the world from heart and vascular diseases. And by 2030, according to WHO experts, this figure will reach even more terrible figures - 23.6 million deaths from CVDs per year.
Causes of myocardial infarction
In most cases, necrosis of myocardial tissue occurs due to thrombosis of the coronary artery, which is provoked by atherosclerosis - atherosclerotic plaques clog the artery, disrupting the blood supply.
Other common causes of heart attack are coronary vasospasm and coronary thrombosis.
1 Ultrasound of the heart during a heart attack
2 Diagnosis of heart attack
3 Diagnosis when there is a threat of a heart attack
Who is at risk of myocardial infarction
Risk factors are:
- hypertonic disease;
- previous heart attack;
- smoking;
- sedentary lifestyle;
- hereditary predisposition;
- increased levels of “bad” cholesterol in the blood;
- obesity;
- diabetes;
- elderly age;
- postmenopausal state (in women);
- regular stress;
- excessive stress (physical and emotional);
- bleeding disorders.
HELP OF THE SAMAZDRAV RESPIRATORY SIMULATOR IN REHABILITATION
To quickly return to a normal lifestyle, you can use the Samozdrav breathing simulator. Regular exercises on this device will improve blood supply to the heart. It can be especially useful for that group of patients who undergo rehabilitation at home.
You can start training on the simulator within 3 months after a heart attack. The Samozdrav simulator is useful both for the rehabilitation of the patient and for the prevention of a recurrent heart attack. After all, with the help of a hypercapnic mixture, vascular spasm is relieved and the functioning of the entire cardiovascular system is improved.
Due to constant training, a system of collaterals is formed - small blood vessels around the heart. They provide alternative blood supply and more complete nutrition of the heart muscle.
By exercising on the Samozdrav simulator, the patient will recover faster after a heart attack, because blood flow is normalized and the load is removed from the coronary vessels. Classes on the Samozdrav simulator will give tangible results within 3-4 months, and for such a serious illness as a heart attack this period is quite short.
Disability after a heart attack
A heart attack requires a long period of treatment and rehabilitation. At the same time, a person’s full working capacity is not always restored. For these reasons, permanent or temporary disability is given to patients with a heart attack quite often.
All patients who have suffered a major heart attack have the right to four months of paid rehabilitation based on the compulsory medical insurance policy. Usually this period of rehabilitation is enough to understand whether a person needs a disability or whether he is able to fully begin his usual work. If there is reason to think about partial loss of ability to work, the patient, on the recommendation of the attending physician, can undergo an examination by a medical and social expert commission.
To assess the level of disability, the commission will assess:
- patient self-care options,
- his education,
- possibility of returning to normal work,
- general health.
As a result, disability may be assigned to those whose work involves frequent stress, increased attention, and physical activity; pensioners and patients who have undergone vascular surgery; people with heart failure or unstable angina, as well as those who have lost their ability to work by 50 percent or more.
The commission evaluates each case individually and makes a decision based on a combination of factors both on the fact of establishing disability and on its group.
Diet
In the first week after myocardial infarction, a low-calorie diet with limited fluid, salt, fat, excessive fiber and cholesterol is recommended. The diet should include foods rich in potassium and vitamin C.
In the first week, food is served pureed, in small portions 6-7 times a day. It can be:
- semolina,
- oatmeal,
- buckwheat,
- rice porridge,
- lean veal,
- chicken,
- fish,
- steamed white omelette,
- cottage cheese and kefir,
- carrot and apple salad,
- beets and cabbage,
- fruit purees,
- honey.
You can't eat:
- baked goods and sweets,
- smoked,
- fried,
- fatty,
- spicy,
- salted and pickled dishes;
- pasta,
- beans,
- coffee,
- boiled and fried eggs.
After the acute period, whole foods are introduced into the diet, but dietary restrictions should become the norm for a person.
The basis of the diet should be:
- vegetables,
- fruits,
- nuts,
- lean meats and fish,
- cereals
Smoked, canned, fried and salted foods are not recommended for consumption. It is convenient to control your weight using your body mass index (the result of dividing your weight in kg and height in meters squared).
It should be within 25-27 kg/m. In addition, the waist circumference is assessed: for men this figure should not exceed 94 cm, for women – 80 cm.
Diet for weight loss
First breakfast.
One hundred grams of low-fat cottage cheese, a cup of coffee with milk and without sugar.
Lunch.
Fresh cabbage salad (170 g) with sour cream without salt.
Dinner.
Vegetarian cabbage soup (200 ml), 90 g lean boiled meat, 50 g green peas, 100 g apples.
Afternoon snack.
One hundred grams of cottage cheese and 180 ml of rosehip decoction.
Dinner.
Boiled fish (100 g) and vegetable stew (125 g).
Before going to bed, at night.
Kefir (180 ml) and 150 g of rye bread.
Let us repeat, this is an approximate diet for one day. This diet contains 1800 kcal.
For patients without excess weight problems, the diet is significantly expanded.
They are prescribed a diet with a calorie content of 2500 - 3000 kcal
. The consumption of animal fats and carbohydrates is limited. Also 4-5 meals a day. It is useful to spend fasting days on apples (1.5 kg) or fresh cucumbers (2 kg). For “avid meat eaters”, 600 g of lean meat plus a side dish of vegetables (fresh cabbage, green peas) are even allowed.
Strongly not recommended
Doctors do not allow such patients to drink
alcohol
, even of the highest quality. It causes tachycardia and an undesirable increase in appetite. The consumption of smoked meats, fried foods, fatty sausages and sweets is absolutely unacceptable.
Breathing exercises after a heart attack
A heart attack is an acute condition associated with extreme strain on blood vessels and extreme circulatory impairment. Lack of oxygen in the heart muscle leads to its death. Unfortunately, necrosis of the heart muscle is irreversible, but nevertheless, it is necessary to create conditions for sufficient oxygen in the body for both primary and secondary prevention of the disease.
Acute pain during angina attacks, which are precursors to a heart attack, signals the myocardium about problems with oxygen.
The surest way to provide the heart muscle with enough oxygen is to reduce risk factors and breathe properly. We receive oxygen through the respiratory organs, and they must be trained and tuned to support a full respiratory cycle.
The Samozdrav breathing simulator can become a confident and powerful support in the prevention of heart attack. One of the basic positive effects of breathing training on the body is sufficient oxygen supply to the body and maintenance of normal CO2 levels. Thanks to training with Samozdrav, you can constantly maintain oxygen levels at a level that eliminates oxygen deficiency. This means a high probability of myocardial preservation and significantly reduces the risk of heart attack.
In addition to the “direct supply” of oxygen to the body, breathing training strengthens the functioning of the nervous system and corrects reactions to stress, providing peace and a smooth emotional background even under high loads.
Training with Samozdrav corrects metabolism and is effective in treating obesity. They activate metabolism by normalizing the level of oxygen in cells and tissues, normalize the excretion of metabolic products, and allow for better absorption of nutrients.
Samozdrav is indispensable for patients with hypertension. It was the treatment of this disease that became the primary goal of the creators of the breathing simulator, and today its effectiveness in treating hypertension without medications has been fully proven by research and many years of practice of use by millions of people.
Breathing training can cope with any modified risk factor for heart attack. Regular exercise will give the myocardium sufficient oxygen levels and keep the heart healthy.
Types of myocardial infarction
Since areas of muscle tissue of different sizes can undergo necrosis, cardiologists distinguish between small-focal and large-focal myocardial infarction.
Also, heart attacks are divided, depending on the depth of damage to the heart wall, into:
- transmural - pathological changes cover the entire thickness of the muscle layer;
- intramural - necrosis lies deep in the heart muscle;
- subepicardial - areas of the myocardium close to the epicardium are affected;
- subendocardial - the necrotic process is concentrated in the area of contact between the myocardium and the endocardium.
Depending on the location of the lesion, there are 2 types of myocardial infarction:
- right ventricular;
- left ventricular.
Based on clinical manifestations, cardiologists distinguish between typical and atypical myocardial infarction.
1 ECG for heart attack
2 IVF-KG for heart attack
3 Blood test for markers of heart attack
Symptoms of myocardial infarction
The severity of signs of a heart attack depends on the stage of the disease.
The pre-infarction period is not observed in all patients; it occurs in the form of exacerbation and increased frequency of angina attacks and can last hours and days, or several weeks.
The most acute period is accompanied by the development of myocardial ischemia and the formation of an area of necrosis, lasting from 20 minutes to 3 hours. The main symptom is burning or pressing pain, which often appears due to physical activity or severe stress. The pain may radiate to the left arm, shoulder, neck, shoulder blade or lower jaw.
Painful sensations vary in duration (more than 30 minutes) and are not relieved even by repeated administration of nitroglycerin.
Other symptoms of myocardial infarction:
- cold sweat;
- fear of death, severe weakness;
- shortness of breath, suffocation;
- sometimes vomiting.
First aid for myocardial infarction: if you detect at least a few of the listed symptoms, you must immediately call an ambulance! The patient must be put down and have access to fresh air. Before the arrival of the medical team, it is possible to take 1 tablet of nitroglycerin (or 1 dose of isoket) under the tongue.
The acute period of myocardial infarction begins from the moment of formation of a focus of necrosis on the myocardium and lasts from 2 to 14 days.
During this period, a person may not experience pain. Due to the formation of an area of necrosis and inflammation of the heart tissue, body temperature rises. The patient's symptoms of cardiovascular failure persist and increase. Blood pressure is low or normal.
First aid is the same: immediately go to an ambulance.
The subacute period is accompanied by the formation of scar tissue and lasts 4-8 weeks. This period of myocardial infarction is not characterized by heart pain and fever.
The patient's condition is normalized, blood pressure and pulse rate are gradually approaching normal, and manifestations of cardiovascular failure are weakening.
Post-infarction period - all symptoms disappear, laboratory parameters gradually return to normal. The body adapts to the consequences of changes in the structure of the heart muscle.
Symptoms of myocardial infarction in atypical forms of the disease:
Abdominal - symptoms are masked as signs of abdominal diseases: pain and bloating in the abdomen, nausea. Asthmatic - the patient experiences shortness of breath and attacks of suffocation. Cerebral - manifestations of brain disorders: headache, dizziness, confusion. Arrhythmic - a person complains of rapid heartbeat or irregular heartbeat. Edema form - there is pronounced peripheral edema of soft tissues.
1 Diagnosis of heart attack in MedikCity
2 Diagnosis of heart attack in “MedicCity”
3 Diagnosis of heart attack in MedikCity
Acute myocardial injury due to coronavirus disease 2021 (COVID-19) (case study)
- Babaev Maxim Alexandrovich
- Petrushin M.A.
- Dubrovin I.A.
- Kostritsa N.S.
- Eremenko Alexander Anatolievich
Summary
COronaVIrus Disease 2021 in 20% of cases is characterized by a severe and very severe course, which is accompanied by pneumonia, acute respiratory distress syndrome, and multiple organ dysfunctions. Complications from the cardiovascular system occur in 20-25% of cases and, alone or together with respiratory failure, cause deaths in 40% of patients with an unfavorable course of the disease. Acute myocardial damage (5-38%), which is most often caused by a combination of factors: infarction against the background of acute viral myocarditis and “cytokine storm”; thrombosis of coronary vessels due to covid-associated coagulopathy; vasoconstriction due to blocking of SARS-COV-2 receptors of angiotensin-converting enzyme II (ACE II) and an increase in the concentration of angiotensin II; hypoxia due to respiratory failure, manifested by heart failure, cardiac arrhythmias (~20%) and/or cases of sudden death (5-7%).
This clinical case demonstrates how a patient at particular risk (hypertension), despite positive dynamics, after therapy with human monoclonal antibodies to the interleukin-6 receptor (sarilumab), on the 8th day of her stay in the intensive care unit sudden death occurred with circulatory arrest, the cause of which was acute myocardial injury.
Key words: coronavirus, COVID-19, acute myocardial injury, multiple organ dysfunctions
Financing
.
The study had no sponsorship. Conflict of interest
.
The authors declare no conflict of interest. For citation
: Babaev M.A., Petrushin M.A., Dubrovin I.A., Kostritsa N.S., Eremenko A.A. Acute myocardial injury during coronavirus disease 2021 (COVID-19) (clinical case analysis) // Clinical and experimental surgery. Journal named after academician B.V. Petrovsky. 2021. T. 8, No. 3. P. 87-94. DOI: https://doi.org/10.33029/2308-1198-2020-8-3-87-94
COVID 19 (COronaVIrus Disease 2019) is a viral infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with a mortality rate of 3-7% [1]. The disease has a 7-14-day incubation period and is more common in males with reduced body reserves (age, comorbidity). The disease has a heterogeneous clinical course, depending on the severity of the systemic process, the endotype and/or combination of endotypes of the generalized response to the introduction of the virus (hyperinflammation, coagulation disorders, immunosuppression) and the amount of damage to the vascular endothelium and epithelial tissues [2, 3]. With an adaptive response, the appearance of individual symptoms or generally asymptomatic carriage is possible. In 20% of cases, a severe and very severe course is observed, which is accompanied by pneumonia, acute respiratory distress syndrome (ARDS), multiple organ dysfunctions, the addition of a bacterial infection and ends with multiple organ failure [2].
In addition to pulmonary complications, the most common complications are those of the cardiovascular system (CVS), which alone or together with respiratory failure cause deaths in 40% of patients with an unfavorable course of the disease. With COVID-19, patients with a history of cardiovascular disease (CVD) and hypertension are more likely to require intensive care [odds ratio (OR) 2.1; confidence interval (CI) 1.5-3.0; OK: 1.9, CI 1.5-2.5)] and have an increased risk of mortality (OR 4.7; CI 2.9-7.b) [4]. Complications from the cardiovascular system manifest themselves in the form of acute heart failure (AHF) and venous thromboembolism. Heart damage is detected in 20-25% of severe patients with COVID-19 [2]. Acute myocardial injury is a consequence of ischemic (acute coronary syndrome, ACS)/non-ischemic (myocarditis)/mixed causes (arrhythmias), manifested by increased levels of troponin and type B natriuretic peptides, and is associated with an increased risk of developing ARDS, malignant ventricular tachyarrhythmias, acute kidney injury and coagulopathy, the risk of death, and this risk is greater in patients with existing cardiovascular diseases [5, b].
This article presents an analysis of risk factors, causes of occurrence and course of COVID-19, complicated by acute myocardial injury.
Clinical case
Patient Z.,
Born in 1958, she was admitted on May 30, 2020 to the pulmonology department (for the treatment of patients with diagnosed COVID-19) of the Regional Clinical Hospital of Tver with a diagnosis of “bilateral community-acquired pneumonia (covid-pneumonia?).”
She considers herself sick since 05/23/2020, when general weakness appeared, after 2 days she turned to her local physician for help, after which she was prescribed levofloxacin, and from 05/26/2020 ceftriaxone was added to the treatment. On May 29, 2020, a multislice computed tomography (MSCT) of the chest was performed, which revealed bilateral moderate pneumonia with damage to 25-50% of the lung parenchyma, areas of compaction of the “ground glass” type (CT2 - classification according to the degree of detected changes). She did not seek inpatient care. On May 30, 2020, due to deterioration of her condition (hyperthermia up to 38.6 °C, refractory to therapy, weakness), she called an ambulance. History: stage II hypertension, stage II arterial hypertension, risk 2.
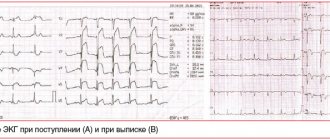
Upon admission, PCR analysis detected Covid-19 RNA; on the electrocardiogram (ECG) atrioventricular (AV) block of the first degree, corrected QT
— 413 ms; in a biochemical blood test: an increase in the level of aspartate aminotransferase (AST) - up to 111 units/l with the level of alanine aminotransferase (ALT) - 31 units/l, γ-glutamyl transpeptidase (GGT) - up to 988 units/l, serum creatinine - 134 µmol/l.
After additional studies, the patient was diagnosed with coronavirus infection caused by the COVID-19 virus, the virus was identified (U07.1); community-acquired bilateral polysegmental pneumonia (J18.8); multiple organ dysfunctions (moderate acute respiratory distress syndrome, ARDS); acute myocardial injury; acute kidney injury, AKI) and concomitant diseases in the form of stage II hypertension, stage II arterial hypertension, risk 2.
By the 3rd day of hospital stay (11th day from the onset of the disease), the patient’s condition worsened (Fig. 1):
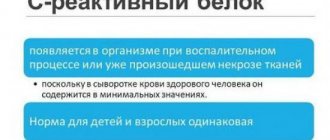
• therapy-resistant hyperthermia up to 38.7 °C persisted; an increase in the level of C-reactive protein to 85 mg/l, ferritin was detected, the content of presepsin corresponded to a moderate risk of developing systemic inflammation (487 pg/ml); there was a high tendency to microthrombosis (D-dimer, lactate dehydrogenase, LDH);
• laboratory signs of myocardial damage (troponin I) and overload of the heart cavities (NT-proBNP) were recorded; according to echocardiography (EchoCG) diastolic dysfunction of the left ventricle (LV) of the first degree (slow relaxation), a tendency to dilatation of the left atrium, signs of pulmonary hypertension (average pressure in the pulmonary artery - 25 mm Hg);
• hypoperfusion with the appearance in the analysis of acid-base status (ABS) - metabolic (4 mmol/l) lactic acidosis (pH - 7.20, BE - 16 mmol/l);
• progression of respiratory failure - decrease in SatO2 level to 86% (by pulse oximeter) when breathing atmospheric air, the appearance of tachypoea up to 26/min, on control computed tomography (CT) diffuse thickening of the lung tissue like “ground glass”, consolidation in combination with reticular changes, significant distribution of the volume of lung damage 96% (CT4).
Rice. 1.
Clinical and laboratory characteristics of the course of the disease in patient Z.
SOFA - sepsis-associated organ dysfunction scale; TnI—troponin I; PEEP - positive end-inspiratory pressure; CPAP - continuous positive airway pressure; NT-proBNP - N-terminal propeptide of natriuretic hormone; CT - computed tomography; RR - respiratory rate; FIO2—fraction of oxygen in inspired air; prone position - prone position; AST—aspartate aminotransferase; ALT - alanine aminotransferase.
Fig. 1.
Clinical and laboratory characteristics of the course of the disease in patient Z.
SOFA—scale of organ dysfunction associated with sepsis; TnI—troponin I; PEEP is the positive pressure of the end of the dose; CPAP - continuous positive airway pressure; NT-proBNP - N-terminal propeptide of natriuretic hormone; CT - computed tomography; RR—respiratory rate; FIO2 - fraction of oxygen in the inhaled air; prone position - prone position; AST—aspartate aminotransferase; ALT - alanine aminotransferase.
The patient was transferred to the intensive care unit (ICU), where she was started on non-invasive pulmonary ventilation (NIV) in CPAP mode with PEEP 8 cm H2O. and fraction of inhaled oxygen (FiO2) 50% with periodic sessions of prone position for 6-10 hours, correction of CBS and water-electrolyte balance, a change in antibiotic therapy was carried out, targeted therapy for the “cytokine storm” was started with the IL-6 antagonist drug sarulumab.
By the 7th day of stay in the ICU (18th day from the onset of the disease), it was possible to stop the hyperthermia, the patient began to notice a subjective improvement in well-being, which was accompanied by a decrease in the volume of the lesion to 86% according to CT data, with stabilization of the SatO2 indicator at 96% during inhalation 40% oxygen.
However, blood tests showed progressive signs of inflammation (leukocytosis - 25.5x109/l, segmented neutrophils - 80.5%), thrombotic microangiopathy (LDH increase almost 2 times), acute hepatic-renal dysfunction (cholestasis, cytolysis, increase in creatinine) and myocardial damage (increased levels of high-sensitivity troponin I and NT-proBNP), which was accompanied by an increase in the corrected QT
up to 420 ms, diffuse hypokinesia of the LV myocardium without local contractility disorders; reduction in ejection fraction up to 46%; LV diastolic dysfunction of the first degree. Also, echocardiography visualized LV hypertrophy, signs of chronic pulmonary heart disease (dysfunction and overload of the right sections against the background of arterial pulmonary hypertension, right ventricular hypertrophy); secondary tricuspid insufficiency degree II; left atrium dilatation; atherosclerosis of the aorta, grade I-II calcification of the aortic valve leaflets, grade I aortic regurgitation.
On June 11, 2020, the patient’s condition worsened sharply. The patient lost consciousness, did not respond to painful stimuli (Glasgow Coma Scale - 6 points), asystole was recorded on the ECG. The patient was intubated, transferred to mechanical ventilation, and full resuscitation measures were carried out, which turned out to be ineffective.
Results of pathological examination
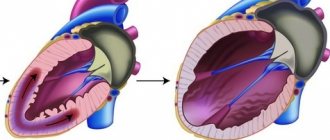
The macropreparation is shown in Fig. 2.
Rice. 2.
Macroscopic specimen of the heart of patient Z.
Heart weighing 340 g, size 11x9x7 cm. Left ventricular wall thickness 1.5 cm, right 0.3 cm, interventricular septum thickness 1.3 cm; coronary arteries are patent. Noticeable enlargement of the right side of the heart. The heart muscle on sections is pale red, under the endocardium of the anterior wall of the left ventricle and the interventricular septum there is a hemorrhage of 5x4 cm. The pulmonary arteries are passable freely, the intima is smooth, shiny
Fig. 2.
Macrodrug of the heart of a patient Z.
Heart weighing 340 grams, size 11x9x7 cm. LV wait thickness 1.5 cm, right 0.3 cm, interventricular septum thickness 1.3 cm; coronary arteries are passable. Marked expansion of the right heart. The muscle of the heart on the incisions is pale red, under the endocardium of the anterior wall of the left ventricle and interventricular septum there is a 5×4 cm hemorrhage. The pulmonary arteries are freely passable, the intima is smooth, shiny
Discussion
This clinical example confirms the data of numerous studies that COVID-19 aggravates the course of existing CVDs and leads to the development of new ones; the addition of acute myocardial injury leads to a pronounced worsening of the disease, contributes to the occurrence of multiple organ dysfunctions and is a significant risk factor for an unfavorable outcome, despite the therapy; the presence of acute myocardial damage can cause sudden circulatory arrest.
The incidence of COVID-19 complications from the cardiovascular system, according to various authors, ranges from 5 to 38% among hospitalized patients [4, 7, 8].
Complications manifest themselves in the form of acute heart failure (ACS, myocarditis, arrhythmias) and venous thromboembolism. Complications of CVS in COVID-19 are closely related to existing heart and vascular diseases, especially hypertension (23.3%) [4]. The reasons for this relationship remain to be determined. The medical history of patient Z. clearly shows that this risk factor (stage II hypertension, stage II arterial hypertension, risk 2), even without coronary heart disease and severe atherosclerosis in a woman under 65 years of age, can become a significant cause of the development of damage to the heart muscle and progression of cardiac dysfunction in COVID-19.
The literature notes that cardiovascular complications diagnosed upon admission to the hospital in 41.3% lead to a severe course of the disease and rapid transfer to the ICU [4]. In our case, this happened on the 3rd day from the moment of admission.
The causes of AHF and venous embolic complications are quite well understood, since they are a direct consequence of the main cardiovascular complications that develop during COVID-19 (ACS, myocarditis, arrhythmias, hypercoagulation, vasospasm). At the same time, the pathogenesis of acute myocardial injury is quite difficult to differentiate, since the mechanisms underlying it are of a mixed ischemic and non-ischemic nature.
The pathogenesis of cardiac injury includes vasoconstriction [due to increased angiotensin II concentrations following SARS-COV-2 blockade of angiotensin-converting enzyme II (ACE II) receptors]; impaired oxygen delivery and consumption due to respiratory failure; myocardial infarction (types 1 and 2) against the background of acute viral myocarditis and “cytokine storm”; thrombosis due to Covid-associated coagulopathy [9] (see Fig. 2).
The pathogenesis and microscopic picture of COVID-19 in patient Z. with acute myocardial injury are presented in Fig. 3.
Rice. 3.
Pathogenesis and microscopic picture of COVID-19 acute myocardial injury: 1. Fragmentation, discoid and block decomposition of myocardiocytes; 2. Necrosis of groups of myocardiocytes (absence of nuclei in cardiomyocytes). The zone of necrosis is delimited from the preserved myocardium by a zone of plethora and leukocyte infiltration (demarcation inflammation); 3. Wave-like deformation of cardiomyocytes (cause of fibrillation); 4. Arteriole thrombus; 5. Congestion, hemorrhages, stagnation of leukocytes in capillaries with access to interstitial spaces (necrosis lasts about 1 day); 6. Blocky decomposition of cardiomyocytes
Fig. 3.
Pathogenesis and microscopic picture in acute covoid myocardial damage
(hematoxylin and eosin, X100).
1. Fragmentation, discoid and blocky decomposition of myocardiocytes; 2. Necrosis of myocardiocyte groups (lack of nuclei in cardio-myocytes). The area of necrosis is delimited from the preserved myocardium by the zone of plethora and leukocyte infiltration (demarcation inflammation); 3. Wave-like deformation of cardiomyocytes (the cause of fibrillation); 4. Arterioles thrombus; 5. Plethora, hemorrhages, stasis of leukocytes in the capillaries with access to interstitial spaces (necrosis lasts about 1 day); 6. Blocky decomposition of cardiomyocytes
An important role in the pathogenesis of myocardial damage is played by the effect of SARS-CoV-2 on ACE II receptors [10]. The virus directly binds to ACE II and leads to a decrease in its expression. Thus, under the influence of the virus, the concentration of angiotensin II increases and the concentration of angiotensin 1-7, which has cardioprotective properties, decreases [10]. Angiotensin II, in turn, has a vasoconstrictor and proatherosclerotic effect [11]. In addition, the expression of TNF-α is increased, increasing the local and systemic inflammatory response and promoting further myocardial damage [12]. These effects can be both local and systemic in nature. Direct entry of the virus into cells can also lead to necrosis of cardiomyocytes and ultimately to myocardial damage [13].
In COVID-19, a “cytokine storm” caused by an uncontrolled and dysfunctional immune response by T helper cells 1 and 2 leads to the continuous activation and proliferation of various cytokines that cause apoptosis and necrosis of myocardial cells, and also predispose to plaque rupture [10].
Respiratory failure and generalized inflammation lead to a mismatch between oxygen consumption and delivery to tissues, causing hypoxia, which promotes excessive intracellular calcium deposition, leading to myocardial cell apoptosis and damage [11].
With COVID-19, an increase in the frequency of arterial thrombosis is recorded, causing strokes, ACS and episodes of sudden death. The pathogenesis of these thrombotic complications is multifactorial and repeats elements of known coagulation disorders (sepsis-induced coagulopathy, disseminated intravascular coagulation, hemaphagocytic syndrome and hemaphagocytic lymphohistiocytosis, antiphospholipid syndrome, thrombotic microangiopathy, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, heparin-induced thrombocytopenia) [14] .
Acute myocardial injury is characterized by an increase and/or decrease in the concentration of markers of myocardial damage: cardiac troponin (cTnI/cTnT) above/below the 99th percentile in the absence of clinical signs of myocardial ischemia may be accompanied by an increase in the level of B-type natriuretic peptide (BNP) or N-terminal fragment brain natriuretic peptide (NT-proBNP) [15].
With COVID-19, 2 types of myocardial damage can be suspected: primary or secondary. With primary injury, patients predominantly present with cardiac rather than respiratory complaints. The cause of the primary injury may be acute myocardial infarction (type 1), viral myocarditis, or stress-induced cardiomyopathy. Patients complain of chest pain, tests reveal elevated cardiac enzymes, and echocardiography reveals LV dysfunction and changes associated with the ST-T
on the ECG, but with normal patency of the coronary vessels on the angiogram [10].
Secondary damage is associated with direct damage to cardiomyocytes by the virus, generalized inflammation, expressed by a tendency to increase cTnI in parallel with an increase in inflammatory biomarkers (interleukin-b, D-dimer, ferritin and LDH). F. Zhou et al. [16] showed that the incidence of cTnI elevation was significantly higher among non-survivors and was a predictor of in-hospital death (odds ratio 80.07; 95% CI 10.34–620.36; p
<0.0001) [3]. The results [17, 18] noted a dynamic increase in cTnI in the group of non-survivors, with the most dramatic increase in its concentration after the 16th day from the onset of the disease and the maximum value on the 22nd day. Notably, the median time to death from symptom onset was 18.5 days (interquartile range, range 15–20 days). Similarly, the level of NT-proBNP >88.64 pc/ml in patients with severe COVID-19 is an independent factor that increases in-hospital mortality [19].
From the moment of admission to the hospital, patient Z. already showed signs of myocardial damage: increased levels of cTnI and NT-proBNP, serum transaminases, cardiac cavities, signs of pulmonary hypertension. Changes in laboratory parameters were not accompanied by characteristic complaints, there was no anamnestic information about the presence of ischemic disease, and no changes of ischemic origin were recorded on the ECG. One day before the onset of an unfavorable outcome (8th day in the ICU and 19th from the onset of the disease; this time period coincides with the data presented in the work of G. Lippi et al. [17]) an increase in the levels of cTnI and NT-proBNP was noted - almost 1.5 times from the initial values and a slight decrease in the LV ejection fraction on EchoCG, an increase in the characteristic indicators of microthrombosis and progression of the severity of organ dysfunction against this background. Clinical and laboratory characteristics are confirmed by the results of an autopsy, which revealed characteristic pathological changes in the macroanatomy of the heart (weight, size, wall thickness, presence of hemorrhage in the interventricular septum) and the structure of cardiomyocytes (fragmentation, edema, decay of cardiomyocytes). The protocol noted the appearance of a fresh area of myocardial necrosis (one day before the onset of death) with an area of perifocal inflammation and thrombus in the lumen of the arteriole, which coincided with the obtained laboratory parameters. It was possible to record a section of the myocardium with wave-like deformations of cardiomyocytes, which could be the morphological cause of the development of rhythm disturbances and sudden death [20].
Cardiac arrhythmias occur in 7-17% of cases in patients with COVID-19 and are detected significantly more often in those who require intensive care (44.4 vs. 6.9%, p
<0.001) [5, 6].
The pathogenesis of arrhythmias includes ischemia and myocardial damage caused by viral infection, hypoxia, fever, metabolic disorders, neurohormonal dysregulation and inflammatory stress, and the use of drugs that cause prolongation of the QT period (
chloroquine, hydroxychloroquine, azithromycin) [21]. It is typical that the risk of arrhythmias is greater in patients with previously diagnosed CVD. According to the literature, an increase in troponin levels along with the appearance of arrhythmia may indicate the addition of fulminant myocarditis [13].
Cases of sudden cardiac death have also been described in patients with COVID-19 [22], which can be caused by any of the cardiovascular complications described above.
Thus, in the presented clinical case, the risk factor for the development of complications from the cardiovascular system was hypertension; the cause of acute myocardial damage was ischemic and non-ischemic effects characteristic of the pathogenesis of COVID-19 (generalized inflammation, myocarditis, myocardial ischemia, microthrombosis). Acute myocardial injury was characterized by elevated levels of cardiac enzymes, echocardiographic abnormalities and was clinically expressed in the progression of organ disorders (acute renal and hepatic dysfunction), AHF and sudden cessation of hemodynamics against the background of cardiac arrhythmias. Morphological and histological confirmation of organ structure disorders and suspected causes of death in a patient with COVID-19 was obtained.
Conclusion
In the context of the current threat of a pandemic of a new coronavirus disease, patients with underlying cardiovascular pathology represent a special risk group with high rates of adverse outcomes. Complications from the cardiovascular system significantly worsen the severity of COVID-19, are closely associated with the development of multiple organ dysfunctions and are the main cause of adverse outcomes. Even a slight but persistent increase in the level of high-sensitivity troponin I and the enzyme NT-proBNP can serve as a warning signal of myocardial damage associated with direct viral effects on cardiomyocytes or with cardiomyopathy or infarction that arose during the generalized response of the body and the course of COVID-19-associated pathologies processes. The greatest danger is caused by rhythm and conduction disturbances that occur when the heart is damaged, which can be a harbinger of cases of sudden death.
Literature
1. World Health Organization, Coronavirus disease 2019 (COVID-19): situation report, 121. 2021. P. 19.
2. Madjid M. et al. Potential effects of coronaviruses on the cardiovascular system: a review // JAMA Cardiol. 2021 Mar 27.
3. Russian Cardiological Society. Guidelines for the diagnosis and treatment of diseases of the circulatory system in the context of the CO-VID-19 pandemic // Russian Journal of Cardiology. 2021. T. 25. No. 3. P. 1-20.
4. Zadori N. et al. The negative impact of comorbidities on the disease course of COVID-19 // Intensive Care Med. 2021. P. 1-3.
5. Gopinathannair R. et al. COVID-19 and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies // J. Interv. Card. Electrophysiol. 2021. P. 1-8.
6. Liu K. et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province // Chin. Med. J. (Engl.). 2021. Vol. 133, N 9. P. 1025-1031.
7. Guo T. et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2021 (COVID-19) // JAMA Cardiol. 2021 Mar.
8. Shi S. et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China // JAMA Cardiol. 2021. Vol. 5, N 7. P. 802-810.
9. Al Jaroudi WA, Hage FG Cardiovascular disease in the literature: a selection of recent original research papers // J. Nucl. Cardiol. 2021. Vol. 27, N 3. P. 712-714.
10. Tersalvi G. et al. Elevated troponin in patients with coronavirus disease 2021: possible mechanism // J. Card. Fail. 2020. Vol. 26, N 6. P. 470-475.
11. Mahajan K., Chandra KS Cardiovascular comorbidities and complications associated with coronavirus disease 2021 // Med. J. Armed Forces India. 2021 May.
12. Babapoor-Farrokhran S. et al. Myocardial injury and COVID-19: possible mechanisms // Life Sci. 2021. Vol. 253. Article ID 117723.
13. Driggin E. et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic // J. Am. Coll. Cardiol. 2021. Vol. 75, N 18. P. 2352-2371.
14. Iba T. et al. The unique characteristics of COVID-19 coagulopathy // Crit. Care. 2021. Vol. 24, N 1. P. 360.
15. Huang C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China // Lancet. 2021. Vol. 395, N 10 223. P. 497-506.
16. Zhou F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study // Lancet. 2021. Vol. 395, N 10 229. P. 1054-1062.
17. Lippi G., Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2021 (CO-VID-19): evidence from a meta-analysis // Prog. Cardiovasc. Dis. 2021 Mar.
18. Krittanawong C. et al. Coronavirus disease 2021 (COVID-19) and cardiovascular risk: a meta-analysis // Prog. Cardiovasc. Dis. 2020. Vol. 63, N 3. P. 390391.
19. Gao L. et al. Prognostic value of NT-proBNP in patients with severe COVID-19 // Respir. Res. 2021. Vol. 21, N 1. P. 83.
20. Smirnov V.P., Panysheva I.A. Pathomorphology of cardiomyocytes in sudden cardiac death // Medicine: challenges of today: materials of the III International Scientific Conference. Moscow: Buki-Vedi, 2021. pp. 43-46.
21. Kochi AN et al. Cardiac and arrhythmic complications in patients with COVID-19 // J. Cardiovasc. Electrophysiol. 2021. Vol. 31, N 5. P. 1003-1008.
22. Marijon E. et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study // Lancet Public Health. 2021. Vol. 5, N 8. P. e437-e443.
Complications of myocardial infarction
The overwhelming majority of deaths from heart attack occur in the first hours and days and are associated with complications of myocardial infarction:
- Life-threatening arrhythmias - ventricular tachycardia, ventricular fibrillation, cardiac arrest;
- Cardiogenic shock is a condition that develops with extensive damage to the left ventricular myocardium and is characterized by a progressive decrease in blood pressure and impaired blood supply to vital organs;
- A cardiac aneurysm and its rupture are thinning of the heart wall and its protrusion under the pressure of blood in the ventricles. If an aneurysm ruptures, tamponade and cardiac arrest occur;
- Cardiac tamponade is a deadly complication of a cardiac aneurysm in which blood leaks into the pericardial cavity after the aneurysm ruptures. As a result of the rapid filling of the pericardium with blood, the heart can no longer carry out its pumping function and stops;
- Rupture of the interventricular septum;
- Acute heart failure (pulmonary edema);
- The occurrence of complete atrioventricular block and a decrease in heart rate to 20-30 per minute.
Lower IM
AMI with isolated ST-segment elevation in leads II, III, and aVF is usually associated with damage to the right coronary artery (RCA) or the distal circumflex artery (CA). A rather unpleasant feature of AMI with damage to the inferior wall is that the ST segment elevation associated with the infarction can develop over a long period, up to two weeks, to become evident on the ECG [4]. The inferior wall can be supplied with blood from the right coronary artery (in 80% of cases) or from the OA, which is a branch of the left coronary artery.
ST segment elevation in lead III is greater than in lead II, and ST segment depression of more than one mm in leads I and aVL suggests damage to the RCA, which supplies the inferior wall. In the case of blood supply to the lower wall from the OA, the rise of the ST segment in lead III does not exceed the rise in lead II. In this case, either an elevation of the ST segment in aVL is observed, or it is located on the isoline [6, 7].
Diagnosis of myocardial infarction
First, the doctor examines the patient and collects information from the patient or his relatives about the nature and duration of pain, the strength and frequency of attacks, medications taken, and their effect on well-being.
Next, laboratory and instrumental diagnostics of myocardial infarction are carried out:
- general and biochemical blood tests (usually in a hospital setting);
- study of cardiac-specific enzymes and markers of damage to the heart muscle (usually in a hospital setting);
- electrocardiography;
- echocardiography (ultrasound of the heart);
- coronary angiography (in a hospital setting).
Treatment of myocardial infarction
Intensive care measures for acute myocardial infarction may include:
- administration of thrombolytic agents to dissolve the blood clot and restore blood flow in the myocardium;
- pain relief (narcotic analgesics are often used);
- stabilization of blood pressure;
- the use of antianginal, antiarrhythmic drugs, anticoagulants, antiplatelet agents, beta blockers, ACE inhibitors, etc.
Surgical techniques are often used in the treatment of myocardial infarction:
- angioplasty (expansion of a narrowed vessel using a balloon catheter);
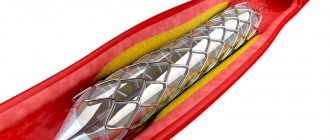
- coronary stenting (installation of a stent at the site of narrowing of the coronary artery, after its expansion with a balloon);
- shunting (suturing a shunt that bypasses the narrowed area).
Post-hospital treatment of myocardial infarction (outpatient management after discharge from hospital) also includes a number of activities:
- observation by a cardiologist;
- pharmacotherapy;
- blood pressure and heart rate control;
- diet;
- avoiding stress, overwork and strain;
- recommended physical activity;
- rejection of bad habits.
Diagnosis of myocardial infarction and treatment of patients who have suffered a myocardial infarction at MedikCity
At the MedicCity clinic, the diagnosis of myocardial infarction and treatment of patients who have suffered a myocardial infarction, as well as those suffering from other cardiac diseases, are carried out at the highest professional level.
Our cardiologists are armed with the best expert-level equipment, extensive scientific knowledge and the latest developments!
We have reasonable prices and an individual approach. You can find out the schedule of specialists and the cost of services by calling: +7 (495) 604-12-12.
"MedicCity" is the right choice!
REHABILITATION AT HOME
Using the recommendations of exercise therapy instructors, patients should regularly do a set of exercises at home. This includes morning exercises and walking. But we must not forget about self-monitoring (measure blood pressure, pulse). For hiking, it will be useful to purchase a pedometer - this way you will know the results of your training, and possibly your achievements. Do not forget about alternating loads and rest.
To quickly say goodbye to the disease, a person needs to forget that he is sick, believe in himself and his speedy and final recovery. Your loved ones should also work on this. A calm, friendly atmosphere should reign in the house. A person must feel necessary, useful, believe in his return to normal life, perhaps to his favorite job.
Some patients who suffered a heart attack belong to the 3rd and 4th functional class
. Their rehabilitation program differs from the program of the first two. Its goal is to provide the patient with such a level of activity that he can care for himself independently. Perhaps - do simple housework or work in an intellectual field (at home).
Physical rehabilitation of this group of patients takes place at home (physical therapy, massage, walks in the yard, slowly climbing a few steps up the stairs). But the patient must be visited periodically by a therapist and a cardiologist.