When is Triazavirin indicated?
Triazavirin is an antiviral drug. It was developed by institutes of two academies of sciences, RAS and RAMS. Chupakhin O.N., Kiselev O.I., Charushin V.N. worked on the medicine. The product has undergone clinical trials in 11 large accredited clinical centers. The registration certificate was issued in 2014.
The drug belongs to the azoloazine class. It is the only drug from this group. The active component of the drug is riamilovir, which directly fights viral agents.
Triazavirin is indicated for the treatment and prevention of respiratory diseases.
The drug is effective for:
- Flu (H3N2, H5N1, H1N1, H5N2, H9N2);
- Parainfluenza;
- Corey;
- Respiratory sensitial virus;
- Dengue fever, West Nile fever;
- Tick-borne encephalitis.
The product can be used for preventive and therapeutic purposes for COVID 19.
The medication is indicated only for adults. It is not used in pediatric practice due to insufficient evidence base.
ENALAPRIL
special instructions
The issue of using dual blockade of the RAAS (for example, by simultaneous use of an ACE inhibitor with an angiotensin II receptor antagonist) must be decided on a case-by-case basis with careful monitoring of renal function.
Caution must be exercised in patients with reduced blood volume (including when used simultaneously with diuretics, in conditions of limited salt intake, with hemodialysis, diarrhea, vomiting), in whom a sudden and pronounced decrease in blood pressure may develop in response to the use of an ACE inhibitor. In patients with mild CHF, with or without chronic renal failure, symptomatic hypotension is usually not observed. The development of arterial hypotension is most likely in patients with more severe CHF due to the use of high doses of diuretics, hyponatremia or functional renal failure. In these patients, treatment should begin under medical supervision until the optimal dose adjustment of Enalapril and/or diuretic is achieved. Similar tactics can be applied to patients with coronary artery disease and cerebrovascular diseases, in whom an excessive decrease in blood pressure can lead to myocardial infarction or cerebrovascular accident. If severe arterial hypertension develops, the patient must be placed in a horizontal position and, if necessary, an intravenous infusion of 0.9% sodium chloride solution should be started. Transient arterial hypotension is not a contraindication for continuing treatment with Enalapril after stabilization of blood pressure and replenishment of blood volume. In some patients with CHF with normal or low blood pressure, an additional decrease in blood pressure may occur when using the drug Enalapril. This is usually not a reason to discontinue the drug. In case of development of arterial hypotension, it is necessary to reduce the dose and/or discontinue the diuretic and/or enalapril.
As with all vasodilators, ACE inhibitors should be used with caution in patients with left ventricular hypertrophy and valvular obstruction and should be avoided in cases of cardiogenic shock and hemodynamically significant obstruction. In case of impaired renal function (creatinine clearance less than 80 ml/min), careful monitoring of potassium and creatinine levels in the blood serum is necessary. In patients with renal failure, it may be necessary to reduce the dose and/or frequency of dosing. Some patients with bilateral renal artery stenosis or arterial stenosis of a solitary kidney experience increased serum urea and creatinine concentrations. The changes are usually reversible and return to normal after stopping treatment.
In some patients who did not have renal disease before treatment, slight and transient increases in serum urea and creatinine concentrations were observed when enalapril was used concomitantly with diuretics. In such cases, it may be necessary to reduce the dose and/or discontinue enalairil and/or diuretic.
In patients with bilateral renal artery stenosis or stenosis of the artery of a solitary kidney taking ACE inhibitors. there is an increased risk of developing arterial hypotension and renal failure. Only moderate changes in plasma creatinine concentration can indicate a decrease in renal function. In such patients, treatment should begin with small doses under medical supervision, gradually selecting an individual dose and monitoring the concentration of creatinine in the blood serum.
There is no experience with the use of enalapril in patients who have recently undergone kidney transplantation. Therefore, the use of this drug in such patients is not recommended.
The use of Enalapril in patients with liver failure usually does not require dose adjustment. Rarely, taking an ACE inhibitor is associated with a syndrome ranging from the development of cholestatic jaundice to the development of fulminant liver necrosis. If symptoms of jaundice or increased liver enzyme activity occur in patients taking ACE inhibitors, discontinue drug therapy and conduct appropriate evaluation. Cases of neutropea/agranulocytosis, thrombocygopenia and anemia have been reported in patients taking ACE inhibitors. In patients with normal renal function and no other complications, neugropenia rarely develops. The drug Enalapril should be used with great caution in patients with connective tissue diseases (including systemic lupus erythematosus, scleroderma) who are simultaneously receiving immunosuppressive therapy, allopurinol or procainamide, as well as a combination of these factors, especially with existing renal dysfunction. These patients may develop severe infections that do not respond to intensive antibiotic therapy. If patients still take the drug Enalapril, it is recommended to periodically monitor the number of leukocytes in the blood. The patient should be warned that if any signs of infection appear, they should consult a doctor.
Angioedema of the face, extremities, tongue, vocal cords and/or larynx has been reported with the use of ACE inhibitors, including enalapril. This can happen at any time during treatment. In such cases, treatment with Enalapril should be stopped immediately, and the patient should be under medical supervision until the corresponding symptoms completely disappear. Even in cases where only difficulty in swallowing occurs without difficulty breathing, patients may require long-term medical observation because Therapy with antihistamines and glucocorticosteroids may not be enough. Angioedema, associated with swelling of the larynx and tongue, can be fatal in very rare cases. Patients with swelling of the tongue, vocal cords, or larynx may develop airway obstruction, especially in patients with a history of respiratory surgery. In cases of airway obstruction, it is necessary to carry out appropriate therapy as soon as possible, including subcutaneous administration of epinephrine (0.3-0.5 ml of epinephrine (adrenaline) solution in a ratio of 1:1000) and/or take the necessary measures to ensure the conductivity of the airways ( intubation or tracheostomy).
Among black patients receiving ACE inhibitor therapy, the incidence of angioedema is higher than among patients of other races. Patients with a history of angioedema not associated with the use of ACE inhibitors have an increased risk of developing angioedema when taking any ACE inhibitor.
There are reports of life-threatening anaphylactic reactions in patients taking ACE inhibitors. during the desensitization procedure with hymenoptera venom. Such reactions can be avoided if you temporarily stop taking ACE inhibitors before desensitization begins. The use of ACE inhibitors should be avoided in patients receiving bee venom immunotherapy.
In rare cases, life-threatening anaphylactoid reactions have been observed in patients taking ACE inhibitors during LDL apheresis with dextrin sulfate. If LDL-afsrez is used, AIF inhibitors should be temporarily replaced with other drugs to treat hypertension and heart failure.
Anaphylactoid reactions have been reported in patients undergoing hemodialysis using high-flux polyacrylonitrile membranes (AN69). In these cases, it is recommended to use a different type of membrane for dialysis or use an antihypertensive drug of a different pharmacotherapeutic group.
When using Enalapril in patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, blood glucose concentrations should be regularly monitored during the first month of therapy. Cough has been reported with the use of ACE inhibitors. Usually the cough is non-productive and persistent and stops after discontinuation of ACE inhibitors. In the differential diagnosis of cough, cough caused by the use of ACE inhibitors must also be taken into account.
In patients undergoing surgery or during general anesthesia with drugs that cause hypotension, ACE inhibitors may block the formation of angiotensin II in response to compensatory release of renin. Before surgery (including dental procedures), it is necessary to warn the surgeon-anesthesiologist about the use of Enalapril.
Hyperkalemia may develop during therapy with ACE inhibitors, including enalapril. Risk factors for hyperkalemia include renal failure, | old age (over 65 years), diabetes mellitus, some concomitant conditions (decrease in BCC, acute heart failure in the stage of decompensation, metabolic acidosis), simultaneous use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, amiloride), as well as potassium supplements or potassium-containing substitutes for table salt and the use of other drugs that increase the content of potassium in the blood plasma (for example, heparin). The use of potassium supplements, potassium-sparing diuretics or potassium-containing table salt substitutes, especially in patients with renal failure, can lead to a significant increase in plasma potassium levels. Hyperkalemia can cause serious heart rhythm disturbances, sometimes fatal. The simultaneous use of Enalairil with any of the drugs listed above should be carried out with caution and should be accompanied by regular monitoring of potassium levels in the blood plasma. The simultaneous use of lithium and Enalapril is usually not recommended.
The drug Enalapril, like other ACE inhibitors, has a less pronounced antihypertensive effect in patients of the Negroid race compared to representatives of other races. possibly due to low renin activity in hypertensive patients in this population.
Sudden cessation of enalapril does not lead to the development of withdrawal syndrome.
How is Triazavirin good for COVID-19?
According to the mechanism of action, the drug is active against RNA viruses. The COVID-19 genome consists of a single strand of RNA.
The drug is recommended for use for preventive purposes. It allows you to stop the proliferation of microorganisms that have penetrated the host cells. The medication is especially recommended for people who are in contact with patients with COVID-19 (relatives of coronavirus patients, doctors, nurses, etc.).
Triazavirin for moderate coronavirus can be used as part of complex therapy. The drug reduces the severity of symptoms and shortens the duration of therapy. Can be used as monotherapy for mild forms of coronavirus infection.
Features of the impact of the funds
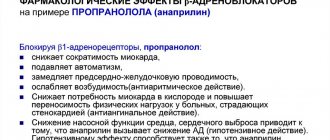
The effect of drugs that belong to the group of ACE inhibitors is based on the fact that they slow down the body's production of angiotensin II. This hormone causes blood vessels to constrict, which leads to increased blood pressure. Under the influence of active substances in the composition of the drugs, the vessels remain dilated, which reduces the load on the heart muscle and lowers blood pressure.
Most ACE inhibitor drugs are intended for oral use. But if intensive therapy is necessary in severe cases, drugs in this group can be administered intravenously.
Indications for prescribing ACE inhibitors are varied. In addition to the treatment of arterial hypertension of any origin, drugs are prescribed for the following pathologies:
- Myocardial infarction in the acute phase. When used, it is possible to reduce the rate of tissue destruction.
- Coronary insufficiency. With the help of funds it is possible to reduce the risk of relapse.
- Ischemic stroke. During an emergency, blood pressure always increases and needs to be normalized.
ATP inhibitors are prescribed for kidney problems and to reduce certain symptoms of diabetes and migraines. When treating arterial hypertension, the doctor may prescribe an ACE inhibitor in combination with other drugs that lower blood pressure in order to obtain quick results.
There are many contraindications for the use of medications whose main purpose is to lower blood pressure. Therefore, they should be prescribed by a doctor taking into account the patient’s condition. It is not recommended to use ATP inhibitors during pregnancy and lactation.
Side effects
Like any medicine, Triazavirin can have unwanted effects. List of consequences of use:
- eosinophilia;
- allergic reaction (rashes on the skin);
- headache;
- dyspepsia (thin stool, vomiting, nausea, bloating, gastralgia, dry oral mucosa);
- the appearance of red blood cells, bacteria, epithelial cells in the urine;
- increased levels of liver enzymes (ALT, AST).
- impotence.
If symptoms appear and intensify, you should consult a doctor to adjust your therapy. In case of an overdose, severe abdominal pain, dyspepsia, vomiting, and nausea occur.
Renipril®
Caution must be exercised when prescribing Renipril® to patients with reduced circulating blood volume (as a result of diuretic therapy, limiting salt intake, hemodialysis, diarrhea and vomiting) - the risk of a sudden and pronounced decrease in blood pressure is increased after using even the initial dose of an ACE inhibitor. Transient arterial hypotension is not a contraindication for continuing treatment with the drug after stabilization of blood pressure. In case of a repeated pronounced decrease in blood pressure, the dose should be reduced or the drug discontinued.
The use of high-permeability dialysis membranes increases the risk of developing an anaphylactic reaction. Correction of the dosage regimen on days free from dialysis should be carried out depending on the level of blood pressure.
Before and during treatment with ACE inhibitors, periodic monitoring of blood pressure, blood parameters (concentration of hemoglobin, potassium, creatinine, urea, liver enzyme activity), and protein in the urine is necessary.
Patients with severe heart failure, coronary heart disease and cerebrovascular disease, in whom a sharp decrease in blood pressure can lead to myocardial infarction, stroke or impaired renal function, should be carefully monitored.
Sudden cessation of treatment does not lead to withdrawal syndrome (a sharp rise in blood pressure).
For newborns and infants who have been exposed in utero to ACE inhibitors, it is recommended to conduct careful monitoring for timely detection of a pronounced decrease in blood pressure, oliguria, hyperkalemia and neurological disorders that may be due to a decrease in renal and cerebral blood flow with a decrease in blood pressure caused by ACE inhibitors. In oliguria, it is necessary to maintain blood pressure and renal perfusion by administering appropriate fluids and vasoconstrictors.
Before studying the functions of the parathyroid glands, the drug should be discontinued. Alcohol enhances the hypotensive effect of the drug.
Before surgery (including dentistry), the surgeon/anesthesiologist must be warned about the use of ACE inhibitors.
In the presence of renal failure, the excretion of the active metabolite may be reduced, leading to an increase in its concentration in the blood plasma. Such patients may need to be prescribed smaller doses of the drug.
In patients with arterial hypertension and unilateral or bilateral renal artery stenosis, an increase in urea and creatinine in the blood serum is possible.
In such patients, renal function should be monitored during the first few weeks of therapy. It may be necessary to reduce the dosage of the drug.
The balance of risk and potential benefit should be taken into account when prescribing Renipril® to patients with coronary and cerebrovascular insufficiency due to the risk of increased ischemia with excessive arterial hypotension.
The drug should be prescribed with caution to patients with diabetes mellitus due to the risk of developing hyperkalemia.
Patients with a history of angioedema may have an increased risk of developing angioedema during treatment with Renipril.
Patients with significant autoimmune diseases, such as systemic lupus erythematosus or scleroderma, are at increased risk of developing neutropenia or agranulocytosis while taking Renipril®.
Caution is recommended when prescribing Renipril® for the treatment of chronic heart failure in patients receiving cardiac glycosides and/or diuretics.
Similar products
The drug has non-structural analogues. List of similar medications:
- Anaferon - the medicine contains antibodies to human interferon gamma, which increase the overall immune status, is produced in the form of tablets, and is inferior in effectiveness to Triazavirin;
- Arbidol - produced in tablet forms or powder for making a suspension, contains umifenovir;
- Viferon - available in rectal suppositories, is highly effective against viral infections, can be used at any stage of the disease, is relatively safe; used in pediatric practice, including neonatology;
- Kagocel is an interferon inducer that stimulates the synthesis of its own interferons.
Triazavirin or Arbidol - which is better?
There is a lot of controversy surrounding these two drugs. The mechanism of action of drugs is aimed at preventing the proliferation of viral agents. Triazavirin fights viruses more effectively, unlike Arbidol. The disadvantage of riamilovir is:
- Lack of children's uniform;
- Toxicity of the drug during simultaneous use with purine analogues;
- There is a load on the liver and kidneys;
- Insufficient research has been conducted regarding the effectiveness and possible adverse effects.
Triazavirin is a relatively new antiviral drug that is currently still under study. Today it is recommended for use against coronavirus infection, all strains of influenza viruses, tick-borne encephalitis and other pathogens. The medicine copes well with infections, but has a number of side effects. The drug is also prohibited for children, pregnant women, lactating women, and patients with liver and kidney pathologies. These restrictions significantly narrow the range of its use, because older people, children, and patients with chronic diseases are more susceptible to viral infections.
Renipril
Caution must be exercised when prescribing the drug to patients with reduced blood volume (as a result of diuretic therapy, limiting salt intake, hemodialysis, diarrhea and vomiting) - there is an increased risk of a sudden and pronounced decrease in blood pressure after using even the initial dose of an ACE inhibitor. Transient hypotension is not a contraindication for continuing treatment with the drug after stabilization of blood pressure. In case of a repeated pronounced decrease in blood pressure, the dose should be reduced or the drug discontinued.
If an excessive decrease in blood pressure develops, the patient is transferred to a horizontal position with a low head, and, if necessary, a 0.9% NaCl solution and plasma-substituting drugs are administered.
The use of high-flow dialysis membranes increases the risk of developing an anaphylactic reaction. Correction of the dosage regimen on days free from dialysis should be carried out depending on the level of blood pressure.
Before and during treatment with ACE inhibitors, it is necessary to monitor blood pressure, blood parameters (Hb, K+, creatinine, urea, liver enzyme activity), and protein in the urine.
Patients with decompensated CHF, ischemic heart disease and cerebral vascular diseases, in whom a sharp decrease in blood pressure can lead to myocardial infarction, stroke or impaired renal function, should be carefully monitored. Sudden cessation of treatment does not lead to withdrawal syndrome (a sharp rise in blood pressure).
Patients with a history of angioedema have an increased risk of developing it when taking ACE inhibitors.
For newborns and infants who have been exposed in utero to ACE inhibitors, it is recommended to conduct careful monitoring for timely detection of a pronounced decrease in blood pressure, oliguria, hyperkalemia and neurological disorders that may be due to a decrease in renal and cerebral blood flow with a decrease in blood pressure caused by ACE inhibitors. With oliguria, it is necessary to maintain blood pressure and renal perfusion by administering appropriate fluids and vasoconstrictor drugs.
In patients with reduced renal function, the single dose should be reduced or the intervals between doses should be increased.
Before studying the functions of the parathyroid glands, enalapril should be discontinued.
Caution should be exercised when performing physical exercise or in hot weather (risk of dehydration and excessive reduction in blood pressure due to a decrease in blood volume).
Before surgery (including dentistry), the surgeon/anesthesiologist must be warned about the use of ACE inhibitors.
During treatment with the drug, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions (dizziness is possible, especially after taking the initial dose of an ACE inhibitor in patients taking diuretic drugs).
Enalapril Renipril tablet 10 mg x20
Trade name: Renipril International name: Enalapril Pharmacological group: ACE inhibitor Pharmacological group according to ATC: C09AA02. Enalapril Pharmacodynamics: An ACE inhibitor is an antihypertensive drug, the mechanism of action is associated with a decrease in the formation of angiotensin II from angiotensin I, a decrease in the concentration of which leads to a direct decrease in aldosterone secretion. At the same time, peripheral resistance, systolic and diastolic blood pressure, post- and preload on the myocardium decrease. Dilates arteries to a greater extent than veins, while no reflex increase in heart rate is observed. Reduces bradykinin degradation, increases Pg synthesis. The hypotensive effect is more pronounced at high plasma renin concentrations than at normal or reduced levels. A decrease in blood pressure within therapeutic limits does not affect cerebral circulation; blood flow in the vessels of the brain is maintained at a sufficient level even against the background of reduced blood pressure. Strengthens coronary and renal blood flow. With long-term use, hypertrophy of the LV myocardium and myofibril of the walls of resistive arteries decreases, prevents the progression of CHF and slows down the development of LV dilatation. Improves blood supply to ischemic myocardium. Reduces platelet aggregation. Extends life expectancy in patients with CHF, slows down the progression of LV dysfunction in patients who have had myocardial infarction without clinical manifestations of HF. Has some diuretic effect. Reduces intraglomerular hypertension, slowing the development of glomerulosclerosis and the risk of chronic renal failure. Enalapril is a “prodrug”: as a result of its hydrolysis, enalaprilat is formed, which inhibits ACE. The onset of the hypotensive effect when taken orally is 1 hour, it reaches a maximum after 4-6 hours and lasts up to 24 hours. In some patients, therapy is required for several weeks to achieve an optimal blood pressure level. In CHF, a noticeable clinical effect is observed with long-term treatment - 6 months or more.
Pharmacokinetics: After oral administration, absorption is 60%. Eating does not affect absorption. It is metabolized in the liver to form the active metabolite enalaprilat, which is a more effective ACE inhibitor than enalapril. Plasma protein binding of enalaprilat is 50-60%. TCmax of enalapril - 1 hour, enalaprilat - 3-4 hours. Enalaprilat easily passes through histohematic barriers, excluding the BBB, a small amount penetrates the placenta and into breast milk. T1/2 of enalaprilat - 11 hours. Excreted mainly by the kidneys - 60% (20% - in the form of enalapril and 40% - in the form of enalaprilat), through the intestines - 33% (6% - in the form of enalapril and 27% - in the form of enalaprilat) . It is removed by hemodialysis (rate 62 ml/min) and peritoneal dialysis.
Indications for use: Arterial hypertension (symptomatic, renovascular, including with scleroderma, etc.), stage I-III CHF, prevention of coronary ischemia in patients with LV dysfunction, asymptomatic LV dysfunction.
Contraindications: Hypersensitivity to enalapril or other ACE inhibitors, pregnancy, lactation.
With caution: history of angioedema during therapy with ACE inhibitors, hereditary or idiopathic angioedema, aortic stenosis, cerebrovascular diseases (including cerebrovascular insufficiency), coronary artery disease, coronary insufficiency, severe autoimmune systemic connective tissue diseases (including including SLE, scleroderma), suppression of bone marrow hematopoiesis, diabetes mellitus, hyperkalemia, bilateral renal artery stenosis, stenosis of the artery of a single kidney, condition after kidney transplantation, renal and/or liver failure, Na+-restricted diet, conditions accompanied by a decrease in blood volume (in including diarrhea, vomiting), old age, age under 18 years (safety and effectiveness of use have not been studied).
Dosage regimen: Orally, regardless of food intake. For monotherapy of arterial hypertension, the initial dose is 5 mg once a day. If there is no effect, after 1-2 weeks the dose is increased by 5 mg. After the initial dose, patients should be under medical supervision for 2 hours and an additional 1 hour until blood pressure stabilizes. If necessary and sufficiently well tolerated, the dose can be increased to 40 mg/day in 1-2 doses. After 2-3 weeks, switch to a maintenance dose - 10-40 mg/day, divided into 1-2 doses. For moderate hypertension, the average daily dose is about 10 mg. The maximum daily dose of the drug is 40 mg. If prescribed to patients concomitantly receiving diuretics, treatment with the diuretic should be discontinued 2-3 days before enalapril is prescribed. If this is not possible, then the initial dose of enalapril should be 2.5 mg/day. For patients with hyponatremia (serum Na+ concentration less than 130 mmol/l) or serum creatinine concentration more than 0.14 mmol/l, the initial dose is 2.5 mg 1 time per day. Renovascular hypertension: initial dose - 2.5-5 mg/day. The maximum daily dose is 20 mg. In severe cases of arterial hypertension, intravenous administration is possible (see Enalaprilat), carried out only in a hospital setting. For CHF, the initial dose is 2.5 mg once, then the dose is increased by 2.5-5 mg every 3-4 days in accordance with the clinical response to the maximum tolerated dose (depending on blood pressure), but not higher than 40 mg/day, once, or in 2 doses. In patients with low systolic blood pressure (less than 110 mm Hg), therapy should begin with a dose of 1.25 mg. Dose selection should be carried out over 2-4 weeks or shorter periods. The average maintenance dose is 5-20 mg/day in 1-2 doses. In the elderly, a more pronounced hypotensive effect and prolongation of the drug's action time are more often observed, which is associated with a decrease in the rate of elimination of enalapril, therefore the recommended initial dose for the elderly is 1.25 mg. For asymptomatic dysfunction of the LV function - 2.5 mg 2 times a day. The dose is selected taking into account tolerability up to 20 mg/day, divided into 2 doses. In chronic renal failure, cumulation occurs when filtration decreases to less than 10 ml/min. With CC 80-30 ml/min, the dose is usually 5-10 mg/day, CC 30-10 ml/min - 2.5-5 mg/day, less than 10 ml/min - 1.25-2.5 mg/day only on dialysis days. The duration of treatment depends on the effectiveness of the therapy. If the decrease in blood pressure is too pronounced, the dose of the drug is gradually reduced.
Side effects: From the cardiovascular system: excessive decrease in blood pressure, orthostatic collapse, rarely - chest pain, angina pectoris, myocardial infarction (usually associated with a pronounced decrease in blood pressure), arrhythmias (atrial brady- or tachycardia, atrial fibrillation), palpitations, thromboembolism of the branches of the pulmonary artery . From the nervous system: dizziness, fainting, headache, weakness, insomnia, paresthesia, anxiety, depression, confusion, fatigue, drowsiness (2-3%), very rarely when used in high doses - nervousness, depression, paresthesia . From the senses: disorders of the vestibular apparatus, hearing and vision impairment, tinnitus. From the digestive system: dry mouth, loss of appetite, dyspeptic disorders (nausea, diarrhea or constipation, vomiting, abdominal pain), intestinal obstruction, pancreatitis, impaired liver function and bile secretion, hepatitis, jaundice. From the respiratory system: nonproductive “dry” cough, interstitial pneumonitis, bronchospasm, shortness of breath, rhinorrhea, pharyngitis. Allergic reactions: skin rash, angioedema of the face, limbs, lips, tongue, glottis and/or larynx, dysphonia, exfoliative dermatitis, exudative erythema multiforme (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell's syndrome) , pemphigus (pemphigus), pruritus, urticaria, photosensitivity, serositis, vasculitis, myositis, arthralgia, arthritis, stomatitis, glossitis. From laboratory parameters: hypercreatininemia, increased urea concentration, increased activity of “liver” transaminases, hyperbilirubinemia, hyperkalemia, hyponatremia, decreased Hb and hematocrit, increased ESR, thrombocytopenia, neutropenia, agranulocytosis (in patients with autoimmune diseases), eosinophilia. From the urinary system: impaired renal function, proteinuria. Other: alopecia, decreased libido, flushing of the face.
Overdose: Symptoms: excessive decrease in blood pressure, up to the development of collapse, myocardial infarction, acute cerebrovascular accident or thromboembolic complications, convulsions, stupor. Treatment: the patient is transferred to a horizontal position with a low headboard. In mild cases, gastric lavage and ingestion of saline solution are indicated; in more serious cases, measures aimed at stabilizing blood pressure are indicated: intravenous administration of a 0.9% NaCl solution, plasma substitutes, if necessary, intravenous administration of angiotensin II, hemodialysis (enalaprilat elimination rate - 62 ml/min).
Interaction: Enhances the effect of ethanol, slows down the excretion of Li+. Weakens the effect of drugs containing theophylline. The hypotensive effect is reduced by NSAIDs and estrogens, and enhanced by diuretics, other antihypertensive drugs (beta-blockers, methyldopa, nitrates, BMCA, hydralazine, prazosin), drugs for general anesthesia, ethanol. Potassium-sparing diuretics and potassium-containing drugs increase the risk of developing hyperkalemia. Drugs that cause bone marrow suppression increase the risk of developing neutropenia and/or agranulocytosis. Immunosuppressants, allopurinol, cytostatics increase hematotoxicity.
Special instructions: Care must be taken when prescribing to patients with reduced blood volume (as a result of diuretic therapy, limiting salt intake, hemodialysis, diarrhea and vomiting) - the risk of a sudden and pronounced decrease in blood pressure is increased after using even the initial dose of an ACE inhibitor. Transient hypotension is not a contraindication for continuing treatment with the drug after stabilization of blood pressure. In case of a repeated pronounced decrease in blood pressure, the dose should be reduced or the drug discontinued. If an excessive decrease in blood pressure develops, the patient is transferred to a horizontal position with a low head, and, if necessary, a 0.9% NaCl solution and plasma-substituting drugs are administered. The use of high-flow dialysis membranes increases the risk of developing an anaphylactic reaction. Correction of the dosage regimen on days free from dialysis should be carried out depending on the level of blood pressure. Before and during treatment with ACE inhibitors, it is necessary to monitor blood pressure, blood parameters (Hb, K+, creatinine, urea, liver enzyme activity), and protein in the urine. Patients with decompensated CHF, ischemic heart disease and cerebral vascular diseases, in whom a sharp decrease in blood pressure can lead to myocardial infarction, stroke or impaired renal function, should be carefully monitored. Sudden cessation of treatment does not lead to withdrawal syndrome (a sharp rise in blood pressure). Patients with a history of angioedema have an increased risk of developing it when taking ACE inhibitors. For newborns and infants who have been exposed in utero to ACE inhibitors, it is recommended to conduct careful monitoring for timely detection of a pronounced decrease in blood pressure, oliguria, hyperkalemia and neurological disorders that may be due to a decrease in renal and cerebral blood flow with a decrease in blood pressure caused by ACE inhibitors. With oliguria, it is necessary to maintain blood pressure and renal perfusion by administering appropriate fluids and vasoconstrictor drugs. In patients with reduced renal function, the single dose should be reduced or the intervals between doses should be increased. Before studying the functions of the parathyroid glands, enalapril should be discontinued. Caution should be exercised when performing physical exercise or in hot weather (risk of dehydration and excessive reduction in blood pressure due to a decrease in blood volume). Before surgery (including dentistry), the surgeon/anesthesiologist must be warned about the use of ACE inhibitors. During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions (dizziness is possible, especially after taking the initial dose of an ACE inhibitor in patients taking diuretic drugs).
Manufacturer: Pharmstandard-Leksredstva OJSC, Russia Registration certificate holder: Pharmstandard-Leksredstva OJSC, Russia Release form: 20 mg tablets, blister packs Belongs to VED Minimum pharmacy assortment Preferential dispensing: DLO Dispensing conditions: by prescription Registration data: P N000084/ 01 from 06.28.2010 Status of the registration certificate: valid Pharmaceutical article number: FSP 42-0550-0293-06
2nd generation drugs
Second-generation ACE inhibitors are used very often today in the treatment of arterial hypertension. This is due to the combination of high efficiency and safety of medications. The main difference from first-generation drugs is that the effect after administration occurs no earlier than 20 minutes later. But at the same time it persists for a longer time - up to 5-8 hours.
Enalapril is often prescribed to treat elderly patients. The drug has the additional ability to prevent the formation of blood clots and remove cholesterol. Other representatives of the group of second-generation ACE inhibitors:
- Perindopril. An effective and safe drug for use in the complex treatment of hypertension, as well as the prevention of heart attack and stroke.
- Lisinopril. The drug is prescribed to patients without kidney pathologies, since it is completely excreted in the urine. The active substance does not accumulate in adipose tissue, so the medicine is prescribed when high blood pressure occurs due to excess weight.
- Ramipril. The medicine is considered effective only in the treatment of arterial hypertension at the initial stage of development. It is often prescribed for long-term use.
Renipril® HT
During therapy with Renipril® GT, the patient's condition should be regularly monitored, especially at the beginning of treatment.
Arterial hypotension and
electrolyte imbalance
When using antihypertensive drugs, some patients may develop symptomatic arterial hypotension (even several hours after taking the first dose). Patients should be monitored for clinical signs of fluid and electrolyte imbalance, such as dehydration, hyponatremia, hypochloremic alkalosis, hypomagnesemia, or hypokalemia, which may occur with concomitant diarrhea or vomiting. In such patients, monitoring of serum electrolytes is necessary. The drug should be prescribed with extreme caution to patients with coronary artery disease or cerebrovascular diseases, in whom a pronounced decrease in blood pressure can lead to myocardial infarction and/or stroke.
If arterial hypotension develops, the patient should be laid down, legs elevated and, if necessary, a 0.9% sodium chloride solution should be administered. Transient arterial hypotension when taking Renipril® GT is not a contraindication to its further use. After normalization of blood pressure and replenishment of blood volume, therapy can be resumed in lower doses or each of the components of the drug can be used in monotherapy.
Aortic or mitral stenosis/HOCM
As with all drugs that have a vasodilating effect, ACE inhibitors should be administered with caution to patients with left ventricular outflow tract obstruction.
Renal dysfunction
The drug should not be prescribed to patients with renal failure (creatinine clearance less than 80 ml/min) until the selection of individual components of the drug shows that the required doses are present in this dosage form. In some patients with arterial hypertension, without any evidence of a history of kidney disease, when treated with enalapril in combination with a diuretic, a slight and transient increase in plasma urea and serum creatinine concentrations may occur; in such cases, treatment with Reniprilk® GT should be discontinued . In the future, it is possible to resume therapy in lower doses or each of the components of the drug can be used in monotherapy.
In some patients with bilateral renal artery stenosis and stenosis of the artery of a solitary kidney, when treated with ACE inhibitors, an increase in the concentration of urea in the blood plasma and creatinine in the serum was observed, these changes were usually reversible, as a rule, the indicators returned to normal after cessation of therapy. This pattern of changes is most likely in patients with impaired renal function.
When using ACE inhibitors for renovascular arterial hypertension, there is also a high risk of a pronounced decrease in blood pressure, so treatment in such patients begins with a low dose of Renipril® GT under the supervision of a physician.
Liver failure
Rarely, when treated with ACE inhibitors, a syndrome is observed that begins with cholestatic jaundice or hepatitis, which progresses to fulminant liver necrosis, sometimes with death. The mechanism of this syndrome has not been studied. Patients who develop jaundice or a marked increase in the activity of liver transaminases during treatment with ACE inhibitors should discontinue the ACE inhibitors and prescribe appropriate auxiliary therapy. The patient must be under medical supervision.
Surgery/general anesthesia
During major surgery or general anesthesia with the use of drugs that cause an antihypertensive effect, enalaprilat blocks the formation of angiotensin II caused by the compensatory release of renin. If a pronounced decrease in blood pressure develops, explained by a similar mechanism, it can be corrected by increasing the volume of blood volume. It is necessary to warn the surgeon/anesthesiologist that the patient is taking ACE inhibitors.
Hypersensitivity reactions/angioedema
When using ACE inhibitors, including enalapril, in rare cases and during any period of therapy, the development of angioedema of the face, upper and lower extremities, lips, mucous membranes, tongue, vocal folds and/or larynx may be observed (see section “Adverse reactions”). action"). If symptoms appear, the drug should be stopped immediately and the patient should be observed until signs of edema completely disappear. If the swelling affects only the face and lips, it usually resolves on its own, although antihistamines may be used to treat symptoms.
Angioedema, accompanied by swelling of the larynx, can be fatal. Swelling of the tongue, vocal folds, or larynx can lead to airway obstruction. When such symptoms appear, emergency treatment is required, including subcutaneous administration of epinephrine (adrenaline) and/or ensuring airway patency. The patient should be under medical supervision until symptoms disappear completely and permanently.
In patients of negroid
races taking ACE inhibitors, angioedema developed more often than in patients of other races.
Patients with a history of angioedema not associated with taking ACE inhibitors may be at greater risk of developing angioedema during therapy with ACE inhibitors (see section "Contraindications").
In patients taking ACE inhibitors and mammalian target of rapamycin (mTOR) inhibitors, estramustine, racecadotril, gliptins, an increased risk of developing angioedema was observed (see section "Interaction with other drugs").
In patients taking thiazide diuretics, hypersensitivity reactions may occur even in the absence of a history of allergic reactions or bronchial asthma. Relapses and worsening severity of systemic lupus erythematosus have been reported in patients taking thiazide diuretics.
In rare cases, intestinal edema develops during therapy with ACE inhibitors. In this case, patients experience abdominal pain as an isolated symptom or in combination with nausea and vomiting, in some cases without previous angioedema of the face and with normal levels of C1-esterase. The diagnosis was made using abdominal computed tomography, ultrasound, or surgery. Symptoms disappeared after stopping the ACE inhibitors. Therefore, in patients with abdominal pain receiving ACE inhibitors, when carrying out differential diagnosis, it is necessary to take into account the possibility of developing angioedema of the intestine (see section “Side effects”).
Anaphylactoid reactions during desensitization with an allergen from Hymenoptera venom
In rare cases, patients taking ACE inhibitors have developed life-threatening anaphylactoid reactions during desensitization with hymenoptera venom allergen. To avoid corresponding reactions, ACE inhibitor therapy should be temporarily discontinued before each desensitization therapy session.
Anaphylactoid reactions during low-density lipoprotein (LDL) apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during LDL apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued before each LDL apheresis procedure.
Patients on hemodialysis
It should be borne in mind that when treated with Renipril® GT in patients who are indicated for hemodialysis, the development of anaphylactoid reactions (swelling of the face, flushing of the skin, marked decrease in blood pressure, shortness of breath) is possible due to the use of high-throughput filter membranes consisting made of polyacrylonitrile (for example, high-flow membranes AN69®). It is recommended to use other types of dialysis membranes for hemodialysis or other classes of antihypertensive agents.
Kidney transplant
There is no experience with the use of enalapril in patients after kidney transplantation. Treatment with enalapril in patients after kidney transplantation is not recommended.
Neutropenia/agranulocytosis
There are reports of the development of neutropenia/agranulocytosis, thrombocytopenia and anemia in patients receiving treatment with ACE inhibitors. The risk of neutropenia likely depends on the dose and the clinical condition of the patient. Neutropenia may occur more often in patients with reduced renal function, especially if there is a concomitant connective tissue disease (systemic lupus erythematosus, scleroderma) or when treated with immunosuppressants, allopurinol or procainamide, as well as a combination of these complicating risk factors. Some of these patients developed severe infectious diseases, which in some cases did not respond to intensive antibiotic therapy. When using enalapril in such patients, it is advisable to carry out monitoring of blood leukocytes and a complete blood count before treatment, every 2 weeks in the first three months of treatment, and then regularly. The patient should be strongly advised to report any symptom of an infectious disease (eg, sore throat, fever) to the doctor; in this case, the leukocyte blood count should be monitored. If neutropenia (less than 1000/mm3) is suspected or detected, which is reversible, the drug Renipril® GT and other drugs taken simultaneously should be discontinued (see section “Interaction with other drugs”).
Double blockade of the RAAS
Cases of hypotension, syncope, stroke, hyperkalemia and renal dysfunction (including acute renal failure) have been reported in susceptible patients, especially when used concomitantly with drugs that affect this system. Therefore, double blockade of the RAAS by combining an ACE inhibitor with an ARA II or aliskiren is not recommended.
Combination with aliskiren is contraindicated in patients with diabetes mellitus and/or moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) (see sections “Contraindications” and “Interaction with other drugs”) . The simultaneous use of ACE inhibitors and ARB II is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Lithium preparations
The simultaneous use of lithium, enalapril and diuretics is not recommended (see section “Interaction with other drugs”).
Cough
Cough may occur during therapy with ACE inhibitors. As a rule, this is a dry cough, is permanent and disappears after stopping treatment. Cough associated with the use of ACE inhibitors should be considered in the differential diagnosis of cough.
Hyperkalemia
(see section "Interaction with other drugs")
During treatment with Renipril® GT, an increase in potassium levels in the blood serum is possible, especially in patients with chronic renal failure, diabetes mellitus, with simultaneous use of potassium-sparing diuretics (for example, spironolactone, eplerenone, amiloride, triamterene), potassium supplements or potassium-containing salt substitutes, as well as in patients taking other drugs that lead to an increase in potassium levels in the blood serum (for example, heparin); this effect is usually attenuated by thiazide diuretics due to increased potassium excretion. If the simultaneous use of the above drugs is necessary, then regular monitoring of potassium levels in the blood serum is recommended (see section “Interaction with other drugs”).
Metabolic and endocrine effects
Thiazide therapy may impair glucose tolerance. It may be necessary to adjust the dose of insulin or oral hypoglycemic agents (see section “Interaction with other drugs”). When treated with thiazides, latent diabetes mellitus can manifest itself.
Thiazides can reduce the excretion of calcium by the kidneys and cause a transient increase in serum calcium without visible disturbances in its metabolism. Severe hypercalcemia may be a sign of latent hyperparathyroidism. Due to the effect of thiazides on calcium metabolism, their use may distort the results of testing the function of the parathyroid glands, therefore, before testing the function of the parathyroid glands, the thiazide diuretic should be discontinued.
Increases in plasma cholesterol and triglyceride concentrations may also be associated with thiazide diuretic therapy.
In some patients, therapy with thiazide diuretics may lead to the development of hyperuricemia and/or exacerbation of gout. However, enalapril may increase renal excretion of uric acid and thereby reduce the hyperuricemic effect of hydrochlorothiazide.
Liver diseases
Thiazide diuretics should be used with caution in patients with impaired liver function and/or progressive liver disease, since even small changes in water and electrolyte balance can lead to hepatic coma.
Anti-doping test
Hydrochlorothiazide may cause a positive result during doping control.
Acute myopia and closed-angle glaucoma
Hydrochlorothiazide, being a sulfonamide derivative, can cause an idiosyncratic reaction in the form of acute transient myopia and acute secondary angle-closure glaucoma. Symptoms include: sudden loss of visual acuity or eye pain, usually occurring within hours to weeks of starting hydrochlorothiazide therapy. If left untreated, acute angle-closure glaucoma can lead to permanent vision loss. Treatment: Stop taking hydrochlorothiazide as soon as possible. If intraocular pressure remains uncontrolled, emergency medical treatment or surgery may be required. Risk factors for the development of acute angle-closure glaucoma are: a history of an allergic reaction to sulfonamides or penicillin.
Non-melanoma skin cancer
Two pharmacoepidemiological studies using data from the Danish National Cancer Registry demonstrated an association between hydrochlorothiazide use and an increased risk of non-melanoma skin cancer (NMSC) basal cell carcinoma and squamous cell carcinoma. The risk of developing NMSC increased with increasing total (cumulative) dose of hydrochlorothiazide. A possible mechanism for the development of NMSC is the photosensitizing effect of hydrochlorothiazide.
Patients taking hydrochlorothiazide as monotherapy or in combination with other drugs should be aware of the risk of developing NMSC. It is recommended that such patients undergo regular skin examination to identify any new suspicious lesions as well as changes in existing skin lesions.
Any suspicious skin changes should be reported to your doctor immediately. Suspicious areas of skin should be examined by a specialist. To clarify the diagnosis, histological examination of skin biopsies may be required.
To minimize the risk of developing NMSC, patients should be advised to follow preventive measures, such as limiting exposure to sunlight and UV rays, and using appropriate protective equipment.
In patients with a history of non-melanoma skin cancer, it is recommended to reconsider the use of hydrochlorothiazide.
Side effects
From the nervous system and sensory organs: dizziness, headache, weakness, increased fatigue, decreased libido.
From the cardiovascular system and blood (hematopoiesis, hemostasis): hypotension, collapse, neutropenia, hyperkalemia.
From the gastrointestinal tract: nausea, impaired liver function (increased activity of liver transaminases, bilirubin levels), diarrhea.
Other: cough, skin rashes, renal dysfunction, proteinuria, muscle spasms, angioedema.