First aid for an angina attack
Angina almost always accompanies ischemic heart disease. However, with other cardiovascular diseases (thickening of the heart muscle, anemia), attacks of angina are also recorded. Symptoms primarily include severe chest pain and shortness of breath. And the reasons are oxygen starvation of the heart tissue due to atherosclerotic narrowing of the lumen of the coronary vessels or severe vascular spasm. The trouble is that the disease manifests itself suddenly, so both the patient and his relatives must know what to do during an attack of angina, how to provide first emergency aid. It is worth remembering that this disease is a pre-infarction condition, and therefore requires qualified diagnosis and treatment. Now you can undergo a consultation and a set of preparatory examinations when registering for a course of enhanced external counterpulsation or shock wave therapy of the heart absolutely free of charge!
Promotion
Just until the end of autumn, undergo a free consultation and a set of preparatory examinations* when registering for a course of enhanced external counterpulsation or shock wave therapy of the heart.**
Send a request
* Check the details of the Promotion by phone. **Has contraindications; consultation with a doctor is required.
Enhanced external counterpulsation (EECP) Cardiac shock wave therapy (SWTS)
Hurry up to apply, the promotion period is limited.
Methods for diagnosing angina pectoris
Laboratory and instrumental examination methods help to give the patient an accurate diagnosis. A blood test can determine:
- the level of total cholesterol and so-called lipid fractions;
- blood clotting indicators;
- glucose level;
- markers of systemic inflammation;
- the presence in the blood of other substances that affect cholesterol metabolism and the level of oxygen saturation in the blood.
Among the instrumental diagnostic methods, the following are of particular importance:
- ECG at the peak of an angina attack;
- daily ECG monitoring, which allows to identify abnormalities in the functioning of the heart in various external conditions;
- EchoCG – reveals ischemic changes and disturbances in the process of contraction of the heart muscle;
- bicycle ergometry - identifies the maximum level of load for the patient without the risk of symptoms of angina pectoris;
- stress echocardiography using ultrasound waves;
- computed tomography of the heart structure;
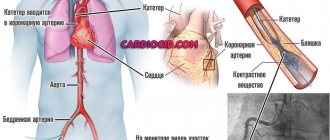
- coronary angiography - radiography with the introduction of a contrast agent.
Based on the results obtained, a treatment course is developed and a decision is made on surgical intervention.
Signs of an angina attack
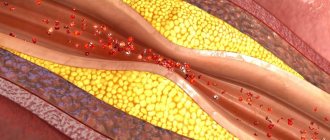
Since the vessels supplying blood to the heart are narrowed due to atherosclerotic plaques, only a small physical or emotional stress is enough for the heart muscle to feel a lack of oxygen and nutrients. At this time, lactic acid is produced in the tissues, which causes pain.
If, after you have worked physically or been over-excited, you experience heart pain, know that these are the first signs of illness. As it develops, less and less stress will be required to cause an attack. In severe cases, signs of angina appear when walking at an average pace for a distance of 200 meters or climbing one floor.
Coronary heart disease (CHD), or angina (questions and advice for the patient)
Coronary heart disease is a disease that occurs due to insufficient blood supply to the heart due to narrowing of the lumen of blood vessels. Pain during angina appears most often in the center of the chest, but it can also be on the left, in the region of the heart, and can radiate (“give”) to the neck, lower jaw, left arm, between the shoulder blades. The sensation may be squeezing or pressing. Some patients feel as if something is falling on their chest. Sometimes, along with the pain, there is a feeling of lack of air, the inability to breathe. Angina almost always appears during stress - physical or emotional. It can begin during fast walking, running, climbing stairs, lifting heavy objects, or during severe stress or emotional distress. In later stages, when the disease becomes more severe, pain may also occur at rest. It is very important that if such sensations occur, be sure to consult a doctor as soon as possible!
What you need to know about coronary heart disease?
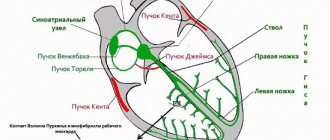
In order to function properly, the heart needs oxygen and nutrients. The blood supply to the heart is carried out through the arteries that surround the heart, like the crown, and are therefore called coronary. Blood enters the coronary arteries from the aorta, after which it is delivered through smaller vessels to the working myocardial cells. The diameter of the coronary arteries is very small - they are no thicker than a cocktail straw (3-5 mm), but disruption of their patency can cause serious damage to health. The main cause of impaired arterial patency is atherosclerosis (from the Greek words “ather” - gruel and “sclerosis” - hardening). The name accurately reflects the essence of the process - the accumulation of soft deposits on the walls of the arteries - lipids (fats, such as cholesterol), the subsequent proliferation of dense connective tissue and hardening - calcification. As a result, the arteries lose their elasticity and become stiff. Lipid (fat) deposits, called atherosclerotic plaques, bulging into the lumen of blood vessels lead to narrowing of the lumen or even blockage of the arteries. The mechanisms of the early stages of the development of the atherosclerotic process, due to which plaques and narrowing of the coronary vessels develop, have not yet been fully clarified. Nevertheless, today it has been proven that atherosclerosis develops, among other things, in response to damage to the vascular wall from the inside (damage or dysfunction of the endothelium). This can be caused by a number of reasons, in particular, smoking, a significant increase in blood lipid (cholesterol) levels, high Blood Pressure, psycho-emotional stress, viral or bacterial infection. Hereditary predisposition also plays a role. Narrowing (stenosis) of one or more coronary arteries by atherosclerotic plaque(s) reduces the supply of blood and oxygen to the heart muscle and causes myocardial ischemia (from the Greek words “ishe” - retain and “hemo” - blood). It is the lack of blood and oxygen that causes the pain a person feels during an angina attack.
What is angina and how to recognize it?
Angina pectoris is the main symptom of chronic coronary heart disease (CHD)
Angina is an acute feeling of discomfort in the chest (a feeling of squeezing, tightness, burning, pain), forcing a person to stop physical activity. Regardless of what kind of exercise causes angina, the attack should go away after stopping the exercise and/or taking nitroglycerin (spray or tablets). If the discomfort in the chest does not go away after this, immediately call an ambulance; a myocardial infarction may develop.
If any unpleasant sensations appear in the chest, you should consult a doctor for a routine, “standard” (ECG, blood tests, medical examination) or more in-depth examination (ECG or echocardiogram with stress, ECG monitoring throughout the day, coronary angiography of the arteries of the heart) . Coronary angiography is performed for severe manifestations of angina pectoris in order to clarify the possibility of using surgical methods to improve the blood supply to the heart, stenting or bypass surgery. (see more detailed information on “poststenta.rf”).
What to do if you have an angina attack?
Angina is a cry from the heart for help. Although an insufficient amount of blood flows through the heart artery narrowed by the plaque, under resting conditions it is enough to provide the heart muscle with oxygen supplied by the blood.
Therefore, the first action for angina pectoris is to stop the load that caused the attack. Second action: if the attack does not go away within 2-3 minutes with rest, you need to take 1 tablet of nitroglycerin, placing it under the tongue. It is more convenient to use nitroglycerin in the form of a spray. Nitroglycerin is quickly absorbed, enters the blood and causes dilation of the blood vessels of the heart. After 1-2 minutes the attack should stop. Short-term attacks of angina go away on their own when you stop exercising or after taking nitroglycerin for 2-3 minutes, sometimes up to 8-10 minutes.
Remember! You should always have an adequate supply of your medications with you!
With coronary heart disease (more precisely, with atherosclerosis, which narrows the arteries of the heart), myocardial ischemia occurs (bleeding of part of the heart muscle) of varying durations - from several minutes to 1 hour or more.
Ischemia for more than 40 minutes is most likely associated with the development of arterial thrombosis (blockage by a blood clot). This is a sure sign of a beginning or already occurring myocardial infarction (death of cells of part of the heart muscle).
What to do in this situation?
At the first sign of a heart attack, call 911. It is best to start treatment within the first hour after symptoms appear. Waiting increases heart damage and reduces the chance of survival. It is essential to prevent the artery from narrowing within 90 minutes to minimize the consequences.
Before the ambulance arrives, provide access to more oxygen: unfasten the collar, open the window.
Be sure to stop any physical activity, lie down with the head of the bed raised or sit in a chair with armrests, and relax as much as possible.
Do not eat, do not drink, do not smoke.
If pain persists, continue taking nitroglycerin every 7-10 minutes. If there is no pain, you do not need to take nitroglycerin.
Do not panic! Emotional stress can further increase ischemia.
Strictly follow the recommendations of the emergency doctor after an attack.
How to deal with angina pectoris?
It has been proven that modern treatment methods can prevent the progression of the disease, prolong life and maintain health.
To do this, first of all, it is necessary to change your lifestyle and give up bad habits, eliminating risk factors:
If there is hypertension, the blood pressure level should be brought to figures less than 130 mm. Hg / 90 mm. rtst.
Quit smoking
Stop drinking alcohol
Monitor your diet using a diet for patients with coronary artery disease
Get rid of excess weight
Consult your doctor for recommendations on physical activity
Non-drug methods (diet, physical training, blood pressure control, weight control) significantly increase the effectiveness of drug therapy. But the persistence of risk factors such as smoking, alcohol, hypertension, excess weight, low physical activity, and diabetes mellitus can reduce the effect of drug prevention!
What medications should be taken to relieve angina attacks?
Once you are diagnosed with angina, you may need to take medications indefinitely, long-term. Even if you have had coronary angioplasty (sometimes called PCI, PTCA, stenting) or coronary artery bypass grafting, you will need to continue taking your medications afterwards.
To reduce the number of angina attacks, there are a number of drugs called antianginal drugs.
Remember that prescribing, discontinuing and changing dosages for the treatment of angina pectoris is carried out only by your attending physician .
The purpose of these drugs is to prolong your life and eliminate (or significantly reduce) the symptoms of angina pectoris. Symptoms will decrease due to normalization of blood flow, pressure, pulse, and restoration of the metabolic state of heart cells.
What can the doctor prescribe for you? (only if indicated and after examinations!).
Fast-acting nitrates (spray or tablets).
These drugs are used to relieve angina attacks. The essence of their action is that they quickly dilate the blood vessels of the heart, which relieves pain. You should always have nitroglycerin spray (or tablets) with you. This could save your life. But remember that these drugs only relieve the symptoms of angina pectoris, but do not cure it. If you take them often and regularly, their effect may weaken. Be sure to tell your doctor how many times a day/week you use nitrates.
Beta blockers
They act on the sympathetic nervous system, somewhat slow down the heart and lower blood pressure. It is very important to take them constantly, for a long time, and under no circumstances stop taking them without consulting your doctor. Beta blockers are used to prevent angina attacks, but not to relieve them.
Calcium antagonists
They also prevent the development of angina attacks. Taking these drugs leads to dilation of the arteries, including the arteries of the heart. As a result, blood flow improves, the load on the heart decreases, and more blood flows to the heart. Calcium antagonists also lower blood pressure.
Myocardial cytoprotectors
These drugs have a fundamentally different mechanism of action. They prevent the development of attacks by influencing metabolic disorders caused by a lack of oxygen directly in the heart cells.
Without affecting blood pressure and pulse, these drugs enable the heart to work without ischemia by switching the heart to more economical use of scarce oxygen. They switch metabolic processes to use glucose as “fuel” for the heart, rather than fatty acids as is usually the case. With the same amount of work, the heart requires less oxygen (by about 20-30%) to oxidize (burn) “fuel” for the normal functioning of heart cells
If after your doctor prescribes/discontinues any pills you feel worse, do not make any independent adjustments to your treatment, but, if possible, contact your doctor as quickly as possible.
What to tell the doctor
Describe how you feel. Fill out the form on the back.
Show your blood pressure and heart rate monitoring diary.
Tell us in detail about the pain - where it hurts, what it is like, when it occurs, how you relieve it.
If you have had any examinations or tests, bring the results to your doctor.
What to ask your doctor
Do I need to take medications? When? How many times a day? What dosage?
When to come next time?
What to do if it gets worse?
Do you need a diet? Which? How much fluid to drink?
Are there any restrictions on physical activity?
It is important to control angina pectoris
Note how you feel in your diary every day, this is very important for controlling angina.
Download the Angina Control mobile application from the AppStore or GooglePlay. It is easy to use and will help you better evaluate the effectiveness of therapy.
Information for patients.
Fill out the questionnaire before your doctor’s appointment; this will make communication with a specialist more effective.
Gracheva Z.M. — cardiologist OGBUZ ARB
Print Email
- Back
- Forward
Symptoms of an angina attack
External signs of the disease are similar to the symptoms of vegetative-vascular dystonia, pinched nerve, osteochondrosis, pleurisy, so you should know how an angina attack differs from them.
Often the manifestations are quite individual. In different patients, an attack can last 1-15 minutes. And even pain is perceived in different ways: as sharp, squeezing, aching, radiating to the jaw, shoulder, throat, accompanied by a burning sensation.
Painful sensations occur:
- when walking fast, climbing stairs;
- physical activity (especially after a heavy meal);
- emotional tension, excitement, worries, stress;
- sudden movement from a warm room to a cold one;
- at rest at night.
An attack of angina is accompanied by additional symptoms and signs. If, when pain occurs, your eyes darken, profuse sweat appears, your limbs become cold, you feel that you are about to faint, call a doctor immediately - first emergency aid is necessary! In women, these symptoms include stomach pain with nausea and heartburn, shortness of breath and a feeling of weakness.
Caring for patients with hypertension
Hypertension is a disease in which the main clinical symptom is increased blood pressure.
According to the recommendations of the World Health Organization, high blood pressure is considered to be, regardless of age, pressure above 139/89 mmHg. Art.
In its development, the disease goes through 3 stages. All three stages are characterized by complaints of headache, poor sleep, increased irritability, decreased memory and performance.
A dangerous complication of hypertension is the development of a hypertensive crisis, which is characterized by: severe headache, dizziness, nausea, vomiting, and visual disturbances. Hypertensive crisis is a serious condition, dangerous in its consequences and requiring immediate medical attention.
Treatment and care of patients with arterial hypertension can be difficult due to some misconceptions of patients suffering from this disease. Patients think that:
- Hypertension can be cured.
- Once blood pressure has returned to normal, treatment can be stopped.
- If there are no symptoms, then there is no disease.
- Any change in well-being is caused by a change in blood pressure, so you need to either take an extra pill or, conversely, skip a dose.
- If you follow a diet and exercise, you do not need to take medications.
- Blood pressure can be determined by how you feel.
Rules for caring for patients with hypertension
Optimal working and rest conditions
- Prevention of stressful situations.
- Creating conditions for physical and mental peace.
- Creating conditions for good sleep.
- Prohibition of night work
- Prohibition of work associated with strong emotional stress and attentional stress.
- Moderate, regular exercise is helpful for lowering blood pressure. Short-term isotonic exercises, such as walking, are indicated. Isometric loads are not shown, since during their implementation blood pressure increases.
Organization of proper nutrition
- Losing excess weight.
- Limit the consumption of fried and fatty foods.
- Limiting the caloric content of food (should not exceed the daily standard requirement).
- Limit the consumption of table salt to 6 g/day.
- A dairy-vegetable diet enriched with magnesium salts helps lower blood pressure. Foods high in calcium, low in fat and caffeine are beneficial. It is necessary to exclude products containing licorice root.
Monitoring the general condition of the patient
- Determination of the patient's well-being.
- Measuring blood pressure as often as recommended by your doctor, but at least once a day;
- Measuring the amount of fluid drunk and excreted.
Monitoring compliance with drug treatment requirements
- Monitoring the constant, timely and full use of medications prescribed by a doctor.
- Prevention of orthostatic collapse while taking drugs that lower blood pressure: carefully change the patient’s body position from lying or sitting.
First aid for an angina attack
Has the disease manifested itself for the first time? The most correct decision would be to call an ambulance. If you have an attack of angina, the signs and symptoms of which appear during walking or physical exertion, stop immediately and rest. It is best to take a comfortable position, sitting or lying down, and take nitroglycerin, which is usually used to relieve angina attacks.
If you take nitroglycerin 3 times, and it does not give the usual relief in 20 minutes - the symptoms do not go away, then you are close to a heart attack and require immediate medical help, possibly with transfer to intensive care.
Emergency care for symptoms of an angina attack also includes self-massage - it helps relieve acute pain, tension and an instinctive feeling of fear. Massage the left chest, neck, and back of the head. Pay attention to the knee, shoulder, and wrist joints.
Care for varicose veins of the lower extremities
Varicose veins of the lower extremities - enlargement of the superficial veins of the legs - are associated with weakness of the vein walls and a number of predisposing factors. The disease is characterized by the appearance of protrusions and nodular swellings on the lower extremities along the saphenous veins.
Main symptoms of the disease:
- leg pain;
- a feeling of warmth and burning in the legs along the veins;
- heaviness in the legs;
- itching;
- night cramps in the legs;
- swelling in the evening;
- dilated veins;
- darkening and thickening of the skin of the legs;
- trophic ulcers.
Risk factors:
- genetic predisposition;
- floor;
- hormonal influences (pregnancy);
- weight gain;
- lifestyle (hard physical work, prolonged standing, high ambient temperature).
Treatment principles:
- recommendations regarding lifestyle and body position;
- wearing elastic bandages, tights or stockings;
- use of venotonic drugs;
- sclerotherapy;
- surgical treatment (removal of affected veins).
Care Tips:
- keep your legs elevated during sleep and rest;
- change the position of your legs more often or periodically walk at a fast pace if you have to sit or stand for a long time;
- rinse your feet with cool water after a warm bath or shower;
- It is not recommended to take hot baths;
- prolonged exposure to the sun should be avoided;
- You need to wear shoes with medium-height heels (3 - 4 cm);
- It is not recommended to wear tight clothes and tight belts, stockings and socks with tight elastic bands;
- exercise regularly;
- walking and swimming;
- Sports not recommended: tennis, weightlifting, high jumping;
- a balanced diet with a reduced number of calories compared to the norm; in case of excess weight, the load on the veins increases;
- the use of elastic stockings or elastic bandages with varying degrees of compression;
- venotonic drugs.
How to relieve an angina attack at home?
If an attack occurs while you are lying down, you need first aid. First of all, they helped you sit down and lower your legs down. Unbutton your collar, ask them to open a window in the house, apartment, or other room where you are and take nitroglycerin.
If you feel weak, pale, or have cold sweats, measure your blood pressure. If it is reduced, there is no need to take nitroglycerin. In this case, it is better to relieve the attack with aspirin. But the effect of validol is causing controversy in the world of medicine: doctors are increasingly inclined to believe that it is ineffective.
To provide effective first aid during an angina attack, always keep baralgin, sedalgin, and analgin in your first aid kit. If you have symptoms such as headaches, take one of these medications. For elevated heart rates, anaprillin is recommended.
Caring for patients with chronic heart failure
Heart failure is a pathological condition that develops as a result of a decrease in the contractile function of the heart muscle. Always accompanied by disruption of blood flow and metabolic processes in organs and tissues. Occurs in a wide variety of diseases.
There are three stages of chronic heart failure. At the first stage, patients complain of fatigue, poor sleep, and palpitations. At the second stage, faster fatigue and shortness of breath occur even with little physical exertion. In some cases, the patient is bothered by palpitations, swelling of the legs in the evening, and the appearance of blue discoloration on the lips, fingertips, nose and ears. In other cases, the patient develops a cough with phlegm and shortness of breath. In the third stage, all the above symptoms increase. Cyanosis and shortness of breath bother the patient even in a state of complete rest. He is forced to sit all day, as shortness of breath increases when lying down. Such a patient can even sleep only while sitting.
Rules for caring for patients with chronic heart failure
- Limiting physical activity. At the first stage, light physical work without significant stress is acceptable. At the second stage, physical work and physical education are excluded, it is recommended to reduce the length of the working day and introduce an additional day of rest. At the third stage, home rest is indicated, and in severe cases, semi-bed rest.
- The patient may get tired even after slight physical activity (washing, eating). Having noticed fatigue, it is necessary to give the patient the opportunity to rest.
- Creating conditions for deep and restful sleep. Sleep duration should be at least 8 hours a day.
- Compliance with diet (therapeutic diet No. 10). Easily digestible food with reduced daily energy value (1400-1500 kcal). Fractional frequent feeding, in small portions. Limitation of table salt intake: the daily dose should not exceed 2-3 g. At the third stage, the amount of salt is reduced to 0.5-1 g per day. Alcohol, strong tea and coffee are excluded from the diet. In case of severe edema, the amount of fluid is limited to 800 ml - 1 liter per day. The diet includes foods rich in potassium: dried apricots, baked potatoes, etc.
- Careful care of the skin, which, in the presence of edema, becomes thinner, loses elasticity, and becomes vulnerable to infection.
- Monitoring the timely and complete intake of medications prescribed by the attending physician.
- Daily measurement of the patient’s body weight, amount of fluid drunk and excreted.
- Monitoring the patient's stool frequency. If there is no stool for more than 2 days, as prescribed by the doctor, it is necessary to give a cleansing enema.
- Monitoring the position of the patient's body in bed or in a chair. If the patient is indicated for bed rest, he should be in a bed with the head end elevated. If the patient is sitting or half-sitting in a chair, it is necessary to help him find a comfortable position with the help of pillows.
- When the patient is sitting, place a bench or low stool under his feet so that his legs are raised as much as possible, but in a way that is comfortable for the patient. Elevating your legs reduces swelling of the lower extremities.
- Measurement of pulse rate, respiration and blood pressure as prescribed by a doctor, but at least once a day.
Rules for taking nitroglycerin
As part of first aid for an angina attack, you can use both tablets (to relieve an attack outside the home) and drops. The medicine is dropped onto a piece of sugar, which is placed under the tongue and wait until it dissolves. Check the dosage with your doctor, but remember: you cannot take more than 3 tablets (drops) in 15 minutes.
You may feel dizzy, because the effect of the medicine is to dilate blood vessels and reduce pressure. Therefore, before taking, take a comfortable position, sitting or lying down.
FAQ
Why is angina pectoris dangerous?
If the patient neglects his health and refuses medical care, the frequency of attacks may increase and the pain may intensify. A further decrease in the lumen can cause acute oxygen starvation and the development of myocardial infarction with a poor prognosis.
How to relieve an angina attack at home?
When the first sensations of pain appear, you should immediately stop working or moving, take a sitting or lying position, put a nitroglycerin tablet under your tongue, which should always be at hand. If your eyes darken and perception deteriorates, you should ask others for help. It is important to try to record the condition preceding the attack and the duration of the last one in order to report it to the attending physician.
How to determine angina?
Among the characteristic signs of angina pectoris are severe pressing pain in the heart area with a return to the peripheral parts of the body, noticeable fluctuations in pulse and pressure. The attack occurs with sudden physical or psycho-emotional stress and subsides within 15-20 minutes. Only the attending physician can carry out differentiated diagnostics and accurately name the cause of the disease.
Why is it important to see a doctor?
Even if there was only one attack, this is a sufficient reason to undergo diagnostics in a qualified cardiology clinic. Angina pectoris can lead to myocardial infarction and even death. Only an experienced cardiologist will promptly identify the problem and prescribe treatment that will help you avoid the fatal risk.
You will receive the full range of qualified cardiological services for the diagnosis, treatment and prevention of cardiovascular diseases at the CBCP Center for Circulatory Pathology, equipped with expert-class European equipment.
Diets for diseases of the cardiovascular system
Diet No. 10
Indications: diseases of the cardiovascular system without clinical signs of heart failure.
Purpose of administration: improvement of blood circulation, functioning of the cardiovascular system, liver and kidneys, normalization of metabolism, sparing the cardiovascular system and digestive organs.
General characteristics: slight decrease in energy value due to fats and partly carbohydrates. Significantly limiting the amount of sodium chloride, reducing fluid intake. The content of substances that excite the cardiovascular and nervous systems, irritate the liver and kidneys, unnecessarily burden the gastrointestinal tract, and promote flatulence is limited. The content of potassium, magnesium, lipotropic substances, and foods that have an alkalizing effect (dairy, vegetables, fruits) has been increased. Meat and fish are boiled. Avoid hard-to-digest foods. Food is prepared without salt. The food temperature is normal.
Chemical composition and energy value: proteins 90 g (55-60% animal), fats 70 g (25-30% vegetable), carbohydrates 350-400 g; energy value 2500-2600 kcal; sodium chloride 6-7 g (3-5 g per hand), free liquid 1.2 l.
Diet: 5 times a day in relatively equal portions.
Excluded products and dishes: fresh bread, butter and puff pastry products, pancakes, pancakes; legume soups, meat, fish, mushroom broths; fatty meats, goose, duck, liver, kidneys, brains, smoked meats, sausages, canned meat; fatty, salted, smoked fish, caviar, canned fish; salty and fatty cheeses; hard-boiled eggs, fried; legumes; salted, pickled, pickled vegetables; spinach, sorrel, radish, radish, garlic, onions, mushrooms; spicy, fatty and salty snacks; fruits with coarse fiber, chocolate, cakes; sauces based on meat, fish, mushroom broth, mustard, pepper, horseradish; natural coffee, cocoa; meat and cooking fats.
Diet No. 10a
Indications: diseases of the cardiovascular system with severe symptoms of heart failure.
Purposes of administration: improvement of impaired blood circulation, functions of the cardiovascular system, liver, kidneys, normalization of metabolism by removing accumulated metabolic products from the body, ensuring sparing of the cardiovascular system, kidneys, and digestive organs.
General characteristics: reduction in energy value due to proteins, carbohydrates and especially fats. The amount of sodium chloride and liquid is sharply limited. Food is prepared without salt, bread is salt-free. Foods and substances that excite the central nervous and cardiovascular systems, irritate the liver and kidneys, and promote flatulence (extractive substances from meat and fish, fiber, fatty foods, cholesterol, tea and coffee, etc.) are sharply limited. Sufficient content of potassium, lipotropic substances, foods that alkalize the body (dairy products, fruits, vegetables). Dishes are prepared boiled and mashed, giving them a sour or sweet taste and flavoring. Fried foods are prohibited. Hot and cold dishes are excluded.
Chemical composition and energy value: proteins 60 g (70% animal), fats 50 g (20-25% vegetable), carbohydrates 300 g (70-80 g sugar and other sweets); energy value 1900 kcal; sodium chloride is excluded, free liquid is 0.6-0.7 l.
Diet: 6 times a day in small portions; The diet is prescribed for a limited time - no more than 4 weeks.
Excluded products and dishes: fresh and other types of bread, baked goods; fatty, stringy meat, pork, lamb, duck, goose, sausages, smoked meats, canned food; fatty, salted, smoked fish, caviar; cheese; hard-boiled eggs, fried; millet, barley, pearl barley, legumes, pasta; fruits with coarse fiber, hard skin, grapes; chocolate, cream products; sauces based on meat, fish, mushroom broths, fatty sauces, horseradish, pepper, mustard; natural coffee, cocoa, grape juice, carbonated drinks, kvass; fats (except for fresh butter and, if tolerated, refined vegetable oils 5-10 g per dish).
Diet No. 10c
Indications: atherosclerosis with damage to the vessels of the heart, brain or other organs; myocardial infarction in the scarring stage, hypertension.
Purpose of administration: slowing the development of atherosclerosis, reducing the severity of metabolic disorders, improving blood circulation, reducing excess body weight, providing nutrition without overloading the cardiovascular system and central nervous system, liver, kidneys.
General characteristics: the diet reduces the content of animal fat and easily digestible carbohydrates. The protein content corresponds to the physiological norm. The degree to which the intake of fats and carbohydrates is reduced depends on body weight (see two diet options below). Table salt, free liquid, extractives, cholesterol are limited. The content of vitamins C and group B, linoleic acid, lipotropic substances, dietary fiber, potassium, magnesium, microelements (vegetable oils, vegetables and fruits, seafood, cottage cheese) is increased. Dishes are prepared without salt; food is added at the table. Meat and fish are boiled, vegetables and fruits with coarse fiber are chopped and boiled. The food temperature is normal.
Chemical composition and energy value:
- Option I: proteins 90-100 g (50% animal), fats 80 g (40% vegetable), carbohydrates 350-400 g (50 g sugar); energy value 2600-2700 kcal;
- Option II (with concomitant obesity): proteins 90 g, fats 70 g, carbohydrates 300 g; energy value 2200 kcal; sodium chloride 8-10 g, free liquid 1.2 l.
Diet: 5 times a day in small portions; kefir at night.
Excluded products and dishes: products made from butter and puff pastry; meat, fish, mushroom broths, legume broths; fatty meats, duck, goose, liver, kidneys, brains, sausages, smoked meats, canned food; fatty fish, salted and smoked fish, caviar; salty and fatty cheese, heavy cream, sour cream and cottage cheese; radish, radish, sorrel, spinach, mushrooms; fatty, spicy and salty seafood; limited or excluded (for obesity): grapes, raisins, sugar, honey (instead of sugar), jam, chocolate, cream products, ice cream; meat, fish, mushroom sauces, pepper, mustard; strong tea and coffee, cocoa; meat and cooking fats.