Published: 05/27/2021 11:45:00 Updated: 05/28/2021
Coronary heart disease is a chronic or acutely developing disease characterized by partial or complete cessation of blood supply to the heart muscle.
The cause of this phenomenon is spasm and thrombosis of the coronary arteries, usually due to their atherosclerotic changes.
Organ ischemia is most often manifested by paroxysmal chest pain - angina pectoris; with a sharp and pronounced disturbance of blood flow in the vessels, myocardial infarction develops.
Prevalence of the disease
In Russia, about 5.1-5.3% of the population suffers from ischemic heart disease.
At the same time, coronary heart disease remains the main cause of mortality and disability in the population. Worldwide, deaths from pathologies of the cardiovascular system account for a third of diagnosed cases. In Russia, this figure is higher and amounts to 57%, of which 29% are deaths due to myocardial ischemia. Myocardial ischemia mainly affects people over 40 years of age. In young and middle age, coronary heart disease is more often detected in men; with increasing age, the ratio of cases evens out.
Risk factors for the development of myocardial ischemia
Factors predisposing to this disease are conventionally divided into two groups – modifiable and non-modifiable.
By eliminating or correcting the former, the risk of coronary heart disease is significantly reduced. This group includes situations in which the myocardium needs more oxygen than usual (or oxygen delivery is reduced without increasing its consumption):
- sedentary lifestyle;
- excess weight;
- unhealthy diet – a large amount of fatty and high-calorie foods in the diet;
- psycho-emotional stress;
- bad habits, especially smoking;
- high levels of “bad” cholesterol and triglycerides in the blood;
- high blood pressure – arterial hypertension;
- diabetes;
- endocarditis and heart defects;
- decrease in the concentration of high-density lipoproteins in the blood.
Factors that cannot be changed:
- male gender;
- age over 65 years;
- IHD, especially myocardial infarction in the past in close relatives of the patient;
- the onset of menopause.
The likelihood of coronary heart disease in women increases significantly with the onset of menopause.
Causes
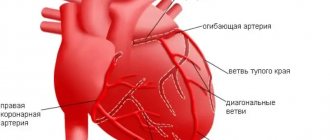
IHD occurs as a result of atherosclerosis of large (epicardial) coronary (heart) arteries of varying degrees: from a slight narrowing of the lumen in the vessel to its complete blockage by atheroma (cholesterol, fat) masses or a blood clot that has developed at the site of a “vulnerable” (damaged) atherosclerotic plaque (ASP) . Other causes of IHD are spasm of the coronary arteries and damage to the microvasculature in the myocardium. In most cases, they also develop against the background of existing atherosclerosis.
It is possible to identify the population groups most susceptible to the development of coronary artery disease: people suffering from high blood pressure, those addicted to smoking, those suffering from high cholesterol levels, diabetes mellitus, and chronic kidney diseases. . Male gender and old age are also powerful risk factors for the development of coronary artery disease.
Symptoms and forms of IHD
With different forms of coronary heart disease, symptoms may differ. There are several forms of the disease.
Angina pectoris
The condition is characterized by attacks of squeezing or burning pain behind the sternum, which usually appears during physical and emotional stress.
It can radiate to the left arm, neck, shoulder, lower jaw, subscapular region, upper abdomen. For this reason, angina pectoris is also called “angina pectoris.” The duration of pain is usually several minutes. Depending on the stability of the course of the disease, stable and unstable forms of angina are distinguished. The first occurs only after physical or psycho-emotional stress, with increased blood pressure, tachycardia. As the disease progresses, the amount of activity available to a person decreases, and in the fourth class of pathology, he can no longer make any movement without developing attacks of chest pain.
Unstable angina can be new - a month or less after the onset of symptoms, progressive and early post-infarction. Progressive angina is characterized by a decrease in the load tolerated, for example, a decrease in the distance that a person can walk without the appearance of symptoms.
Unstable angina requires examination and treatment in a hospital; the risk of myocardial infarction is high.
Myocardial infarction
Develops acutely.
Due to a prolonged decrease in blood flow or its complete cessation to certain areas of the heart muscle, necrosis of the area of the heart muscle occurs - necrosis. The affected area can be of different sizes depending on the diameter of the affected vessel, which is why the disease is often called large-focal or small-focal myocardial infarction. The pain in this condition is intense, pressing and squeezing in nature, and attacks of burning “dagger” pain are also common. In many patients, it has a typical localization in the retrosternal region, but it can also involve the area to the left of the sternum or spread to the entire surface of the chest. In this case, the patient experiences “fear of death”, melancholy, a feeling of doom arises, and may be restless and very excited.
The localization of pain during myocardial infarction can be almost any; for example, sometimes pain occurs even in the abdomen. There is also a painless form.
With small focal lesions, the symptoms may be blurred, and diagnosis by ECG can be difficult.
Spontaneous Prinzmetal ischemia
Substernal pain occurs against the background of spasm of the coronary vessels and is not associated with exercise. Most often, the condition develops at night, between midnight and eight o'clock in the morning. Spastic angina is characterized by regularity and cyclicity, often repeating several attacks in a row with a short interval.
Post-infarction cardiosclerosis
After a heart attack, dead muscle cells are replaced with connective tissue. In this case, conductivity in the myocardium is disrupted, which may be accompanied by sensations of interruptions in the work or prolonged cardiac arrest, periodic fainting and dizziness. There may also be attacks of rapid heartbeat, chest pain, shortness of breath, pale or blue discoloration of the skin.
Heart failure
A disease in which the heart cannot fully perform its function of providing the tissues of various organs with a sufficient amount of blood. The condition is manifested by shortness of breath, swelling, fatigue, and poor tolerance to physical activity.
Heart rhythm disturbances
Arrhythmias are of various types. Accompanied by a feeling of palpitations or a decrease in heart rate. The patient may experience severe weakness, dizziness, nausea, and possible loss of consciousness. There are also asymptomatic forms of pathology, which become an accidental finding on the ECG.
Silent myocardial ischemia
It occurs without characteristic attacks of angina pectoris. It is usually detected accidentally on an ECG and after special diagnostic exercise tests.
Sudden cardiac death
More often it occurs due to ventricular fibrillation or flutter - erratic contraction of the heart muscle at high frequency. The condition develops unexpectedly and is manifested by the following symptoms:
- weakness;
- dizziness;
- loss of consciousness;
- noisy and rapid breathing;
- dilated pupils;
- decrease in respiratory rate;
- absence of heart contractions.
Sometimes the heart can be returned to the correct rhythm, but if this was not done in the first minutes, then the brain cells die from hypoxia, and an irreversible coma develops.
According to modern data, silent myocardial ischemia (SPMI) is a common phenomenon that occurs in 2-57% of the total population, and among practically healthy individuals with risk factors for coronary artery disease, in 15-20% of cases. “Silent” ischemia, like angina, occurs due to a combination of various causes, among which the most common are stenosis, spasm of the coronary arteries and impaired platelet aggregation. 100% of patients with BBIM have severe multiple lesions of the coronary arteries. The article presents a literature review on modern data on the pathogenesis, diagnosis, treatment and prognosis of BBIM.
Painless myocardial ischemia (pathogenesis, diagnosis, treatment, prognosis)
According to recent data, painless myocardial ischemia (PMI) is a common phenomenon, which occurs in 2-57% of the population and among healthy individuals with risk factors for IHD 15-20% of cases. "Silent" ischemia, as well as angina, is caused by a combination of a variety of reasons, including stenosis, spasm of the coronary arteries and a violation of platelet aggregation. In 100% of patients with severe multiple PMI have coronary artery disease. The article presents a review of the literature on current data on pathogenesis, diagnosis, treatment and prognosis PMI
In 1957, R. Wood first reported that among the 100 patients he examined, in 26 patients changes in the electrocardiogram (ECG) were not accompanied by anginal pain. This phenomenon was later called painless, or “silent” myocardial ischemia [1].
Silent myocardial ischemia (SMI) (“silent”, “silent”, silent ischemia) are episodes of transient short-term ischemia of the heart muscle with the occurrence of changes in metabolism, contractile function or electrical activity of the myocardium, objectively detected using some instrumental research methods, but not accompanied attacks of angina or its equivalents (shortness of breath, arrhythmia and other unpleasant sensations) that occur during physical activity [2, 3].
Prevalence. According to modern data, BBIM is a common phenomenon that occurs in 2-57% of the total population, and among practically healthy individuals with risk factors for IHD, in 15-20% of cases [4, 5, 6]. Using various methods, BBIM is detected in 40-60% of patients with stable angina and in 60-80% with unstable angina [8]. Transient BBMI is observed in 65% of patients with congestive heart failure, most often of ischemic origin [9]. BBIM is detected in patients with various heart rhythm disorders (primarily ventricular) [10], especially often in patients with arterial hypertension [1]. The risk of developing “silent” ischemia is significantly higher in smokers (63%) (compared to non-smokers - 42%), i.e. smoking is an independent predictor of ischemia. BBIM is diagnosed in 20-35% of patients with various forms of diabetes mellitus (DM) [6].
The following risk groups for the occurrence of silent myocardial ischemia are distinguished. The first group is patients who have had an MI; persons with several risk factors for coronary artery disease (with severe hyperlipidemia, episodes of ACEI are 2 times more frequent over time; in the presence of 1 risk factor, ACEI was recorded in 17.7%, 2 risk factors - in 71%). The second group includes patients with a combination of coronary artery disease and arterial hypertension (AH). The third group is patients with diabetes. The fourth group includes patients with a combination of coronary artery disease and chronic obstructive pulmonary disease. The fifth group includes some professional groups of high-risk individuals - transport drivers, pilots, surgeons, etc. [11].
Pathogenesis. The pathogenetic mechanisms of painless and painful ischemia are the same and are caused by a discrepancy between the myocardial oxygen demand and coronary blood flow. “Silent” ischemia, like angina, occurs due to a combination of various causes, among which the most common are stenosis, spasm of the coronary arteries and impaired platelet aggregation. It can be provoked by a number of factors that are also characteristic of other forms of IHD: physical activity, emotional stress, smoking, cold. Episodes of AFMI occur more frequently in the morning and evening, consistent with the circadian rhythm of angina. An increase in the number of episodes of BBMI in the morning is associated with physiological changes: an increase in heart rate and blood pressure, platelet activation, an increase in the level of catecholamines in the blood, and a decrease in fibrinolytic activity [6].
100% of patients with BBIM have severe multiple lesions of the coronary arteries (CA). It is characterized primarily by damage to the main trunk of the left coronary artery or damage to the right coronary artery, good development of collaterals in the region of blood supply to the affected arteries and a large extent of coronary stenosis.
Despite numerous works devoted to the study of the phenomenon of BBIM, a satisfactory answer to the question of why myocardial ischemia in some cases manifests itself as attacks of anginal pain, and in others remains “silent” has not yet been obtained [1]. It has been suggested that BBIM may be associated with impaired sensitivity of intramyocardial nerve endings due to neuropathy that develops for various reasons, for example, due to diabetes mellitus [12], the toxic effect of certain cytostatics [13], myocardial infarction (MI), when the sympathetic nerves are affected fibers, which are the main route of transmission of pain impulses [6]. According to one hypothesis, “silent” myocardial ischemia occurs when the strength and duration of exposure to the stimulus is insufficient. Ischemia causes pain when a certain threshold value is reached (pain occurs in cases where myocardial ischemia lasts at least 3 minutes). This is confirmed by data on a significantly lower depth and duration of ST segment displacement during BBIM; at the same time, it is known that pain attacks occur with minimal severity of myocardial ischemia and, on the contrary, a complete absence of clinical symptoms with significant ischemic changes. A decrease in the number and sensitivity of intramyocardial receptors to adenosine, which is the main stimulator of pain receptors and is released during myocardial ischemia, plays a role in the disruption of the formation of nociceptive flow [6, 14, 15].
In patients with BBIM, the activity of the antinociceptive system significantly increases, which consists of reducing pain by increasing the influence of the central nervous system (reticular formation, thalamus and gray matter around the aqueduct of Sylvius). As a result, the pain sensitivity threshold increases significantly, which is the most important pathogenetic feature of BBIM [17]. This mechanism is more often present in asymptomatic patients with signs of ischemia of the posterior wall of the left ventricle with damage to the right coronary artery, where most of the ascending vagal fibers are located [6, 16]. The results of a number of studies have refuted the assumption that with BBIM a smaller volume of myocardium is damaged compared to painful forms [3].
The patient’s personal characteristics play a certain role in the occurrence of BBIM. There are psychological phenomena (style of pain perception, the phenomenon of denial) that influence the ability to perceive pain. The phenomenon of denial allows you to protect yourself from a threatening and alarming situation, to reduce not only fear, but also the feeling of pain. The style of pain perception should also be taken into account in the pathogenesis - patients with BBIM have, in addition to reduced sensitivity to pain, a general decrease in tactile sensitivity. A decrease in the perception of pain may be hereditary or the result of special upbringing conditions [6].
In recent years, evidence has emerged that BBIM is caused by genetic factors. In particular, there is evidence [17] that the presence of allele D of the gene encoding the synthesis of angiotensin-converting enzyme in the genotype of patients with type 2 diabetes mellitus significantly increases the frequency of detection of BBIM in this category of patients.
Classification and diagnosis . In the Russian recommendations for the diagnosis and treatment of stable angina (2008), 2 types of BBIM are identified: type I: completely BBIM; Type II: a combination of BBMI and painful episodes of myocardial ischemia. Type I BBIM is observed in approximately 18% of individuals with coronary atherosclerosis proven by coronary angiography. BBIM type II is noticeably more common than BBIM type I. Thus, in individuals with typical angina, about 50% of episodes of myocardial ischemia are asymptomatic.
The basis for diagnosing BBIM is a variety of instrumental research methods [3, 18], which can objectify the presence of ischemia of the heart muscle. They can be divided into 4 categories:
1. The most common and accessible methods for diagnosing BBIM are electrocardiographic. The most specific marker of myocardial ischemia in patients with coronary artery disease is a decrease in the ST segment upward › 1 mm in any of the leads, with the exception of V2, where a rise is considered 2 mm or more, or downward from the isoelectric line › 1 mm and lasting 80 ms from the J point, slow oblique decrease in ST at point J+80 ms › 1 mm (rapid oblique decrease in ST is not considered ischemic) [2, 3, 9]. Sometimes BBMI can be detected when recording a standard ECG at rest, but most often - during Holter monitoring (HMT) in a physical and emotional atmosphere familiar to the patient [19]. CMT provides information about the time of onset of BBMI episodes, their number and duration, allows for parallels with the patient’s activity patterns during the day, and analyzes the circadian variability of ischemic episodes, their correlation with heart rate and ectopic activity. The absence of contraindications for use, accessibility and high information content allow the CMT ECG method to be widely used for the purpose of diagnosing BBIM and assessing the effectiveness of therapeutic measures. The sensitivity of the XMT ECG method is 55-65%, specificity is 77-92%. The high information content of the CMT ECG method increases with increasing study time to 48-72 hours. In the course of the study, among people with stable angina, after 24 hours of ECG monitoring, BBMI was detected in 64%; after 48 hours, this figure was 83%; after 72 hours, “silent” myocardial ischemia was detected in 94% of those examined [6, 11].
If the resting ECG and CMT data are not informative, physical exercise tests (PE) are performed: bicycle ergometry (VEM), treadmill test [5]. It is believed that the appearance of “silent” ischemia during these tests in patients with coronary artery disease not only has high diagnostic significance, but also indicates an increased risk of developing adverse outcomes of the disease. However, the use of tests with dosed FN is often difficult due to the patient’s lack of training, the presence of orthopedic and neurological disorders, and a pronounced increase in blood pressure (BP). In this regard, a cardioselective test with transesophageal electrical stimulation of the atria (TEES), which excludes a number of peripheral factors, has certain advantages in this regard, in which imposing an artificial rapid rhythm on the heart causes an increase in the myocardial oxygen demand. Its sensitivity and specificity vary widely: 20-96% and 50-70%, respectively. Therefore, it is recommended, as a rule, to use TEES to exclude false-negative (or false-positive) results of stress tests. Less commonly, pharmacological provocative tests with dobutamine, dipyridamole, adenosine, a cold test, and psychoemotional stress are used as a provoking agent [2, 6, 16]. In the diagnostic assessment of the severity of BBIM, stress tests and CMT ECG complement each other. Treadmill test, VEM, TEES make it possible to detect BBIM and the ability to associate it with blood pressure, heart rate (HR), and physical function.
2. Assessment of myocardial perfusion - coronary angiography (CAG), scintigraphy, single-photon emission computed tomography, electron beam computed tomography.
The “golden” standard for diagnosing IHD is coronary angiography. There is a direct relationship between the presence of the BBIM phenomenon and the detection of coronary artery stenosis. On the other hand, there are known facts of the presence of BBIM and the absence of significant stenosis according to coronary angiography, which is quite often described in women [6]. The number of episodes of asymptomatic myocardial ischemia in patients with angina depends on both the number of affected coronary arteries and the severity of coronary artery lesions, and in those examined with BBMI, the number of recorded episodes of BBMI largely depends not on the number of affected coronary arteries, but on the severity of coronary artery lesions [ 20, 21].
To diagnose metabolic changes during myocardial ischemia, methods using radioactive markers have been developed. Depending on the characteristics of the isotope, two main methods of imaging the myocardium are used: single-photon emission computed tomography (free fatty acids labeled with radioactive iodine are used) and positron emission computed tomography. To carry it out, a large number of compounds have been synthesized: palmitate labeled with radioactive carbon (study of fatty acid metabolism), 18F-fluorodeoxyglucose (assessment of myocardial glucose consumption), ammonia labeled with radioactive nitrogen (assessment of regional blood flow) [6]. To determine the area and depth of the myocardial perfusion defect, single-photon emission computed tomography is used [22]. Using the positron emission tomography (PET) method, one can judge the metabolic activity of the myocardium - assess the degree of utilization of glucose and/or fatty acids. Episodes of BBMI are characterized by disruption of regional blood flow, as well as regional myocardial glucose consumption, which is quite accurately detected using the PET method [18]. The disadvantage of the method is its high cost, so it cannot be recommended for widespread use [6].
An important method for diagnosing BBIM is perfusion scintigraphy, which allows assessing not only blood flow in the myocardium, but also the degree of damage to cardiomyocytes [23]. The information content of the method increases when combined with physical exercise. When performing perfusion scintigraphy, tissues with normal coronary blood flow accumulate radiopharmaceuticals (thallium isotope-201, technetium compounds - isonitrile, tetrofosmin, etc.) quite evenly, while during myocardial ischemia, including painless, zones of reduced accumulation appear [20, 21]. The sensitivity of the method ranges from 80-90%, and the specificity reaches 100% [9].
The specificity of instrumental methods for diagnosing BBIM increases when they are combined with certain laboratory tests—the study of the level of troponins, myoglobin, and natriuretic peptides [24, 25].
3. Transient disturbances of myocardial function, characteristic of BBIM, are diagnosed using echocardiography, especially stress echocardiography, stress echocardiography using tissue Dopplerography [6, 16]. Dynamic exercise tests (treadmill test, bicycle ergometry), electrical stimulation of the heart, and pharmacological tests (dobutamine, dipyridamole, arbutamine, adenosine) are used as stress tests, which provoke the occurrence of ischemia by increasing the myocardial oxygen demand or due to a decrease in its delivery to the myocardium [26] . The detected transient myocardial dyssynergia, a decrease in the ejection fraction and the rate of circulatory shortening of myocardial fibers indicate its ischemia. The sensitivity of stress echocardiography in diagnosing BBIM reaches 70%, specificity - 80% [6, 27]. A promising direction in the development of stress echocardiography is the additional use of tissue Doppler ultrasound, which allows quantitative assessment of the test results [28].
Treatment of silent myocardial ischemia. If you have IHD, it is necessary to begin treatment by eliminating risk factors - quitting smoking, normalizing body weight, blood pressure, increasing physical activity, reducing the consumption of table salt and animal fats, identifying and correcting dyslipidemia and carbohydrate metabolism.
Currently, there is no doubt about the need for treatment of BBIM, as it prevents the progression of various forms of IHD and improves the quality of life of patients [3, 9]. In this regard, an urgent task in the treatment of patients with coronary artery disease is the need for timely detection and rational drug correction of BBIM, since these patients practically do not receive antianginal therapy. It should be emphasized that BBIM is a legitimate form of IHD and its treatment is carried out according to the same principles as the treatment of other clinical forms of IHD. When treating IHD, all episodes of myocardial ischemia should be affected - painful and non-painful, i.e. strive to reduce the so-called total ischemic burden - total ischemic burden. The distribution of BBIM episodes during the day showed the presence of two peaks - from 9 to 14 hours and from 17 to 20, which must be taken into account when selecting drug therapy [29].
If the patient has stable angina, treatment is carried out according to the recommendations of the All-Russian Scientific Committee “Diagnostics and Treatment of Stable Angina” (2008) and the EOC (2006) [30].
In the treatment of type I BBIM, the following groups of drugs are most often used [11]: β -blockers, nitrates , calcium antagonists, angiotensin-converting enzyme inhibitors, statins, myocardial cytoprotectors.
B -adrenergic blockers. If exercise tolerance is low and the total duration of BBIM is more than 10 minutes per day, treatment should include beta-blockers (BAB) (31). According to summary data from several controlled studies, blockers reduce the number of episodes of BBMI by an average of 70-75% (while ACs - by 40-45%), and the duration of ischemia is reduced by 69% [29]. In addition, a beneficial effect of beta blockers was noted on reducing the morning increase in episodes of acute myocardial infarction in patients with coronary artery disease, which reduces the risk of acute myocardial infarction and sudden death. BBs in doses selected using exercise tolerance test (ETT) have a significant effect after 2 hours. Therefore, with frequent episodes of myocardial ischemia (painful and non-painful) within 24 hours, you can use both short-acting beta blockers 3-4 times and long-acting beta blockers once a day.
Effective doses of beta blockers in relation to BBIM correspond to 80-320 mg for propranolol (average 160 mg), for metoprolol 50-200 mg (average 150 mg).
A significant advantage of beta blockers, in contrast to nitrates and AKs, is the lack of addiction to the anti-ischemic effect.
After sudden withdrawal of beta blockers, an increase in the frequency of episodes of myocardial ischemia is also possible, which is apparently due to the increased myocardial oxygen demand.
Calcium antagonists. Short-acting dihydropyridines are not recommended because they can lead to reflex tachycardia, increased catecholamine levels, episodes of peripheral vasodilation and proischemic effects.
Currently, special attention is being drawn to long-acting non-dihydropyridine (pulse-cutting) ACs, which are effective and safe for the treatment of BBMI; they help to stop the signs of myocardial ischemia with ST segment depression during the exercise test [11], significantly reduce the incidence and duration of ischemic episodes, but less effective than beta blockers (5, 30, 32).
Nitrates. The anti-ischemic (not inferior to AA) effect of prolonged forms of isosorbide-5-mononitrate (ISMN) has been proven, which is accompanied by a reduction in both painful and painless episodes of IHD [33].
Monotherapy with certain forms of nitrates (nitroglycerin patch, nitroglycerin ointment) should not be recommended for BBIM due to the possibility of rebound myocardial ischemia during the nitrate-free period. To prevent BBIM in such a situation, a combination of nitrates with beta blockers or AK is recommended.
Trimetazidine. The long-acting anti-ischemic effect of trimetazidine occurs at the cellular level (3-ketoacyl-CoA thiolase inhibitor) under conditions of hypoxic myocardial damage without a significant effect on hemodynamic parameters (heart rate, blood pressure, etc.), improving coronary blood flow and myocardial circulation. The drug increases the duration of the load and increases its threshold at which myocardial ischemia occurs, provides reliable protection in the early morning hours, which is the period of the most frequent complications of coronary artery disease [11]. The clinical effectiveness of long-acting trimetazidine has been proven in monotherapy and as part of combination treatment.
Combination therapy. The combination of trimetazidine MB with metoprolol increases the duration of the load before the onset of an attack of angina and ST segment depression. The total number of ischemic episodes is significantly reduced, while BBIM episodes are reduced more significantly. Combined treatment with drugs with two different mechanisms of action - hemodynamic and cytoprotective - reveals high antianginal and anti-ischemic effectiveness [14].
Combination therapy with AK and beta blockers has a more pronounced anti-ischemic effect compared to monotherapy with each drug [29].
Statins. The severity of BBIM noticeably decreases with normalization of the lipid profile of the blood plasma during statin therapy [5, 29].
Angiotensin-converting enzyme inhibitors. Relatively recently, the ability of angiotensin-converting enzyme inhibitors (ACEIs) to have an anti-ischemic effect not only in pain, but also in BBMI has been proven.
Drugs of other groups. The effectiveness of antianginal drugs increases markedly when used with small doses of aspirin [11].
Surgery. In the treatment of BBIM, invasive methods (stenting of the coronary arteries and coronary artery bypass grafting) are effective [34]. Surgical treatments for BMI appear to be more effective than conservative therapy in individuals with an increased risk of cardiac events in the presence of several risk factors for coronary artery disease and decreased LV function. The duration of ischemic changes according to the CMT ECG data is important, especially with BMI. If the total duration of ST segment depression reaches 60 minutes, then this can be regarded as one of the indications for surgical treatment.
The most important result of the Asymptomatic Cardiac Ischemia Pilot (ACIP) study, which compared various treatment strategies for patients with CAD and CAD, was considered to be a more favorable rate of survival without cardiac events in the revascularization group compared with the drug therapy groups after 1 year of follow-up. Moreover, 65% of patients in the revascularization group did not require drug therapy. In other studies, the frequency of new episodes of BMI after coronary bypass surgery is 33%; after percutaneous transluminal coronary angioplasty, ischemia was detected in 22% of patients and in half of the cases there was BMI [11].
Forecast. According to available data [19, 35], BBIM is an unfavorable prognostic factor. Almost a third of patients with coronary artery disease with episodes of myocardial infarction subsequently develop angina, myocardial infarction, or sudden death. The presence of BBMI increases the risk of sudden death by 5-6 times, arrhythmias by 2 times, and the development of congestive heart failure by 1.5 times [2, 9]. In patients with damage to the 3 main coronary arteries and with type I BMI detected during an FN test, the risk of sudden death is increased 3 times compared to the risk of death in patients with angina attacks with the same lesion of the coronary artery.
Thus, BBIM is a fairly common condition, the pathophysiological mechanisms of which still remain unclear. The presence of BBMI is considered an unfavorable prognostic factor, so early diagnosis and its elimination are important components of the prevention of irreversible damage to the heart muscle.
A.I. Abdrakhmanova, S.D. Mayanskaya, I.L. Serdyuk, E.V. Malysheva
Kazan State Medical Academy
Republican Clinical Hospital No. 3, Kazan
Abdrakhmanova Alsu Ildusovna – Candidate of Medical Sciences, Assistant of the Department of Cardiology and Angiology
Literature:
1. Ilic S., Ilic MD, Petrovic D. et al. Silent myocardial ischemia in asymptomatic patients with multiple coronary risk factors // Medicine and Biology. - 2004. - V. 11. - No. 3. - P. 107-112.
2. Pateyuk I.V. Features of silent myocardial ischemia and rhythm disturbances in various types of left ventricular remodeling // Medical Journal. - 2007. - No. 4. - P. 48.
3. Mitkovskaya N.P., Pateyuk I.V., Shkrebneva E.I. Silent myocardial ischemia in women // Medical journal. - 2007. - No. 4. - P. 45.
4. Sajadieh A., Nielsen O.W., Rasmussen V. et al. Prevalence and prognostic significance of daily-life silent myocardial ischaemia in middle-aged and elderly subjects with no apparent heart disease // Eur. Heart J. - 2005. - V. 26. - No. 14. - P. 1402-1409.
5. Witek P. Silent myocardial ischemia // Przegl. Lek. - 2001. - V. 58. - No. 3. - P. 127-130.
6. Mitkovskaya N.P., Pateyuk I.V. Silent myocardial ischemia: pathophysiological features, prognostic significance // Medical Journal. - 2007. - No. 4. - P. 12-15.
8. Meiltz A., Ciaroni S. Silent myocardial ischaemia: a deafeningsilence // Rev. Med. Suisse. - 2005. - V. 1. - No. 9. - P. 613-616.
9. Arques S., Ambrosi P., Gelisse R. et al. Prevalence of angiographic coronary artery disease in patients hospitalized for acute diastolic heart failure without clinical and electrocardiographic evidence of myocardial ischemia on admission // Amer. J. Cardiology. - 2004. - Vol. 94. - No. 1. - P. 133-135.
10. Narula AS, Jha V., Bali HK et al. Cardiac arrhythmias and silent myocardial ischemia during hemodialysis // Ren Fail. - 2000. - V. 22. - No. 3. - P. 355-368.
11. Gurevich M. A. Silent myocardial ischemia: issues of pathogenesis and treatment // Consilium medicum. - 2007. - No. 11. - P. 13-17.
12. Manzella D., Paolisso G. Cardiac autonomic activity and Type II diabetes mellitus // Clin Sci (Lond). - 2005. - V. 108. - No. 2. - P. 93-99.
13. Bertolini A., Flumano M., Fusco O. et al. Acute cardiotoxicity during capecitabine treatment: a case report // Tumori. - 2001. - Vol. 87. - P. 200-206.
14. Nagaeva Yu.M., Sayfutdinov R.G. Silent myocardial ischemia // Practical medicine. — 2008.— No. 4.
16. Denisyuk V.I., Serkova V.K., Malaya L.T. Angina pectoris: Achievements, problems, prospects. - Vinnitsa - Kharkov: State Cartographic Factory, 2002. - 512 p.
17. Xing G., Zeng X., Wang Y., Zhao L. Angiotensin-converting enzyme gene and exercise-induced silent myocardial ischemia in type 2 diabetes mellitus // Zhonghua Yi Xue Yi Chuan Xue Za Zhi. - 2005. - V. 22. - No. 2. - P. 206-208.
18. Mitkovskaya N.P., Terekhov V.I., Avdey L.L., Pateyuk I.V. Silent myocardial ischemia - the path to diagnosis // Medical Journal. - 2008. - No. 3 (25). — P. 12-15.
19. Sejil S, Janand-Delenne B, Avierinos JF et al. Six-year follow-up of a cohort of 203 patients with diabetes after screening for silent myocardial ischaemia // Diabet Med. - 2006. - V. 23. - No. 11. - P. 1186-1191.
20. Anand D.V., Lim E., Hopkins D. et al. Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy // Eur. Heart J. - 2006. - Vol. 27. - P. 713-721.
21. Anand D.V., Lim E., Raval U. et al. Prevalence of silent myocardial ischemia in asymptomatic individuals with subclinical atherosclerosis detected by electron beam tomography // J. Nucl. Cardiology. - 2004. - Vol. 11. - No. 4. - P. 379-381.
22. Sergienko I.V., Vitko N.K., Radkevich L.A. and others. Positron emission tomography in assessing myocardial metabolism in patients with dilated cardiomyopathy and left bundle branch block // Cardiology. - 2005. - No. 8. - P. 28-32.
23. Scholte AJ, Bax JJ, Wackers FJ Screening of asymptomatic patients with type 2 diabetes mellitus for silent coronary artery disease: combined use of stress myocardial perfusion imaging and coronary calcium scoring // J. Nucl. Cardiol. - 2006. - V. 13. - No. 1. - P. 11-18.
24. Landesberg G., Vesselov Y., Einav S. et al. Myocardial ischemia, cardiac troponin, and long-term survival of high-cardiac risk critically ill intensive care unit patients // Crit Care Med. - 2005. - V. 33. - No. 6. - P. 1281-1287.
25. Wong KY, McSwiggan S, Kennedy NS et al. BNP identifies silent myocardial ischaemia in stroke survivors // Heart. - 2006. - V. 92. - P. 487-489.
26. Hadj-Abdelkader M., Rozand JY, Alphonse JC et al. Use of stress echocardiography in detecting silent myocardial ischemia in hemodialysis patients // Arch Mal Coeur Vaiss. - 2003. - V. 96. - No. 7-8. — P. 735-737.
27. Biagini E, Schinkel AF, Bax JJ et al. Longterm outcome in patients with silent versus symptomatic ischaemia during dobutamine stress echocardiography // Heart. - 2005. - Vol. 91. - No. 6. - P. 737-742.
28. Vasyuk Yu.A., Kopeleva M.V., Khadzegova A.B. and others. Diagnostic capabilities of stress echocardiography using tissue Dopplerography // Heart failure. - 2004. - No. 6. - P. 303-307.
29. Orlov V., Gilyarevsky S. Asymptomatic myocardial ischemia. Doctor's notes // Medical newspaper. - 2004. - No. 102-103.
30. Cardiology. Clinical recommendations // Edited by Yu.N. Belenkova, R.G. Oganova. - M.: Geotar-Media, 2009. - 901 p.
31. Takase B., Hikita H., Satomura K. et al. Effect of nipradilol on silent myocardial ischemia and heart rate variability in chronic stable angina // Cardiovasc Drugs Ther. - 2002. - V. 16. - No. 1. - P. 43-51.
32. Vatutin N.T., Kalinkina N.V., Keting E.V. and others. The role of endothelial dysfunction in the genesis of silent myocardial ischemia caused by anthracyclines // Archives of Clinical and Experimental Medicine. - 2001. - No. 3. - P. 287-290.
33. Ino-Oka E., Sagawa K., Takahashi T. et al. Efficacy of anti-anginal drugs in the treatment of angina pectoris associated with silent myocardial ischemia: importance of quantitative Holter ECG data for patient activity // Intern Med. - 2000. - V. 39. - No. 12. - P. 1027-1037.
34. Sousa JE, Sousa AG, Costa MA et al. Use of rapamycin-impregnated stents in coronary arteries // Transplant Proc. - 2003. - Vol. 35. - P. 165-170.
35. Zellweger MJ Prognostic significance of silent coronary artery disease in Type 2 Diabetes // Herz. - 2006. - V. 31 (3). — P. 240-246.
Diagnosis of coronary heart disease
Usually, complaints and symptoms characteristic of coronary heart disease help to suspect the disease.
To confirm myocardial ischemia, instrumental and laboratory diagnostic methods are used. Tests for coronary heart disease may include:
- Leukocytosis and decreased hemoglobin in a general blood test.
- Increased cholesterol and glucose, changes in the lipid profile according to biochemical blood tests.
- An increase in specific enzymes formed during the destruction of cardiomyocytes - creatine phosphokinase (its special fraction - MB) during the first 3-4 hours of a heart attack (lasts 48-72 hours), troponin-I, troponin-T (their level increases 6 hours after a heart attack and remains elevated for 7-14 days), aspartate aminotransferase (AST) (exceeds the normal level 8-12 hours after the onset of pain, normalizes within 3-4 days), lactate dehydrogenase (begins to exceed the normal level 14-48 hours after the onset of symptoms, returns to normal on days 7-14), myoglobin (increases 2 hours after the onset of symptoms and normalizes within 24 hours) in the blood.
- Elevated C-reactive protein and homocysteine levels are a risk for sudden cardiovascular events.
- Increased blood clotting according to the results of a coagulogram may also increase the risk of developing certain forms of coronary artery disease.
Instrumental research methods can be invasive or non-invasive. In the latter case, the following is used to diagnose coronary heart disease:
- electrocardiography;
- ultrasound examination of the heart - Echo-CG;
- Holter ECG monitoring;
- stress ECG tests: treadmill and bicycle ergometry;
- PET/CT of the heart.
Functional load tests are widely used.
They are used, among other things, to detect the early stages of coronary artery disease or a painless form of the pathology, when the disorders cannot be determined at rest. Walking, climbing stairs, exercises on exercise machines (an exercise bike, a treadmill), accompanied by ECG recording of current indicators, are used as stress tests for suspected coronary heart disease. The standard and most accurate method for this is diagnostics using a treadmill (treadmill) and an exercise bike (bicycle ergometry). Positron emission tomography (PET) is used to diagnose viable cardiac muscle cells. Radiopharmaceuticals are used, the accumulation of which in heart cells reveals viable and necrotic areas.
Among the invasive techniques, coronary angiography is used - x-ray examination of blood vessels using a contrast agent.
What classes is heart failure divided into?
There are several classifications of heart failure:
- Classification according to V. Kh. Vasilenko, N. D. Strazhesko, G. F. Lang;
- Classification of acute heart failure according to the Killip scale;
- And the most common is the New York Heart Association classification.
According to the New York Heart Association (NYHA) functional classification, heart failure is classified into classes I-IV depending on the severity of symptoms and limitation of physical activity.
Heart failure is divided into four classes depending on the severity of symptoms:
- NYHA I: heart disease without any restrictions on physical activity. Normal activity does not cause increased fatigue, palpitations, or difficulty breathing.
- NYHA II: Heart disease causing moderate limitation in daily activities. No symptoms at rest.
- NYHA III: Heart disease causing marked limitation in daily activities. Simple activities such as brushing your teeth, eating, or talking cause fatigue, palpitations, or difficulty breathing. There are no symptoms at rest.
- NYHA IV: Heart disease that causes symptoms at rest (and with any degree of light physical activity).
Heart failure significantly reduces quality of life. Patients often experience great frustration with physical limitations and tend to withdraw from social life. For this reason, psychological disorders such as depression are often present in addition to the expected physical symptoms.
Treatment of coronary artery disease
Treatment for coronary heart disease includes lifestyle changes, medications and, in some cases, surgery.
All patients are advised to give up bad habits, spend more time in the fresh air, and reduce excess body weight. In your diet, you must avoid foods high in fat, very salty and sweet foods. Smoking and unauthorized discontinuation of prescribed medications are strictly prohibited. All this can lead to a sharp deterioration in the patient's condition. To stop an attack of angina, you need to immediately stop physical activity, provide access to fresh air and take nitroglycerin under the tongue or use nitrate in the form of a spray.
Basic drug therapy includes the following drugs:
- antiplatelet agents – drugs that thin the blood;
- beta blockers;
- ACE inhibitors or sartans;
- statins.
Long-acting nitrates can be used to prevent attacks.
In the presence of concomitant diseases, especially diabetes mellitus and hypertension, their treatment and achievement of target blood pressure and glucose levels are required.
To restore cardiac blood flow, surgical intervention is necessary in some cases:
- Coronary artery bypass surgery is the creation of a bypass for blood at the site of narrowing of the coronary arteries using vascular prostheses.
- Coronary angioplasty and stenting - restoration of the diameter of the vessel, and, accordingly, the blood flow in it, by installing a special dilator.
Measures to prevent cardiovascular pathology
To avoid developing heart disease, you need to stop smoking and reduce your alcohol consumption.
Severe stress is also one of the predisposing factors to the occurrence of IHD. It is impossible to remove stress from life, but you can react to it correctly: humans are evolutionarily designed in such a way that muscle work is necessary after any stress. If you are worried or upset, then you need to squat, jog, or walk – the muscles should get tired. In case of severe anxiety, you may need to use sedatives, for the selection of which you need to consult a doctor.
Regular exercise with moderate physical activity is useful for the prevention of ischemia. You also need to monitor your weight and blood pressure. All persons over 40 years of age must be examined annually - take a biochemical blood test to check the level of cholesterol in the blood, and do an ECG.
Advantages of the clinic on Yauza
We do everything to make our visitors feel comfortable. At the medical center you will find polite and responsive staff, an individual approach, cozy and sterile hospital rooms. Doctors of the highest category carry out diagnostics and treatment using modern equipment.
There are systems of discounts and promotions. There is also a convenient pre-registration via the website. The doctors of our clinic, their education and work experience are also listed there. Thanks to this, you have the opportunity to make an appointment with a specific specialist. We guarantee effective treatment without pain or discomfort.
Make an appointment