Myocardial infarction is a focus of ischemic necrosis (death) of the heart muscle, resulting from an acute circulatory disorder in the coronary artery. Myocardial infarction is one of the most common forms of coronary heart disease (CHD). The condition poses a threat to human health and life and is the leading cause of death among adults in developed countries. Most often, symptoms of myocardial infarction are recorded in men (about 5 times more often than in women), and 70% of all sick people are aged 55–65 years. A heart attack manifests itself with extremely unpleasant symptoms: sharp pain in the chest, shortness of breath, cold sweat, and a feeling of fear. However, with timely identification of risk factors, diagnosis of a heart attack and provision of timely assistance during an attack of myocardial infarction in the clinic, it is possible to avoid tragic consequences.
Causes of heart attack
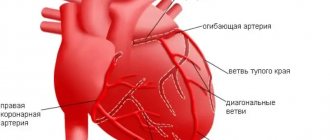
The direct cause of a heart attack is the sudden occurrence of an obstruction to blood flow in the branches of the coronary artery. In 95–97% of cases, such an obstacle is a blood clot formed as a result of atherosclerotic lesions of the arteries. In other cases, a heart attack occurs without any manifestations of atherosclerosis, and the main cause is a pronounced prolonged spasm of the coronary artery.
In extremely rare cases, myocardial infarction develops as a complication of other diseases (arteritis, developmental anomalies and injuries of the coronary artery, infective endocarditis, etc.). The likelihood of symptoms of an acute heart attack increases several times if the following risk factors are present:
- hyperlipoproteinemia (abnormal increase in the level of lipids and/or lipoproteins in the blood);
- old age (55 years and older);
- male gender;
- physical inactivity (lack of physical activity);
- obesity;
- smoking;
- diabetes;
- hypertonic disease;
- hereditary predisposition (presence of IHD in blood relatives).
Symptoms of a heart attack
In most cases, the first symptoms of myocardial infarction are increasing manifestations of a person’s existing angina:
- pain in the sternum (longer and more intense);
- an increase in the area of pain and the appearance of irradiation (spread of pain to other areas: left arm, shoulder blade, collarbone, jaw);
- a sharp drop in exercise tolerance;
- a significant decrease in the effect of taking nitroglycerin;
- development of shortness of breath at rest, dizziness, general weakness.
Symptoms of a heart attack rarely appear against the background of new-onset angina or after a period of long remission. Often, the occurrence of an acute heart attack is provoked by one of the following factors:
- severe stress;
- significant physical stress;
- severe overheating or hypothermia;
- surgery;
- sexual intercourse;
- binge eating.
The typical course of the disease is characterized by the fact that the main complaints are associated with such symptoms of a heart attack as severe pain, which is localized behind the sternum. The pain can be burning, squeezing, cutting. Often symptoms of myocardial infarction include pain spreading to the left arm, shoulder blade and shoulder. However, antianginal drugs such as nitroglycerin do not have an analgesic effect. Compared to an attack of angina, the duration of pain is increased: from 30 minutes to several days. Even slight physical activity or stress increases pain.
Most people note that the painful symptoms of a heart attack have a pronounced emotional overtones: there is a feeling of fear of death, hopelessness, doom, and intense melancholy. The person becomes easily excitable, may scream, and strive to constantly change body positions. In addition, symptoms of myocardial infarction are severe weakness, shortness of breath, excessive sweating, nausea, vomiting, and dry cough.
The examination reveals in patients such objective symptoms of a heart attack as pale skin with blue discoloration of the nasolabial triangle and nails, the skin is moist to the touch. The pulse rate rises to 90–100 beats per minute, while blood pressure rises slightly. Often in the first days, an increase in body temperature to 37–38 °C is detected.
Can the pressure go down?
Can you have a heart attack with low blood pressure? Yes, because during an attack a painful shock develops, which is accompanied by collapse (this condition is characterized by pathological narrowing of blood vessels, including the brain, and a lack of oxygen supply). In such a situation, a person loses consciousness, and blood pressure drops sharply.
Low pressure readings with a rapid pulse indicate an increase in the Algover shock index - this aggravates the picture of the attack and often leads to death due to the centralization of the blood supply. Initially, the heartbeat simply increases, but then tachycardia with a decrease in cardiac output is replaced by uncontrolled contraction of the atria. Ventricular fibrillation develops, which is considered a life-threatening condition.
Consequences of a heart attack
Myocardial infarction rarely goes away without leaving a trace. Its consequences in the form of complications can significantly reduce life expectancy. The most common complications of a heart attack are:
- early post-infarction angina;
- heart rhythm disturbances;
- cardiogenic shock (sharp decrease in myocardial contractility);
- acute cardiovascular failure;
- cardiac aneurysm (protrusion of the thinned wall of the heart);
- heart rupture (violation of its integrity).
After a heart attack, it is possible to return to a full life; the likelihood of this depends on many factors, including the timeliness and adequacy of treatment of the heart attack, the prevalence of tissue necrosis, and the presence of complications. Unfortunately, the mortality rate from a heart attack is high and amounts to about 35%. A third of those who have had the disease develop circulatory failure, in which people may lose their ability to work and become disabled.
Stages and complications of hypertension
Arterial hypertension leads to increased stress on the heart, blood vessels, and kidneys. Hypertension can cause diseases and pathologies such as:
- heart failure, myocardial infarction;
- cerebrovascular accidents (ischemic or hemorrhagic strokes);
- nephrosclerosis, renal failure;
- deterioration of vision (as a result of circulatory disorders in the retina).
Therefore, those who are at risk of developing the disease, as well as those who have already been diagnosed with hypertension, need to monitor their condition and regularly measure their blood pressure.
The following procedure for measuring pressure is recommended. Blood pressure is measured while sitting, after a five-minute rest. The measurement is carried out three times in a row, the lowest values are taken into account.
Depending on the detected pressure, three stages of hypertension are distinguished.
Stage I hypertension
characterized by increases in blood pressure in the range of 160-180/95-105 mmHg. Art.
Stage II hypertension
diagnosed with pressure in the range of 180-200/105-115 mm Hg. Art.
Stage III hypertension
– this is a severe pathological condition in which blood pressure is recorded in the range of 200-230/115-130 mm Hg. Art. This pressure cannot be normalized on its own, without medical help.
Diagnosis of myocardial infarction
In a typical course, the diagnosis of acute myocardial infarction is performed based on an analysis of the clinical picture of the disease. To confirm the diagnosis, electrocardiography and laboratory diagnostics are used. The presence of an atypical form can usually be determined only with the help of additional methods for diagnosing a heart attack. The main diagnostic signs of myocardial infarction are the following:
- prolonged pain (more than 30 minutes), which is not eliminated with nitroglycerin;
- characteristic pattern on the electrocardiogram;
- an increase in erythrocyte sedimentation rate (ESR), leukocytosis, detected by a general blood test;
- deviation of biochemical parameters from the norm (detection of C-reactive protein, increase in the level of fibrinogen, sialic acids);
- the presence in the blood of markers of myocardial cell death.
It is not difficult to distinguish between the symptoms of myocardial infarction and signs of other diseases with severe pain in the heart area (angina pectoris, pleurisy, pulmonary embolism, spontaneous pneumothorax, intercostal neuralgia, etc.) when diagnosing a heart attack. With an atypical course, it is more difficult: the abdominal form can be mistaken for food poisoning, peptic ulcer, pancreatitis, acute cholecystitis; cerebral form - for a stroke.
Treatment of heart attack
If qualified treatment of myocardial infarction is started in a timely manner, this largely determines the prognosis of the disease and the severity of the consequences. In the most acute and acute periods of the disease, hospital therapy is necessary. Treatment for a heart attack includes:
- relief of pain with analgesics, anesthesia with nitrous oxide for persistent pain;
- oxygen therapy – oxygen inhalations are performed using nasal catheters, flow rate 3–4 l/min;
- restoration of coronary blood flow using thrombolytic therapy;
- improving blood supply to the damaged area of the myocardium with the help of nitrates, β-blockers and calcium antagonists;
- prevention of heart rhythm disturbances using magnesium solution;
- stabilization of the emotional state with the help of sedatives, tranquilizers and psychotherapy;
- compliance with the daily regimen: first bed rest, after 2 weeks - ward rest, minimum physical activity (only dosed walking). The average duration of inpatient treatment for heart attack is 3 weeks.
- Compliance with the diet: diet during the acute period with the exclusion of “heavy” foods from the diet, increasing the frequency of meals and reducing the amount of food consumed at a time.
Classification
There are several classifications of heart attacks:
- by localization of tissue death. Possible infarction of the left or right ventricle, interventricular septum, apex of the heart, or combined localization;
- by the width of the lesion: extensive (large focal) or small focal. This parameter is assessed by ECG;
- by depth: if all layers of the heart are covered, the infarction is transmural. Subendocardial (affects the inner layer of the lining of the heart walls), subepicardial (affects the outer layer of the lining of the heart walls), intramural infarction (small-focal lesions) can also develop;
- according to the course: monocyclic (the attack develops quickly), protracted, recurrent (a new focus of necrosis develops 3-7 days after the first attack), repeated (a heart attack occurs again within up to 1 month).
When diagnosing, the location of necrosis is assessed (localization, depth and width of the focus of tissue necrosis), as well as the etiology and accompanying circumstances. A heart attack can be spontaneous or caused by ischemia, associated with oxygen deprivation, coronary intervention, or other reasons.
Stages
Symptoms associated with a heart attack may appear in the weeks, days, or hours before a heart attack. Usually this is pain, a burning sensation or squeezing during physical activity, weakness, and mild malaise. Such symptoms appear in the prodromal period preceding the attack. If you consult a doctor at this stage, you can prevent the development of a heart attack (Fig. 2).
Figure 2. Stages of infarction development. Source: Blausen Medical Communications, Inc. / and Journal of the American College of Cardiology
There are four main stages of a heart attack:
- acute. It continues from the development of ischemia until the necrosis of the heart tissue area. The average duration is from 20 minutes to 2 hours. Normal blood flow must be restored as quickly as possible. To do this, you need to remove the blood clot using thrombolytic therapy. If you suspect a heart attack, you should immediately call an ambulance so that doctors can begin such treatment;
- spicy. It begins when tissue necrosis has already occurred. At this stage, enzymatic melting of necrotic tissue occurs, which can last from 2 to 14 days;
- subacute A scar begins to form at the site of necrosis. It takes 4 to 8 weeks to form;
- post-infarction. At this stage, the scar matures and adaptation of the heart occurs.
Prevention of heart attack
The goal of primary prevention of myocardial infarction is to combat coronary heart disease and eliminate risk factors. Quitting smoking, maintaining an active lifestyle, systematic moderate physical activity, maintaining normal body weight, and a balanced diet will help prevent the development of a heart attack.
Secondary prevention aims to combat the development of recurrent infarctions: preventive measures include the prescription of anticoagulants, β-blockers, and calcium antagonists. An important point is to ensure patency of the coronary artery. This can be accomplished by cardiac bypass surgery or stenting of cardiac vessels.
If you need an examination to identify risk factors or treat a heart attack, the ABC-Medicine clinic offers you its assistance. To ask any question you are interested in about diagnosing a heart attack or any other aspects of the problem, as well as to make an appointment with a specialist, call +7.