Hypertension is a pathology of the heart and blood vessels, manifested by increased blood pressure. In the pathogenetic mechanism of the formation of the disease, disturbances in the neurohumoral, central and renal mechanisms of blood pressure regulation play a huge role.
Arterial hypertension is one of the fundamental risk factors for the development of potentially fatal diseases - stroke and heart attack. That is why it is important to know why hypertension occurs, how it is diagnosed and what medications are used in treatment.
Causes of hypertension
True hypertension, or, as it is also called, essential hypertension, occurs as a result of overstrain of the nervous system. The result of this process is a disruption of the processes of regulation and maintenance of optimal blood pressure.
Scientists have identified many factors that contribute to the occurrence of hypertension:
- excessive emotional stress;
- irregular working hours;
- lack of sleep;
- obesity;
- physical inactivity;
- diabetes;
- alcohol and tobacco abuse.
The hereditary dependence of the formation of hypertension has been proven - more than 20 genes have been identified that are responsible for the development of the pathology.
Symptoms of hypertension
The severity of clinical symptoms depends on the level of pressure increase and the involvement of the so-called target organs in the process. This term refers to those organs on which a prolonged increase in pressure affects the most unfavorably: the retina of the eyes, the brain, the kidneys, the heart.
At the initial stage, patients are usually bothered by dizziness and periodic headaches. An increase in pressure is usually accompanied by tinnitus, nausea, palpitations, and pulsation in the head.
The progression of the disease leads to symptoms of heart failure: shortness of breath during exercise, a feeling of lack of air. The chronic nature of the pathology is accompanied by swelling of the legs and puffiness of the face.
When blood pressure jumps, visual impairment may occur in the form of “floaters” in front of the eyes and decreased visual acuity. The most important symptom is an increase in pressure, confirmed instrumentally!
Degrees and stages of hypertension
Hypertension is classified according to stages and degrees. The division into degrees is based on the level of pressure rise:
- I degree - rise in systolic pressure above 139 up to 159 mm Hg. art (diastolic fluctuates in the range of 90-99 mm Hg);
- II degree - from 160 to 170 mm Hg. Art. (diastolic oscillation interval - 100-109);
- III degree - pressure rises above 180 mm Hg. Art.
The stage of hypertension also takes into account the degree of target organ damage:
- Stage 1 (low risk) - mild hypertension, in which there is no damage to target organs;
- Stage 2 (high risk) - moderate or severe course of the disease, in which target organs are involved in the process: cardiac hypertrophy, spasm of the retinal arteries, deterioration of renal blood flow;
- Stage 3 (very high risk) - an extremely severe course, accompanied by frequent hypertensive crises and dangerous damage to target organs in the form of stroke, heart attack, and retinal hemorrhages.
Hypertonic disease
Hypertension is a pathology of the cardiovascular system, developing as a result of dysfunction of higher centers of vascular regulation, neurohumoral and renal mechanisms and leading to arterial hypertension, functional and organic changes in the heart, central nervous system and kidneys. Subjective manifestations of high blood pressure include headaches, tinnitus, palpitations, shortness of breath, pain in the heart, blurred vision, etc. Examination for hypertension includes monitoring of blood pressure, ECG, echocardiography, ultrasound of the arteries of the kidneys and neck, urine analysis and biochemical parameters blood. Once the diagnosis is confirmed, drug therapy is selected taking into account all risk factors.
The leading manifestation of hypertension is persistently high blood pressure, i.e. blood pressure that does not return to normal levels after a situational rise as a result of psycho-emotional or physical stress, but decreases only after taking antihypertensive drugs. According to WHO recommendations, normal blood pressure is not exceeding 140/90 mmHg. Art. Exceeding the systolic reading over 140-160 mmHg. Art. and diastolic - over 90-95 mm Hg. Art., recorded at rest with double measurements during two medical examinations, is considered hypertension.
The prevalence of hypertension among women and men is approximately the same 10-20%; the disease most often develops after the age of 40, although hypertension is often found even in adolescents. Hypertension contributes to a more rapid development and severe course of atherosclerosis and the occurrence of life-threatening complications. Along with atherosclerosis, hypertension is one of the most common causes of premature mortality in the young working population.
There are primary (essential) arterial hypertension (or hypertension) and secondary (symptomatic) arterial hypertension. Symptomatic hypertension accounts for 5 to 10% of hypertension cases. Secondary hypertension is a manifestation of the underlying disease: kidney diseases (glomerulonephritis, pyelonephritis, tuberculosis, hydronephrosis, tumors, renal artery stenosis), thyroid gland (thyrotoxicosis), adrenal glands (pheochromocytoma, Itsenko-Cushing syndrome, primary hyperaldosteronism), coarctation or atherosclerosis of the aorta, etc. .
Primary arterial hypertension develops as an independent chronic disease and accounts for up to 90% of cases of arterial hypertension. In hypertension, high blood pressure is a consequence of an imbalance in the body's regulatory system.
Mechanism of development of hypertension
The pathogenesis of hypertension is based on an increase in cardiac output and peripheral vascular resistance. In response to the influence of a stress factor, disturbances in the regulation of peripheral vascular tone by higher centers of the brain (hypothalamus and medulla oblongata) occur. A spasm of arterioles occurs on the periphery, including renal arterioles, which causes the formation of dyskinetic and dyscirculatory syndromes. The secretion of neurohormones of the renin-angiotensin-aldosterone system increases. Aldosterone, which is involved in mineral metabolism, causes retention of water and sodium in the vascular bed, which further increases the volume of blood circulating in the vessels and increases blood pressure.
With arterial hypertension, blood viscosity increases, which causes a decrease in the speed of blood flow and metabolic processes in tissues. The inert walls of the vessels thicken, their lumen narrows, which fixes a high level of total peripheral vascular resistance and makes arterial hypertension irreversible. Subsequently, as a result of increased permeability and plasma saturation of the vascular walls, the development of elastofibrosis and arteriolosclerosis occurs, which ultimately leads to secondary changes in organ tissues: myocardial sclerosis, hypertensive encephalopathy, primary nephroangiosclerosis.
The degree of damage to various organs in hypertension may be different, so there are several clinical and anatomical variants of hypertension with predominant damage to the vessels of the kidneys, heart and brain.
Classification of hypertension
Hypertension is classified according to a number of criteria: the reasons for the rise in blood pressure, damage to target organs, the level of blood pressure, the course, etc. Based on the etiological principle, they distinguish between: essential (primary) and secondary (symptomatic) arterial hypertension. According to the nature of the course, hypertension can have a benign (slowly progressive) or malignant (rapidly progressive) course.
The level and stability of blood pressure is of greatest practical importance. Depending on the level there are:
- Optimal blood pressure is <120/80 mmHg. Art.
- Normal blood pressure is 120-129/84 mm Hg. Art.
- Borderline normal blood pressure - 130-139/85-89 mm Hg. Art.
- Arterial hypertension of the 1st degree - 140-159/90-99 mm Hg. Art.
- Arterial hypertension II degree - 160-179/100-109 mm Hg. Art.
- Stage III arterial hypertension - more than 180/110 mm Hg. Art.
According to the level of diastolic blood pressure, the following types of hypertension are distinguished:
- Mild course - diastolic blood pressure < 100 mm Hg. Art.
- Moderate course - diastolic blood pressure from 100 to 115 mm Hg. Art.
- Severe - diastolic blood pressure > 115 mm Hg. Art.
Benign, slowly progressive hypertension, depending on target organ damage and the development of associated (concomitant) conditions, goes through three stages:
Stage I (mild and moderate hypertension) - blood pressure is unstable, fluctuating during the day from 140/90 to 160-179/95-114 mm Hg. Art., hypertensive crises occur rarely and are not severe. There are no signs of organic damage to the central nervous system and internal organs.
Stage II (severe hypertension) - blood pressure in the range of 180-209/115-124 mm Hg. Art., hypertensive crises are typical. Objectively (with physical and laboratory examination, echocardiography, electrocardiography, radiography), narrowing of the retinal arteries, microalbuminuria, increased creatinine in the blood plasma, left ventricular hypertrophy, and transient cerebral ischemia are recorded.
Stage III (very severe hypertension) – blood pressure from 200-300/125-129 mm Hg. Art. and higher, severe hypertensive crises often develop. The damaging effect of hypertension causes the phenomena of hypertensive encephalopathy, left ventricular failure, the development of thrombosis of cerebral vessels, hemorrhages and edema of the optic nerve, dissecting vascular aneurysm, nephroangiosclerosis, renal failure, etc.
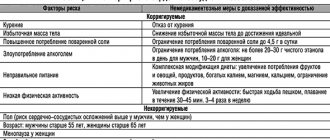
Risk factors for developing hypertension
The leading role in the development of hypertension is played by disruption of the regulatory activity of the higher parts of the central nervous system, which control the functioning of internal organs, including the cardiovascular system. Therefore, the development of hypertension can be caused by frequently repeated nervous overstrain, prolonged and severe anxiety, and frequent nervous shocks. The occurrence of hypertension is facilitated by excessive stress associated with intellectual activity, night work, and exposure to vibration and noise.
A risk factor in the development of hypertension is increased salt intake, which causes arterial spasm and fluid retention. It has been proven that consuming >5 g of salt per day significantly increases the risk of developing hypertension, especially if there is a hereditary predisposition.
Heredity, aggravated by hypertension, plays a significant role in its development in close relatives (parents, sisters, brothers). The likelihood of developing hypertension increases significantly if two or more close relatives have hypertension.
Arterial hypertension in combination with diseases of the adrenal glands, thyroid gland, kidneys, diabetes mellitus, atherosclerosis, obesity, chronic infections (tonsillitis) contribute to the development of hypertension and mutually support each other.
In women, the risk of developing hypertension increases during menopause due to hormonal imbalance and exacerbation of emotional and nervous reactions. 60% of women develop hypertension during menopause.
Age factors and gender determine an increased risk of developing hypertension in men. At the age of 20-30 years, hypertension develops in 9.4% of men, after 40 years - in 35%, and after 60-65 years - in 50%. In the age group under 40 years, hypertension is more common in men; in older age groups, the ratio changes in favor of women. This is due to a higher rate of male premature mortality in middle age from complications of hypertension, as well as menopausal changes in the female body. Currently, hypertension is increasingly being detected in people at a young and mature age.
Alcoholism and smoking, poor diet, excess weight, physical inactivity, and poor ecology are extremely conducive to the development of hypertension.
Symptoms of hypertension
The course of hypertension is varied and depends on the level of increase in blood pressure and the involvement of target organs. In the early stages, hypertension is characterized by neurotic disorders: dizziness, transient headaches (usually in the back of the head) and heaviness in the head, tinnitus, pulsation in the head, sleep disturbance, fatigue, lethargy, a feeling of weakness, palpitations, nausea.
Later, shortness of breath occurs when walking quickly, running, exercising, or climbing stairs. Blood pressure is persistently above 140-160/90-95 mm Hg. (or 19-21/12 hPa). Sweating, redness of the face, chill-like tremor, numbness of the toes and hands are noted, and dull, prolonged pain in the heart area is typical. With fluid retention, swelling of the hands (“ring symptom” - it is difficult to remove the ring from the finger), swelling of the face, puffiness of the eyelids, and stiffness are observed.
In patients with hypertension, there is a veil, flickering of flies and lightning before the eyes, which is associated with vasospasm in the retina; There is a progressive decrease in vision; retinal hemorrhages can cause complete loss of vision.
Complications of hypertension
With a long-term or malignant course of hypertension, chronic damage to the blood vessels of target organs develops: the brain, kidneys, heart, eyes. Instability of blood circulation in these organs against the background of persistently elevated blood pressure can cause the development of angina pectoris, myocardial infarction, hemorrhagic or ischemic stroke, cardiac asthma, pulmonary edema, dissecting aortic aneurysm, retinal detachment, uremia. The development of acute emergency conditions against the background of hypertension requires a decrease in blood pressure in the first minutes and hours, as it can lead to the death of the patient.
The course of hypertension is often complicated by hypertensive crises - periodic short-term increases in blood pressure. The development of crises may be preceded by emotional or physical overstrain, stress, changes in meteorological conditions, etc. In a hypertensive crisis, there is a sudden rise in blood pressure, which can last several hours or days and is accompanied by dizziness, severe headaches, a feeling of heat, palpitations, vomiting, cardialgia , visual impairment.
During a hypertensive crisis, patients are frightened, excited or inhibited, and drowsy; in severe cases they may lose consciousness. Against the background of a hypertensive crisis and existing organic changes in blood vessels, myocardial infarction, acute cerebrovascular accidents, and acute left ventricular failure can often occur.
Diagnosis of hypertension
Examination of patients with suspected hypertension has the following goals: to confirm a stable increase in blood pressure, exclude secondary arterial hypertension, identify the presence and degree of damage to target organs, assess the stage of arterial hypertension and the degree of risk of complications. When collecting anamnesis, special attention is paid to the patient’s exposure to risk factors for hypertension, complaints, level of increase in blood pressure, the presence of hypertensive crises and concomitant diseases.
Dynamic measurement of blood pressure is informative for determining the presence and degree of hypertension. To obtain reliable blood pressure levels, the following conditions must be met:
- Blood pressure measurement is carried out in a comfortable, quiet environment, after 5-10 minutes of patient adaptation. It is recommended to exclude smoking, exercise, eating, tea and coffee, and the use of nasal and eye drops (sympathomimetics) 1 hour before measurement.
- The patient's position is sitting, standing or lying down, with the arm at the same level as the heart. The cuff is placed on the shoulder, 2.5 cm above the fossa of the elbow.
- At the patient's first visit, blood pressure is measured in both arms, with repeated measurements after a 1-2 minute interval. If blood pressure asymmetry is > 5 mm Hg, subsequent measurements should be carried out on the arm with higher values. In other cases, blood pressure is usually measured on the “non-working” arm.
If blood pressure readings differ from each other during repeated measurements, then the arithmetic mean is taken as the true one (excluding the minimum and maximum blood pressure readings). In case of hypertension, self-monitoring of blood pressure at home is extremely important.
Laboratory tests include clinical blood and urine tests, biochemical determination of the level of potassium, glucose, creatinine, total blood cholesterol, triglycerides, urine analysis according to Zimnitsky and Nechiporenko, Rehberg test.
On electrocardiography in 12 leads in hypertension, left ventricular hypertrophy is determined. ECG data is clarified by echocardiography. Ophthalmoscopy with fundus examination reveals the degree of hypertensive angioretinopathy. An ultrasound scan of the heart determines enlargement of the left chambers of the heart. To determine target organ damage, ultrasound of the abdominal cavity, EEG, urography, aortography, CT scan of the kidneys and adrenal glands are performed.
Treatment of hypertension
When treating hypertension, it is important not only to lower blood pressure, but also to correct and reduce the risk of complications as much as possible. It is impossible to completely cure hypertension, but it is quite possible to stop its development and reduce the frequency of crises.
Hypertension requires the combined efforts of the patient and the doctor to achieve a common goal. At any stage of hypertension it is necessary:
- Follow a diet with increased consumption of potassium and magnesium, limiting the consumption of table salt;
- Stop or sharply limit alcohol intake and smoking;
- Get rid of excess weight;
- Increase physical activity: it is useful to engage in swimming, physical therapy, and walking;
- Take prescribed medications systematically and for a long time under the control of blood pressure and dynamic supervision of a cardiologist.
For hypertension, antihypertensive drugs are prescribed that depress vasomotor activity and inhibit the synthesis of norepinephrine, diuretics, β-blockers, antiplatelet agents, hypolipidemic and hypoglycemic drugs, and sedatives. The selection of drug therapy is carried out strictly individually, taking into account the entire range of risk factors, blood pressure levels, the presence of concomitant diseases and target organ damage.
The criteria for the effectiveness of treatment of hypertension is the achievement of:
- short-term goals: maximum reduction in blood pressure to a level of good tolerance;
- medium-term goals: preventing the development or progression of changes in target organs;
- long-term goals: prevention of cardiovascular and other complications and prolongation of the patient’s life.
Prognosis for hypertension
The long-term consequences of hypertension are determined by the stage and nature (benign or malignant) of the disease. Severe course, rapid progression of hypertension, stage III hypertension with severe vascular damage significantly increases the frequency of vascular complications and worsens the prognosis.
With hypertension, the risk of myocardial infarction, stroke, heart failure and premature death is extremely high. Hypertension has an unfavorable course in people who become ill at a young age. Early, systematic therapy and blood pressure control can slow the progression of hypertension.
Prevention of hypertension
For primary prevention of hypertension, it is necessary to exclude existing risk factors. Moderate physical activity, a low-salt and low-cholesterol diet, psychological relief, and giving up bad habits are useful. It is important to early identify hypertension through monitoring and self-monitoring of blood pressure, follow-up of patients, adherence to individual antihypertensive therapy and maintenance of optimal blood pressure levels.
Features of the course of hypertension with heart damage
A prolonged or particularly malignant course of the disease affects the heart muscle. Initially, myocardial hypertrophy develops - with the help of this, the heart tries to compensate for the excess load. Without treatment or if it is insufficiently effective, as well as with irregular medication use, the following types of heart damage may develop:
- angina pectoris - acute pain in the heart caused by a lack of oxygen;
- heart attack - an extreme degree of coronary artery disease, manifested by necrosis of the heart muscle;
- acute left ventricular failure - manifested by cardiac edema.
Hypertension with predominant heart damage without heart failure
Michael
1951 views
November 19, 2020
Hello! 36 years old, 83 kg, 192 cm, male Complaints: periodic pressure surges, underwent examination, verbally the doctor said that carvedilol should be increased from 12.5 to 25 once a day. When I read the diagnosis at home, I was stunned by “hypertension with primary damage to the heart without heart failure” and Possibly an enlargement of the left atrium Interatrial conduction disturbance The phenomenon of early ventricular repolarization How severe is the deviation from the norm? ——=======Stress echocardiography=======—— Initially: blood pressure 130/80 mmHg, heart rate 84 beats per minute During the test, a load of 12.7 METs was achieved. Duration of the test was: 12 min 29 sec At the height of the load, the heart rate was recorded: 166 beats per 1 min, 90% of the maximum heart rate, blood pressure 160x80 mm Hg. Reason for stopping the test: achievement of submaximal heart rate Load tolerance according to the test results: high Blood pressure response to load: adequate No significant ischemic changes in the ECG were noted Anginal attack: not recorded Echoradiography data Before load: LV walls with normal contractility After load: No disturbances in regional contractility revealed Conclusion: Test negative ——=======Electrocardiogram=======—— Heart rate: 60 beats per minute PQ: 141 ms QRS: 101 ms QT: 380 ms QTc: 388 ms Alpha angle: 37 Grad Regulation EOS: Intermediate ST: I 21 μV V1 -88 μV II 6 μV V2 121 MMV III -29 μV V3 155 μV AVR -4 μV v4 AVL 27 μV V5 197 197 μV AVF -11 μV Conclusion Conclusion : Sinus rhythm with heart rate 60/bpm Incomplete blockade of PNPG Possibly enlarged left atrium Impaired interatrial conduction Phenomenon of early ventricular repolarization ——=======Echocardiographic study (with calculations)=======—— Aorta diameter in the area of the sinuses of Valsalva 38 mm; diameter of the ascending aorta 32 mm; the walls are not changed. The left atrium diameter is 39 mm; indLP 1.81 cm/m2; LA volume 61 ml; LA volume index 28.24 ml/µV; MPP is not changed Left ventricle. MZhP 9 mm, CDR 50 mm, CL 10 mm, CDR index 2.31 cm/m2, FROM 0.38, EDV (Th) 118.24 ml, MM 169.80 g, IMM 78.61 g/m2 KDOV-mode 122 ml, EDC v-mode 46 ml , EDV index 56.48 ml/m2, ESV index 21.30 ml/m2, Simpson EF 62%, kinetics unchanged Right ventricle paramternal position 31 mm; 4-chamber 31 mm Right atrium area 17.3 cm2 Pulmonary artery 20 mm, estimated systolic pressure 23 mm Hg Inferior vena cava: 20 mm, burning on inspiration: >50% Aortic valve leaflets are not changed; Vmax 1.15 m/s, dPmax 5.32 mm Hg, no regurgitation The mitral valve leaflets are not changed; Ve 0.81 cm/s, Va 0.55 cm/s, Ve\Va 1.47, Tdec 137 ms, no regurgitation Tricusidal valve leaflets are not changed, regurgitation is valvular dPtr 17.74 mm Hg Pulmonary valve Vmax 0.73 m/s, dPmax 2 ,14 mm Hg, valvular regurgitation Description of the study: The heart chambers are not dilated. The walls of the LV are not thickened, the calculated values of the myocardial mass are not increased. Global contractility of the LV is not impaired. No zones of violation of regional contractility have been reliably identified. Normal diastolic function and LV filling pressure. E/Em-4.56 RV contractility according to TDI (TAVS = 14.0 cm/s) is preserved. TAPSE = 2.4 cm The IVS and IVS are located intact. During CDI mapping, no convincing evidence for transseptal blood shunting was obtained. The root, ascending section and arch (33 mm) of the aorta are not dilated, the walls are not changed. The pulmonary trunk is not dilated. The aortic valve is tricuspid, its crescents are not changed. Blood flow in the AC and in the LVOT is not accelerated. SV (LVOT) ~ 74ml. The leaflets of the mitral valve and tricuspid valves are not imzened. Mitral regurgitation is valvular. Tricuspid regurgitation, valvular. Estimated MPAP is not increased The amount of fluid in the periocardial cavity is not increased
The question is closed
aorta
maximum heart rate
estimated value