Chronic heart failure (CHF) is a disease characterized by the inability of the heart to pump a certain volume of blood sufficient to provide the body with oxygen. In severe heart failure, a gallop rhythm develops - an auscultatory phenomenon, which consists of the presence of an additional third sound. Cardiologists at the Yusupov Hospital determine it using modern diagnostic equipment from leading global manufacturers.
Severe cases of chronic heart failure with a gallop rhythm are discussed at a meeting of the Expert Council. Professors and associate professors, doctors of the highest category take part in his work. Leading specialists in the field of cardiology and arrhythmology collectively develop treatment tactics for patients.
CHF can be caused by many diseases of the cardiovascular system. The most common include coronary heart disease, hypertension, endocarditis and rheumatoid heart defects. Weakening of the heart muscle leads to the impossibility of normal pumping of blood, as a result of which the amount of blood released into the vessels gradually decreases.
The development of heart failure occurs gradually. In the early stages, the disease can only manifest itself during physical activity. Then it begins to be felt at rest. The appearance of characteristic symptoms at rest indicates that the disease has entered a severe stage. The progression of chronic heart failure threatens a significant deterioration of the patient’s condition, a decrease in his working capacity and even disability. The development of chronic liver and kidney failure, blood clots, and strokes may occur.
Conducting timely comprehensive diagnostics and competent treatment ensures a slowdown in the development of CHF and the prevention of dangerous complications of this serious disease. In order to stabilize the condition, a patient diagnosed with “acute and chronic heart failure” must adhere to the correct lifestyle: normalize his weight, follow a low-salt diet, limit physical and emotional stress.
Classification
Chronic heart failure develops gradually, going through four stages:
- The first stage – the patient has no restrictions on physical activity. During normal exercise, there is no weakness (lightheadedness), palpitations, shortness of breath or anginal pain;
- The second stage - physical activity is moderately limited, the patient is in a comfortable state at rest. Ordinary physical activity may cause weakness (lightheadedness), palpitations, shortness of breath, or anginal pain;
- The third stage – physical activity is limited. The patient's comfortable state is observed exclusively at rest. When performing physical activity, weakness (lightheadedness), palpitations, shortness of breath or anginal pain appears;
- At the fourth stage of chronic heart failure, performing any exercise is invariably accompanied by discomfort. Chronic heart failure syndrome also appears at rest. Even with minimal loads, discomfort increases.
CHF classification includes various types of disease, divided depending on the following parameters:
- forms (acute and chronic heart failure);
- localization (left ventricular, right ventricular and mixed heart failure);
- origin (myocardial, overload or combined chronic heart failure).
Make an appointment
Etiology and pathogenesis
The main cause of chronic heart failure is damage to the heart muscle or impairment of its ability to pump the required amount of blood through the vessels. Occurs in patients suffering from the following pathologies:
- Arterial hypertension – high blood pressure;
- IHD (coronary heart disease);
- Heart defects.
The development of CHF in women is most often caused by arterial hypertension. In men, chronic heart failure occurs as a consequence of coronary heart disease.
In addition, chronic heart failure can develop due to the presence of the following diseases and bad habits:
- diabetes mellitus;
- arrhythmias (heart rhythm disturbances);
- cardiomyopathies;
- myocarditis;
- alcoholism and smoking.
How is the rhythm of a quail formed?
In case of mitral valve stenosis, during auscultation the quail rhythm should be listened to at the top of the heart. The valve separating the left atrium from the ventricle is a bicuspid septum. These are two plates of connective tissue whose task is to prevent the backflow of blood into the atrium from the ventricle. Typically, during diastole, the valves open and press tightly against the muscle walls, allowing blood to flow freely. During contraction, the valves close tightly, preventing the backflow of blood.
One of the pathologies of the left-sided valve structure is stenosis. A healthy mitral valve covers an opening with an area of 4 to 6 square meters. see. Narrowing of the lumen between the atrium and the ventricle to 2 or less centimeters occurs when, due to inflammatory or other pathological processes, the tissue of the valves fuses with the edges of the atrioventricular opening, adhesions and scars form on it.
The valves become rigid (inelastic), so the sound of their closing is clearly audible. The quail rhythm is a clapping, loud sounding 1st heart sound and a split 2nd heart sound. The triple melody resembles the cry of a bird.
With mitral stenosis, the quail rhythm is caused by an increase in the first tone. It occurs because the left ventricle does not fill completely. Cardiomyocytes react by increasing tension (to push through an insufficient amount of blood they have to contract more), which causes an increase in sound. This is followed by the usual II sound, accentuated by the closure of the leaflets of another valve - the pulmonary valve.
Immediately after, an additional sound is produced by the mitral valve when it opens. It merges with the third normal tone and enhances the previous one, forming the phenomenon of splitting the second tone. The quail rhythm in mitral stenosis is one of the first “pre-electrocardiographic” symptoms of the disease.
Symptoms
The clinical picture of CHF is quite diverse and depends on the severity and duration of its course. The disease develops slowly over several years. Lack of treatment threatens serious deterioration of the patient's condition.
Most often, chronic heart failure is manifested by the following symptoms:
- Shortness of breath during physical exertion, when the patient moves to a supine position, and later at rest;
- Dizziness, fatigue and weakness;
- Nausea and lack of appetite;
- Edema of the lower extremities;
- Development of ascites (accumulation of fluid in the abdominal cavity);
- Weight gain due to swelling;
- fast or irregular heartbeat;
- Dry cough with pinkish sputum;
- Decreased intelligence and attention.
In severe heart failure, cyanosis (bluish color) of the skin and mucous membranes, heaviness in the right hypochondrium, swelling in the lower extremities, and an increase in abdominal volume due to fluid accumulation appear. During an objective examination of a patient with CHF in case of severe heart damage, a three-part rhythm can be heard. It is caused by weakening of the myocardium of the left ventricle and occurs as a result of rapid stretching of its walls under the pressure of blood flowing from the atrium. This creates a melody of a three-part rhythm (first, second and additional third tones) that resembles the clatter of a galloping horse - the “gallop rhythm”. It is better heard with a phonendoscope when the patient is lying on his left side. Patients with CHF are examined using:
- electrocardiography,
- echocardiography,
- magnetic resonance imaging of the heart.
Do pathological rhythms need to be treated?
Therapy in the presence of pathological rhythms in a patient is necessary only after a thorough examination and establishment of an accurate diagnosis. The type of medical institution where treatment will be carried out depends on the underlying disease. For example, hypertension, leading to left ventricular hypertrophy, can be dynamically observed in a clinic, and more severe pathologies (heart attack, myocarditis, severe heart failure) must be treated in a hospital setting. Mitral stenosis, when diagnosed for the first time, also requires further examination and selection of therapy in a hospital, where the need for surgical correction of the defect will be determined.
2012-2020 sosudinfo.ru
Go to section:
Diseases of the heart and aorta, arrhythmology, functional. diagnostics, cardiac pharmacology and surgery
Recommendations to SosudInfo readers are given by professional doctors with higher education and specialized work experience.
Risk group
The following risk factors, or at least one of them, can provoke the development of CHF. When several factors are combined, the likelihood of chronic heart failure increases significantly.
The risk group for the development of CHF includes patients suffering from:
- Coronary heart disease;
- History of myocardial infarction;
- Arterial hypertension;
- Heart rhythm disturbances;
- Diabetes mellitus;
- Congenital heart disease;
- Frequent viral diseases;
- Chronic renal failure;
- Alcohol addiction.
Pregnancy with CHF
The body of a pregnant woman has to overcome quite serious loads, including on the heart. Due to intrauterine growth and fetal development, the heart muscle must cope with the circulation of increased blood volume.
In women suffering from certain cardiovascular diseases, this heart function is often impaired, which leads to the development of CHF. The degrees of heart failure manifest themselves in different ways, but if even the slightest discomfort occurs, pregnant women should immediately inform their doctor.
Make an appointment
Diagnostics
When diagnosing CHF, doctors at the Yusupov Hospital take into account medical history data, characteristic symptoms and the results of a physical examination, instrumental and laboratory tests.
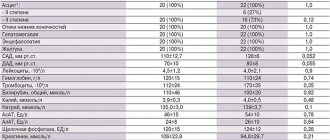
Patients are prescribed the following laboratory tests:
- General blood test - as a rule, there are no changes. Sometimes the presence of moderate anemia is determined;
- ESR (erythrocyte sedimentation rate) - an increase in ESR is observed with rheumatic heart disease or infective endocarditis, which resulted in the development of heart failure;
- A general urine test is performed to diagnose kidney complications and exclude the renal origin of edema. The most common possible manifestation of CHF is an increase in protein levels in the urine;
- Study of total protein and protein fractions - in CHF, their indicators decrease, which is associated with redistribution into the edematous fluid;
- Blood glucose level is important in order to exclude such a risk factor for CHF as diabetes;
- Indicators of cholesterol, low and high density lipoproteins - a clear relationship has been proven between high cholesterol levels and atherosclerosis, hypertension, coronary heart disease; elevated levels of lipoproteins and cholesterol in CHF may indicate a more severe course of the disease;
- The level of sodium and potassium in the blood - edema that occurs in patients with CHF is the cause of a significant decrease in the level of these microelements. Monitoring blood composition is especially important when taking diuretic drugs, as well as in cases where the patient has chronic heart and kidney failure;
- Study of the level of brain natriuretic propeptide, a protein whose formation in the heart muscle is associated with its excessive stretching and overload. Its circulation in the blood is quite long, so laboratory testing can easily determine its level. With increasing cardiac overload, the secretion of propeptide is activated. Therefore, its indicators are important for determining the severity of CHF.
Additionally, instrumental studies are prescribed, the scope of which is determined by the attending physician:
- Plain X-ray of the chest - to assess the position and size of the heart, exclude or confirm concomitant changes in the lungs (if the patient is suspected of chronic pulmonary heart failure);
- Electrocardiography (ECG) - to determine heart rhythm disturbances and the consequences of a previous myocardial infarction;
- Echocardiography - to differentiate systolic and diastolic heart failure, assess the activity of all parts of the heart, its size, the thickness of the heart muscle and its valves;
- Load tests – allow you to study the reaction of the heart muscle to increased physical activity;
- Coronarocardiography - the essence of this x-ray study is the introduction of a special contrast agent through a catheter directly into the vessels of the heart, thanks to which it is possible to diagnose coronary heart disease;
- Transesophageal echocardiography - ultrasound examination of the heart with placement of a sensor in the esophagus. Can be used if conventional cardiography does not provide a clear enough image, and also helps to identify blood clots in the right atrium in patients with atrial fibrillation;
- Stress echocardiography is an ultrasound examination of the heart at rest and after exercise or after the use of medications with an effect similar to exercise. The study allows you to assess the reserve capabilities of the heart and identify areas of viable heart muscle;
- Spiral computed tomography - during the procedure, X-rays are taken at different depths, which, in combination with MRI, provides an accurate image of the heart;
- Endomyocardial biopsy - during the diagnostic procedure, tissues of the muscle and inner lining of the heart are taken for histological examination, which makes it possible to clarify the cause of the disease in complex cases.
In addition, patients at the Yusupov Hospital are given consultations with therapists and cardiac surgeons.
Heart sounds are normal
The heart, like any other organ, creates certain sounds when working. This is due to the fact that blood is constantly moving in the heart, passing through the valves, and the valve flaps open and close, emitting sound vibrations. In addition, at the moment of stretching of the heart muscle of the atria and ventricles, vibration is created, which is layered with the sounds of slamming valve flaps.
Normally, at the points of projection of the heart valves onto the anterior chest (fifth intercostal space on the left, second intercostal space on the right and left, fourth intercostal space on the left), two heart sounds are heard - the first and second. In asthenic thin people, in children and adolescents, two more tones can be heard - the third and fourth, but their absence is not considered pathology.
Previously, it was believed that the first sound is formed when the atrioventricular valves close at the moment when blood flows from the atria into the ventricles, and then when the valves of the aorta and pulmonary trunk open, when blood flows from the ventricles into the aorta and into the pulmonary trunk. That is, the first sound characterizes the filling of the ventricles with blood and its expulsion further into large arteries. However, since 2004 (E. Braunwald), ideas about the nature of the origin of the first tone have changed somewhat - now it is generally accepted that such a sound is created not by the slamming of a valve, but by the impact of blood on the walls of the ventricle, when the blood first quickly fills the ventricles and then abruptly stops movement. The first sound is systolic, as it indicates systole (contraction) of the ventricles. The second sound is diastolic, as it is caused by diastole (relaxation) of the ventricles.
The second sound is formed a few hundredths of a second after the first and is formed by sounds that are created by the closure of the valves of the aorta and pulmonary trunk, as well as the oscillatory movements of the walls of these arteries.
distribution of heart sounds in the cardiac cycle
The first sound is normally heard at the point of projection of the mitral valve (at the apex of the heart), and the second sound is heard at the point of projection of the aortic and pulmonary valves. In terms of time, the constant change of two heart sounds is as follows: the first sound lasts 0.11 seconds, the pause between the first and second sounds lasts 0.2 seconds, the second sound lasts 0.07 seconds, and the pause between the second and first sounds lasts 0.42 seconds. A continuous set of heart tones, called the melody of the heart, normally sounds like this in letter designation:
– there – ta – there – ta – there – ta – I tone – II tone – I tone – II tone – I tone – II tone
Heart sounds and heart murmurs should not be confused. Between the two tones there are silent pauses, during which the blood flows directly, which normally occurs silently through the chambers of the heart. However, with heart defects or other pathologies of the heart valves, the blood stream has difficulty expelling from the heart chambers corresponding to the defect, so sound phenomena called murmurs occur. Noises can be heard in pauses between tones, or can be layered on top of them.
Drug treatment
CHF is a disease in which patients need to constantly take medications. For chronic heart failure, drugs are used that help slow the progression of the process and improve the patient's condition. In some patients with CHF, treatment requires surgical intervention.
Medicines for chronic deficiency are primary, auxiliary and additional.
The main drugs include ACE inhibitors (angiotensin-converting enzyme), angiotensin receptor antagonists, beta-blockers, aldosterone receptor antagonists, diuretics, ethyl esters of polyunsaturated fatty acids, cardiac glycosides. Cardiac glycoside for the treatment of chronic heart failure is used most often in patients with atrial fibrillation.
Auxiliary drugs for chronic heart failure are used in special clinical situations with complications of CHF. These include nitrates, calcium antagonists, antiarrhythmic drugs, antiplatelet agents, and non-glycoside inotropic stimulants. Additional medications for chronic insufficiency: statins, indirect anticoagulants.
For patients diagnosed with chronic heart failure, clinical recommendations from doctors relate not only to taking medications, but also to revising their lifestyle in general:
- It is necessary to stop smoking and drinking alcohol;
- Bring your weight back to normal;
- Follow a salt-free diet (diet for CHF should be balanced, contain sufficient amounts of proteins and vitamins);
- Walk more in the fresh air.
Treatment
When patients are diagnosed with gallop rhythm, CHF, doctors recommend adhering to a diet (limit the amount of salt consumed, ensure a sufficient amount of protein and vitamins in the diet), an optimal mode of physical activity, and maintaining normal body weight. Drug therapy for chronic heart failure is carried out with drugs from the following groups:
- ACE inhibitors;
- Angiotensin II receptor antagonists (ARBs or sartans);
- β-adrenergic receptor blockers;
- Mineralocorticoid receptor antagonists;
- Cardiac glycosides.
For uncontrolled blood pressure, patients are prescribed calcium agonists. Oral anticoagulants are used to prevent the risk of thromboembolism.
Electrophysiological methods of treating CHF (implantation of biventricular pacemakers for cardiac resynchronization therapy or implantation of cardioverter defibrillators) are carried out in addition to optimal drug therapy in patients who, after implantation of the device, can have a high level of quality and a life expectancy of at least one year.
Atrial flutter
Atrial flutter is a rapid, uniform rhythm of the atria, which contract at a frequency of up to 200-400 beats per minute. An attack of atrial flutter lasts from 1-2 seconds to several days.
Symptoms . For atrial flutter:
- general weakness develops, endurance decreases;
- discomfort appears in the chest, angina pectoris - pain behind the sternum;
- sudden attacks of rapid heartbeat develop;
- shortness of breath increases.
Diagnosis and treatment . The problem is diagnosed by ECG and ultrasound of the heart. Drug treatment is aimed at normalizing atrial contractions, preventing attacks and reducing the risk of blood clots. Beta blockers, potassium supplements, and anticoagulants are prescribed.
The Medicenter clinic diagnoses and prescribes effective treatment for all types of arrhythmia. Drug therapy is used and surgery is prescribed.