- How does it manifest?
- What causes fluid to accumulate?
- Risk factors
- Classification and types
- How to treat?
- Clinical case
- What causes ascites to develop in cancer?
- Features of the treatment of ascites in cancer patients
- Conservative therapy
- Surgery
- Diagnostic methods
- Possible complications
- Forecast
- Prevention
- Prices
Euroonco doctors specialize in working with patients with ascites. We have the following treatment features for this disease:
- We provide comprehensive treatment. During laparocentesis (a puncture of the abdominal wall to remove fluid from the abdomen), we install temporary or permanent peritoneal catheters, as well as port systems. This allows the patient not to be limited in movement.
- If this is indicated, the patient is prescribed a special diet with limited water and salt load.
- If this condition occurs against the background of cancer, chemotherapy may be performed. Thanks to this, we achieve improvement in the condition of such patients with advanced ovarian and colon cancer.
- Intracavitary chemotherapy is effective. After the fluid is removed, a chemotherapy drug is injected into the abdominal cavity. In approximately half of the cases, repeated evacuation of the fluid is not required for at least 2 months.
When a patient with cancer and ascites switches to complex therapy, laparocentesis is required 2–3 times less often than usual.
How does it manifest?
The presence of a small amount of fluid in the abdominal cavity does not manifest itself clinically. In addition, the human body normally produces and absorbs approximately 1.5 liters of fluid in the abdominal cavity per day. At the initial stage of this condition, patients have no special complaints, and fluid can only be detected during an ultrasound examination.
As the disease progresses, there is more fluid in the abdominal cavity, the person feels heaviness in the abdomen, and dull aching pain in the lower part. Subsequently, difficulty breathing, indigestion (nausea, belching, stool disorders) and urination problems occur. In the most severe forms, health deteriorates significantly, discomfort appears in the abdomen, shortness of breath occurs, early satiety occurs, an umbilical hernia forms, and swelling of the lower extremities appears.
5–10 liters of fluid, and sometimes 20 liters, can accumulate in the abdominal cavity. Because of this, internal organs are strongly compressed, intra-abdominal pressure increases, and the diaphragm is pushed into the chest cavity. This entails severe difficulty breathing. Due to the fact that resistance to blood flow increases in the abdominal organs, heart failure occurs. The consequence of long-term ascites is a violation of the drainage of the lymphatic system. Because of this, there is also a violation of lymphatic drainage in the lower extremities and, as a result, their swelling. There may also be a backflow of lymph into the internal organs. As a result, cancer cells enter healthy organs from the affected lymph nodes. This can trigger the development of metastases in the liver, stomach, pancreas and other organs. [4.8]
When there is more than one liter of fluid in the abdominal cavity, this can be noticed during a routine examination: the abdomen is enlarged or deformed, in an upright position it looks saggy, in a lying position the abdomen is flattened, the sides look swollen (the so-called “frog belly”). In thin patients, the navel often protrudes. A person may also experience hydrothorax, the presence of fluid in the pleural cavity. Typically, this condition develops in patients with congestive heart failure with long-standing ascites.
Mild or moderate ascites develops in 15 to 50 percent of patients in the early stages of cancer. Severe occurs in advanced stages in 7 to 15 percent of patients. [1]
In patients with advanced advanced cancer, exudative pleurisy is most common.
Book a consultation 24 hours a day
+7+7+78
Treatment of edema syndrome in chronic heart failure
For citation. Efremova Yu.E. Treatment of edematous syndrome in chronic heart failure // Breast Cancer. 2015. No. 27. pp. 1622–1624.
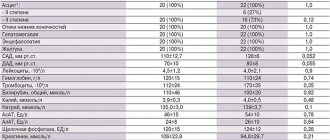
According to the European Society of Cardiology guidelines, heart failure is defined as a consequence of disturbances in cardiac structure and function that result in the inability of the heart to deliver oxygen at a rate comparable to the metabolic needs of the tissues, despite normal filling pressures [1]. Chronic heart failure (CHF) is a syndrome that results from various causes of myocardial damage. The main causes of CHF are coronary heart disease and arterial hypertension (AH), less often - cardiomyopathy, valvular heart disease, pericardial disease, etc. The prevalence of CHF in the age group of 25–54 years is 1%, in the group of 65–74 years – 4– 5%, about 10% – in people over 75 years of age. Compared to 20 years ago, there is evidence of a 4-fold increase in hospitalizations for CHF. This is partly explained by an increase in average life expectancy [2]. According to the results of the Russian epidemiological study EPOCHA-CHF, the prevalence of CHF in Russia averages 7.9%, including clinically significant - 4.5%, increasing from 0.3% in the age group from 20 to 29 years to 70 % in people over 90 years of age [3]. Having heart failure increases the risk of death by 4 times. Treatment of patients with CHF is a difficult task in modern medicine, since heart failure is only a syndrome that can develop as a complication of many diseases of the cardiovascular system. Therapy for a patient with CHF should first of all include treatment of the underlying disease. The main goal of treatment of CHF is to reduce mortality, as well as [2]: – reduction of clinical symptoms of CHF; – reduction in the incidence of major complications; – maintaining or improving the patient’s quality of life; – improvement of left ventricular function; – increased exercise tolerance; – reducing the need for hospitalization; – prevention of side effects of therapy. Drug treatment of CHF includes a large number of drugs, the most common of which are angiotensin-converting enzyme inhibitors (ACE inhibitors); angiotensin II receptor blockers; diuretics; β-blockers and mineralocorticoid receptor antagonists (aldosterone antagonists). The use of a specific drug in the treatment of CHF is aimed at solving specific problems. Let us consider in more detail the treatment of edema syndrome in CHF using diuretic therapy. Peripheral edema in heart failure is a consequence of fluid retention caused by reduced renal blood flow and neurohormonal changes. They predominantly develop on the lower extremities. With significant fluid retention, ascites and/or hydrothorax may be present. Diuretics are used to treat edema syndrome. Drugs of this class are indicated for all patients with clinical symptoms of CHF associated with excessive retention of sodium and water in the body [4]. Diuretics are used for the symptomatic treatment of CHF. They prevent fluid retention in the body, increase the excretion of salt and water, which leads to a decrease in congestion. Against the background of their use, the total peripheral vascular resistance decreases, the pre- and afterload decreases, and therefore the dilatation of the left ventricle decreases. There are 5 classes of diuretics (Table 1) that act on different parts of the loop of Henle. In the initial stages of CHF, the use of thiazide diuretics is possible. In severe CHF, a combination of loop and thiazide diuretics is possible, which leads to an increased diuretic effect. In case of severe edema syndrome and/or decompensation of CHF, it is advisable to administer diuretics parenterally. The loop diuretics furosemide and torsemide are the most commonly used diuretics for CHF.
Torsemide has been used in clinical practice since the 1980s. For edema syndrome, this drug is prescribed 5 mg in the morning after meals; if necessary, the dose is increased to 20 mg 1 time/day. Compared with furosemide, torasemide is characterized by higher bioavailability, which does not decrease with edematous syndrome, has less effect on the plasma concentration of potassium and magnesium, acts longer and has anti-aldosterone properties (blockade of aldosterone receptors on the membranes of epithelial cells of the renal tubules and decreased secretion of aldosterone in the adrenal glands) . The pleiotropic properties of torasemide include the ability of this drug to inhibit the synthesis and deposition of type 1 collagen in the myocardium in patients with CHF. In addition, unlike patients receiving furosemide, patients in the torasemide group had a decrease in the serum concentration of the C-terminal propeptide of type 1 procollagen (a marker of myocardial fibrosis) [6]. Torsemide reduces mortality, as well as the frequency and duration of hospitalizations for CHF. In addition, it leads to increased exercise tolerance, improves the functional class (FC) of CHF (according to NYHA) and the quality of life of patients. In the TORIC study among 1377 patients with CHF, torasemide led to a significant reduction in cardiovascular mortality compared with furosemide [7]. This study analyzed the results of a 9-month comparative treatment with torasemide at a daily dose of 10 mg and furosemide 40 mg in patients with CHF. In the group of patients receiving torsemide therapy, the FC of circulatory failure improved significantly more often and cardiovascular and overall mortality significantly decreased. Recently, slow-release torasemide has appeared on the Russian drug market - Britomar
®. The drug provides gradual release of the active substance. Due to this, fluctuations in the concentration of the drug in the blood are reduced compared to the usual form. Britomar® is a tablet based on a hydrophilic matrix of guar gum, which is a natural water-soluble polymer obtained from the seeds of a plant of the legume family. In the pharmaceutical industry, guar gum is widely used to create sustained-release dosage forms. In the gastrointestinal tract it forms a kind of sponge, which provides a slow release of the drug. The drug substance is released over a longer period of time, due to which diuresis begins approximately 1 hour after taking the drug, reaching a maximum after 3–6 hours, the effect lasts from 8 to 10 hours. Slow release of the drug allows for additional clinical benefits in the treatment of edema syndrome in CHF. Torsemide, when used long-term, does not cause changes in blood potassium levels, does not have a noticeable effect on calcium and magnesium levels, glycemic and lipid profiles [8]. The drug does not interact with anticoagulants (warfarin), cardiac glycosides or organic nitrates, other drugs most often used in the treatment of CHF, such as β-blockers, ACE inhibitors, angiotensin II receptor blockers and mineralocorticoid receptor antagonists. Long-acting torasemide has been studied in a number of studies in comparison with other diuretics. Thus, in a Russian single-center, randomized, open-label study, the comparative effectiveness of long-acting torasemide and furosemide was studied in patients with class II–III CHF, edematous syndrome, and elevated levels of natriuretic peptides [9]. The study included 40 patients with CHF of ischemic etiology with a left ventricular ejection fraction of less than 40%, divided by randomization into 2 equal groups: the 1st received long-acting torasemide (Britomar®), the 2nd received furosemide. In both groups, during treatment, a significant improvement in exercise tolerance, an improvement in the quality of life of patients, and a decrease in the concentration of natriuretic hormones were observed. In the torasemide sustained-release group, a trend towards a more significant improvement in quality of life (p=0.052) and a significantly more significant decrease in NT-pro-brain natriuretic peptide levels (p<0.01) were identified. This may be due to the fact that extended-release torasemide has a slow onset of action, does not lead to the development of urinary urgency, and has a longer duration of action compared to the standard-release dosage form [9]. This study also examined data on the effect of diuretic treatment regimens on the electrolyte profile of patients. Potassium and sodium concentrations were determined at baseline, 2, 4 and 12 weeks. treatment. There were no cases of changes in the electrolyte profile compared to normal values in the torasemide extended-release group. In the furosemide group, 3 (15%) patients experienced a decrease in potassium levels below normal limits (3.5 mmol/l), in 1 case requiring dose adjustment of aldosterone antagonists and intravenous infusion of potassium salts. Undoubtedly, reducing the frequency of hypokalemia also has an impact on both the well-being of patients and the frequency of potential complications of therapy. While taking long-acting torasemide, the phenomenon of increased post-diuretic sodium reabsorption can be avoided. The absence of a rapid increase in the volume of excreted urine does not cause a sharp change in the volume of circulating blood, and therefore does not potentiate the excessive synthesis of A-II and norepinephrine, which lead to a decrease in the glomerular filtration rate and deterioration of renal function. The benefits of extended-release torasemide compared with standard-release torsemide have been demonstrated in a number of studies. In a study by MJ Barbanoj et al. a comparative assessment of bioavailability and bioequivalence was carried out and the pharmacokinetics and pharmacodynamics of torasemide sustained and standard release were assessed [11]. Two doses of extended-release torsemide were compared with similar dosages of torasemide. 20 healthy volunteers (2 groups, 10 people each) took part in the study. As a result, sustained release torasemide showed a significantly longer tmax compared to that of torsemide. The amount of torasemide detected in urine 24 hours after administration was higher in the sustained-release torasemide group at both dosages. Urine volume and urinary electrolyte excretion were lower in the sustained-release torasemide group during the first hour after dosing, but natriuresis was significantly greater in this group. Thus, although both forms showed similar systemic distribution (AUC), sustained-release torasemide had a lower absorption rate (smaller C (max) and prolonged t (max)). In a pilot study by G.P. Arutyunova et al. a comparison of sustained release torasemide with standard release torasemide was also carried out [12]. This open, randomized, comparative clinical trial in parallel groups included patients with FC I–II CHF (NYHA) and grade II–III essential hypertension. Using the random number method, patients were divided into 2 treatment groups - treatment with Britomar and standard release torsemide. The treatment period lasted 40 days. As a result, it was shown that the total natriuresis on the 1st day of administration of Britomar and torasemide standard release was greater in the second group, however, it is important that in the Britomar group a smooth natriuresis was observed during the day without peaks, in contrast to the standard form of torasemide, when prescribed which causes a peak increase in natriuresis at 3 hours and a sharp decrease already at 6 hours with a further progressive decrease. It was also shown that natriuresis following a single dose of a loop diuretic lasted only a few hours, and after 5-6 hours, urinary sodium excretion approached a level comparable to that with placebo, i.e., from 6 to 24 hours, even torsemide is ineffective , and its cumulative natriuresis is comparable to that of hydrochlorothiazide precisely due to the presence of an antinatriuretic period. A beneficial effect of Britomar on central hemodynamic parameters was demonstrated, which the authors associate with the absence of rebound sodium retention when using this diuretic, and therefore an increase in the rigidity of the vascular wall. Thus, sustained-release torasemide, due to its pharmacodynamics and pharmacokinetics, is a highly effective drug in the treatment of edema syndrome in CHF and can improve the quality of life of patients and the tolerability of therapy.
What causes fluid to accumulate?
Pathological accumulation of fluid in the abdominal cavity occurs in certain diseases in which the regulation of water-salt metabolism and normal circulation are disrupted. The reason may be:
- Oncological diseases: secondary peritoneal carcinomatosis, lymphoma and leukemia, metastases in the hepatic portal area, primary mesothelioma.
- Diseases of the liver and its vessels: liver cancer, portal hypertension, liver cirrhosis, veno-occlusive disease, Budd-Chiari disease.
- Peritonitis (inflammation of the peritoneum) of various origins: pancreatic, fungal, parasitic, tuberculous.
- Congestive heart failure, constrictive pericarditis.
- Other diseases: ovarian tumors and cysts (Meigs syndrome), pancreatic cyst, Whipple's disease, sarcoidosis, systemic lupus erythematosus, myxedema.
Euroonco treats ascites of various origins. But since our main work is related to the treatment of malignant neoplasms, a significant part of our patients are cancer patients. [4,5]
Causes of pathology in adults
In many cases, pathology develops as a symptom of a number of diseases, including:
- Portal hypertension;
- Cirrhosis;
- Hepatitis;
- Thrombosis of the liver veins.
It is possible that the cause of the pathology is blood oncology, as well as pathologies whose nature has nothing in common with the tumor.
Heart failure can also cause pathology. Problems associated with lymph circulation and the activity of organs such as the thyroid gland and kidneys can also cause pathology.
Protein deficiency
Risk factors
Among the risk factors for the development of ascites, pathologies that can lead to liver cirrhosis are of greatest importance. First of all, these are viral hepatitis B and C, alcoholic hepatitis. Other most common risk factors:
- congestive heart failure;
- renal failure;
- obesity;
- diabetes mellitus type II;
- increased levels of “bad” cholesterol in the blood. [eleven]
Risk factors
The main risk factor is a malignant tumor. The peritoneum itself looks like a sheet covered with a mucous membrane and is an ideal place for the development of metastases.
They penetrate there through the blood vessels, breaking away from the tumor focus, and force the serosa to reproduce excess liquid mass.
In addition, in the lymph vessels, atypical cells grow and block them, thereby disrupting the absorption of the liquid mass.
Factors that contribute to the accumulation of excess fluid mass in oncology are:
- Cirrhosis;
- Liver dysfunction as a result of a chronic disease or toxic hepatitis;
- Heart disease that slows blood flow;
- Failure of kidney excretory function as a result of chemotherapy;
- Increased thrombus formation in the vessels of the peritoneal cavity;
- Changes in the protein composition of the blood as a consequence of gastrointestinal carcinoma.
Classification and types
Classically, depending on the level of protein in ascitic fluid, ascites is divided into exudative (25 g/l or more) and transudative (<25 g/l). This allows us to indirectly judge the reasons. Currently, a more accurate indicator is used - the serum albumin-ascitic albumin gradient (SAAG):
- When SAAG is more than 1.1, the cause of ascites is usually pathologies such as cirrhosis, congestive heart failure, and Budd-Chiari disease. They are associated with increased pressure in the portal vein.
- If SAAG is less than 1.1, it can be assumed that the accumulation of fluid in the abdomen is caused by pancreatitis or cancer.
According to the clinical course, the following types of ascites are distinguished:
- Depending on the severity of the current:
- 1st degree. There are no clinical manifestations; the diagnosis is established by ultrasound (determining the level of free fluid in the abdominal cavity).
- 3rd degree. Significant visual enlargement of the abdomen.
2nd degree. Slight visual enlargement of the abdomen.
- Resistant to diuretics: treatment with diuretics in combination with a diet in which sodium chloride intake is limited to less than 2 g per day is ineffective (no effect after 1 week of therapy).
Uncontrolled by diuretics: It is impossible to use diuretics because they cause significant side effects. [6,7]
Diet
A very important goal is to restore nutritional status and normalize the level of proteins that were lost during the evacuation of the liquid mass.
Restriction of fluid and salt intake is required. It is necessary to exclude canned food, marinades and fast food from the patient’s diet, as they contain excess salt.
Insufficient protein levels are compensated by IVs and a selected diet. Patients with cancer need to consume protein at the rate of one and a half grams for every kilogram of weight.
How to treat?
There are several main methods for treating ascites in patients with cancer:
- conservative therapy (aldosterone antagonists, diuretics) - aimed at normalizing water-salt metabolism and reducing the formation of fluid in the abdominal cavity;
- laparocentesis - puncture of the abdominal wall under ultrasound control; used not only for removing fluid, but also for installing drainage, which will serve for long-term removal of fluid;
- palliative surgical operations - peritoneovenous shunt, omentohepatophrenopexy, deperitonization of the abdominal walls and others. [1.9]
Traditional methods of treating ascites caused by cancer do not have proven effectiveness and safety, therefore they are not used at Euroonko.
If you come to our clinic with ascites due to cancer, we recommend getting a second opinion regarding the treatment of the underlying disease from our clinical oncologists and chemotherapists.
Clinical case
A 59-year-old woman, Sh., was diagnosed with stage IV ovarian cancer (adenocarcinoma), ascites, and chronic pain syndrome 2 b according to the ShVO. The patient noticed an increase in the abdomen up to 120 cm in circumference, difficulty breathing, and weight loss. Specific treatment at the place of residence was denied. According to the patient, she was “sent home to die.” Read more…
A 59-year-old woman, Sh., was diagnosed with stage IV ovarian cancer (adenocarcinoma), ascites, and chronic pain syndrome 2 b according to the ShVO.
The patient noticed an increase in the abdomen up to 120 cm in circumference, difficulty breathing, and weight loss. Specific treatment at the place of residence was denied. According to the patient, she was “sent home to die.” Patient Sh. was urgently hospitalized in the specialized department of Euroonko, after active symptomatic therapy aimed at normalizing blood counts and restoring water and electrolyte balance, a peritoneal port was installed. Resolution of ascites was carried out under the control of plasma protein levels. The use of peritoneal ports allows for the removal of ascitic fluid in fractional doses, which ultimately eliminates the occurrence of serious complications in the form of hemorrhagic syndrome associated with hemodilution and coagulopathy as a result of massive entry of ascitic contents into the venous bed.
After stabilization of the general condition, against the background of nutritional support, antiemetic and antisecretory therapy, patient Sh. received specific chemotherapy treatment with good effect. Upon resolution of ascites in the presence of a peritoneal port, intra-abdominal chemotherapy became possible.
Six months after the described hospitalization, the patient returned to her usual lifestyle and continues to receive systemic treatment on an outpatient basis under the supervision of a team of Euroonco specialists. The response to treatment is regarded as positive in the absence of ascites and a total reduction in the size of the lesions by more than 70%. Combined treatment in the format of systemic and local (intra-abdominal) therapy with implantation of a port system is the optimal treatment regimen for this group of patients. In the practice of Euroonco doctors, such cases occur on a regular basis. Hide
What causes ascites to develop in cancer?
The most common cancers that cause fluid accumulation are:
- ovarian cancer (in 25–30 percent of patients),
- mammary cancer,
- uterine cancer,
- stomach cancer,
- colon cancer. [2]
The accumulation of fluid in the abdominal cavity during cancer occurs due to the fact that the peritoneum (the membrane lining the inside of the abdominal wall and covering the organs located in it) is affected. Tumor cells settle on its parietal and visceral layers, resulting in disruption of lymphatic drainage. This causes deterioration in fluid absorption. Typically caused by tumors of the gastrointestinal tract and ascites in ovarian cancer.
When a tumor or metastases forms in the liver, the reason for the accumulation of fluid in the abdominal cavity is different: the venous system of the liver is compressed and the natural venous outflow from the intestine is disrupted. This condition develops quickly and usually lasts longer and is more severe. 15 percent of cancer cases occur in this particular form.
Abdominal lymphoma causes ascites through blockage and effusion (leakage) of lymph from the intra-abdominal lymph ducts. [2.6]
Causes
The basis for the development of the disease is pathology: during the normal functioning of the peritoneal cavity, no significant amount of liquid mass is discharged. It is only insignificant, just to avoid adhesions from sliding intestinal loops. The liquid released for this purpose constantly flows back.
When the usual operation of this mechanism is disrupted, the function of secretion of the liquid mass is destabilized, as well as the function of its outflow. The consequence of such destabilization is the accumulation of excess liquid mass inside the abdomen.
Features of the treatment of ascites in cancer patients
In hospitals that do not specialize in the treatment of cancer, the approach to patients with ascites may be ineffective due to the characteristics of this condition. For example, the main treatment may be the use of diuretics, aldosterone antagonists, and dietary changes to limit water and salt load. The effectiveness of this approach for reducing portal hypertension is relative; in cancer patients, fluid accumulation in the abdominal cavity is caused by peritoneal carcinomatosis. Therefore, conservative therapy cannot be the main treatment method in such patients.
Typically, fluid is removed from the abdomen using laparocentesis (abdominal paracentesis). This is a surgical procedure that is performed by a surgeon and an anesthesiologist-resuscitator. [3.10]
Ascites
shutterstock.com/Getty Images
Share
Ascites is an accumulation of fluid in the abdominal cavity.
Causes of ascites
Most often, ascites occurs with kidney disease, heart failure, nutritional dystrophy, cirrhosis of the liver, due to damage to the lymphatic thoracic duct, peritoneum (tuberculosis, cancer, etc.), as a result of compression of the trunk of the portal vein of the liver or thrombosis of its branches. In newborns, ascites develops when there is hidden blood loss or when the fetus has hemolytic disease. In children under three years of age, ascites is usually associated with liver disease, but can also be the result of exudative enteropathy, chronic nutritional disorders, and also a manifestation of nephrotic syndrome. The occurrence of ascites is facilitated by disturbances in water-salt metabolism.
Clinical signs of ascites
Fluid accumulating in the abdominal cavity in large quantities (sometimes more than 20 liters) causes the diaphragm to be pushed into the chest cavity and an increase in intra-abdominal pressure. The result of this is restriction of lung movement (up to respiratory failure), heart function is disrupted, and protein deficiency develops. Ascites can be determined clinically only if there is at least one liter of fluid in the abdominal cavity. On examination, an enlarged abdomen, sagging, and protrusion of the navel are noted. In a patient lying down, the lateral parts of the abdomen bulge, he is flattened (“frog belly”). The venous network is clearly visible on the skin of the abdomen. Twisted, swollen and dilated veins are concentrated around the navel and extend from it in the form of rays, forming the so-called “head of Medusa”. When percussing the abdominal cavity above its lateral or sloping part, a dull sound is heard. When the position of the body changes, the limit of dullness also changes. With your palm placed on the side of one side of the abdomen, you can feel the tremors that occur when you tap the fingers of the other hand on the opposite side (the so-called fluctuation symptom). X-ray examination and percussion determine the limitation of diaphragm mobility. In patients with ascites complicated by heart failure, hydrothorax (fluid in the pleura) is often observed.
Diagnosis of ascites
The main diagnostic task is to establish the underlying disease, which resulted in ascites. In cirrhosis, ascites is often combined with bleeding from the veins of the esophagus and is accompanied by the development of collaterals under the skin of the abdomen. In heart failure complicated by ascites, swelling of the feet and legs and acrocyanosis are observed. In renal failure, swelling of the subcutaneous tissue and skin is common.
For diagnosis, puncture of the abdominal cavity with further examination of the resulting fluid is of great importance. In patients with heart failure and liver cirrhosis, the fluid is clear, contains mainly endothelial cells, and the protein concentration is no more than 2.5%. In peritoneal cancer, cancer cells are found in the fluid. In children under three years of age, ascites must be differentiated from pseudoascites, which can be observed with cystic fibrosis and celiac disease.
Treatment of ascites
Aimed at eliminating the underlying disease. To reduce the amount of fluid, aldosterone antagonists and diuretics are used to normalize water-salt metabolism. If medication methods are ineffective, abdominal puncture is indicated. Surgical treatment of ascites is used to reduce portal hypertension and create the necessary conditions for fluid absorption by nearby tissues. The prognosis of the underlying disease when complicated by ascites worsens.
Conservative therapy
Conservative therapy is used in the treatment of small and moderate ascites. In other words, if there are no tiring and debilitating symptoms: pain, rapid breathing (tachypnea), etc. Up to 65% of patients have an improvement in their condition when treated with diuretics - this way you can remove up to 1 liter of fluid per day. [5]
In the later stages of cancer, reducing salt and water intake can reduce quality of life. Therefore, at Euroonko such diet correction is rarely prescribed.
Book a consultation 24 hours a day
+7+7+78
Education
Excessive accumulation of liquid mass does not occur immediately, so human organs during this process adapt to changes in intraperitoneal pressure.
The international classification distinguishes three degrees of pathology:
- The first degree is characterized by a minimal volume of liquid mass, which is detected by ultrasound of the peritoneal cavity;
- Stage two - accumulation of liquid mass is determined by liters, the stomach increases;
- The third degree is called tense ascites, the person’s condition is assessed as serious.
As a rule, tense ascites is characterized by the accumulation of more than 10 liters of fluid in the peritoneal cavity.
Surgery
Ascites in cancer must be treated surgically when it:
- Refractory, that is, not amenable to conservative treatment.
- Large, that is, if it is necessary to remove up to 6–10 liters of fluid at a time (this difficult procedure is carried out for strict medical reasons).
- Giant. In this case, a combined operation is needed, which includes removing a large volume of fluid (up to 5–7 liters) on the first day and removing the remaining volume at a rate of no more than 1 liter per day for 7–10 days.
In the classic version, laparocentesis is performed on an empty bladder, the patient sits down, and the seriously ill person is placed on his side. [4]
It is dangerous to perform laparocentesis without observing the rules of asepsis and antisepsis. Therefore, the release of fluid is carried out only in a specialized medical institution with a license to perform surgical interventions and with a hospital. If the patient is in serious condition, it is difficult for him to move, an ambulance team is called for him.
First, local anesthesia is performed, then, under ultrasound guidance, a puncture is made with a trocar (an instrument in the form of a thin tube with a sharp end) along the midline of the abdomen or along the line connecting the navel to the iliac crest. Usually no more than 5–6 liters of liquid are removed at a time. To prevent blood pressure from dropping sharply and vascular collapse, the fluid is released slowly.
In accordance with the classical technique, the patient needs to lie for several hours on the side free from the puncture. If at this time a small amount of liquid continues to be released, then a reservoir is applied, which is removed after a day or two.
If it is necessary to remove a large amount of liquid, then a loss of protein and salts occurs, which becomes the cause of protein deficiency. To prevent such a complication, the patient is given albumin. With repeated puncture, another complication may arise - fusion of the omentum (part of the peritoneum) or intestine with the anterior wall of the abdomen. Because of this, intestinal function deteriorates significantly, and during subsequent punctures serious complications can develop. [4,6]
With the modern approach to laparocentesis, fluid drainage occurs primarily through a permanent peritoneal catheter. At the same time, the deficit in circulating blood volume is replaced by plasma expanders (from the English plasma expander - increasing plasma volume). Typically, 10–20% albumin solutions are used for this. In some cases, aminosteril, polyglucin, rheopolyglucin (dextran-40), hemacell and new starch-based preparations (refortan, stabizol, HAES-steril) can be used instead of albumin. This alternative only helps to compensate for fluid deficiency in the blood, but these drugs do not affect protein deficiency.
Some patients with ascites undergo omentohepatophrenopexy. This is a laparoscopic operation in which the omentum is sutured to areas of the surface of the liver and diaphragm. Due to the fact that contact occurs between the omentum and the liver, conditions appear for the absorption of ascitic fluid by nearby tissues. If the patient has peritoneal carcinomatosis, surgery is performed to a limited extent. Typically, in such patients, omentohepatophrenopexy becomes part of palliative treatment. [6,7]
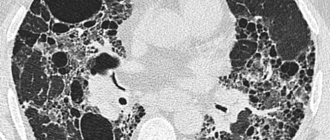
Diagnostic methods
If more than 500 ml of fluid has accumulated in the abdomen, the doctor may identify symptoms during an examination. Ultrasound is used to confirm the diagnosis. Sometimes ascites is discovered accidentally during an ultrasound or computed tomography scan of the abdomen, which is performed for another reason.
Euroonco operates a comprehensive gastrointestinal screening program, which helps assess the condition of the digestive system. It, in particular, includes an ultrasound of the abdominal cavity with determination of the level of free fluid. This helps diagnose ascites at an early stage.
It is important not only to identify fluid in the abdominal cavity, but also to understand the reasons for its accumulation - this helps to assess the prognosis and prescribe effective treatment. In most cases, the examination includes the following laboratory tests:
- Biochemical blood test - complete biochemical panel. It helps assess the condition and function of the liver, kidneys, and electrolyte levels.
- Blood clotting study.
- Study of ascitic fluid obtained during laparocentesis. For analysis you need a little of it - usually 20 cm³, less than a tablespoon. It examines the level of red and white blood cells, total protein, albumin, amylase, glucose, and examines for pathogenic microorganisms. A cytological examination is performed to help identify cancer cells. [6]
Possible complications
If a lot of fluid accumulates in the abdominal cavity, the functioning of the internal organs is disrupted, difficulties arise during breathing, as the mobility of the diaphragm is limited, and effusion forms in the pleural cavity.
With increased portal vein pressure, bacteria from the intestine can spontaneously enter the ascitic fluid and cause spontaneous bacterial peritonitis .
In rare cases, a very serious complication develops - hepatorenal syndrome . This term refers to impaired renal function with severe liver damage, up to severe renal failure. The exact mechanism of development of this condition is unknown, but it is believed to occur due to impaired renal blood flow, excessive use of diuretics and intravenous contrast agents. [4]
Stages of severity
There are three stages of abdominal hydrops depending on the amount of accumulated fluid:
- Initial stage - up to one and a half liters of fluid accumulates in the abdominal cavity;
- Moderate ascites - manifested by an increase in the size of the abdomen, edema of the lower extremities. The patient is concerned about severe shortness of breath, heaviness in the abdomen, heartburn, constipation;
- Severe dropsy - from 5 to 20 liters of fluid accumulates in the abdominal cavity. The skin on the abdomen tightens and becomes smooth. Patients experience heart failure and respiratory failure. When the fluid becomes infected, ascites-peritonitis (inflammation of the peritoneal layers) develops.
Forecast
Ascites in cancer significantly worsens the prognosis. From the moment of diagnosis, only half of the patients remain alive within 1–4 months. The average life expectancy is from 20 to 58 weeks. Timely treatment in a clinic that specializes in working with such patients helps improve survival. If the accumulation of fluid in the abdominal cavity is caused by cirrhosis of the liver, when there is no cancer, the prognosis is better, and if there is chronic heart failure, with appropriate treatment, you can live for years. [6]
Symptoms
The main manifestation of ascites is a significant increase in size and pathological bloating of the abdomen. Signs of abdominal dropsy can increase rapidly or over several months. Ascites is manifested by the following clinical symptoms:
- Feeling of fullness in the abdominal cavity;
- Pain in the abdomen and pelvis;
- Increased gas formation (flatulence);
- Belching;
- Heartburn;
- Digestive disorders.
Visually, the patient’s abdomen enlarges, in a horizontal position it hangs down and begins to “blur” on the sides. The navel gradually protrudes more and more, and blood vessels are visible on the stretched skin. As ascites develops, it becomes difficult for the patient to bend over and shortness of breath appears.
Doctors at the Oncology Clinic evaluate the clinical manifestations of the disease and carry out a differential diagnosis of cancer with other diseases, the manifestation of which is ascites.
Prices
Euroonko has a special offer for drainage of ascites in a day hospital - 63,300 rubles.
The program includes:
- Examination and consultation with an oncologist surgeon.
- Complete blood count, biochemical blood test, ECG.
- Ultrasound of the abdominal organs with determination of the level of free fluid
- Conducting laparocentesis with ultrasound navigation.
- Complex drug therapy aimed at restoring water and electrolyte balance.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Pharmacotherapy of tumors. Dedicated to the memory of Mikhail Lazarevich Gershanovich // A.N. Stukov and the team of authors / Ed. A.N. Stukova, M.A. Blanca, T.Yu. Semiglazova, A.M. Belyaeva. St. Petersburg: Publishing House ANO “Oncology Issues”, 2021, 512 p.
- Willert A.B., Kolomiets L.A., Yunusova N.V., Ivanova A.A. Ascites as a subject of research in ovarian cancer. Siberian journal of oncology. 2019; 18 (1): 116–123. – doi: 10.21294/1814-4861-2019-18-1-116-123.
- Willert A. B., Kolomiets L. A., Yunusova N. V. Ascites as a tumor microenvironment in ovarian cancer: relationship between prognosis and chemoresistance. Advances in Molecular Oncology 2019;6(2):8–20.
- Yu.M. Stepanov, I.N. Kononov, T.A. Skorokhod, Ascites associated with intraperitoneal rupture of the bladder and urinary peritonitis. Clinical decline of current gastroenterology, 4 (66) • 2012.
- T.A.Baeva, D.N.Andreev, E.M.Mironova, D.T.Dicheva - Ascites: differential diagnosis and treatment. — Directory of a polyclinic doctor. No2, 2021.
- Alekseichik, S. E. Ascites. Differential diagnosis: method. recommendations / S. E. Alekseychik. – Mn.: BSMU, 2005. – 28 p.
- V.T. Ivashkin, M.V. Mayevskaya, Ch.S. Pavlov, E.A. Fedosina. Clinical recommendations of the Russian Society for the Study of the Liver and the Russian Gastroenterological Association for the treatment of complications of liver cirrhosis. Ros journal gastroenterol hepatol coloproctol 2016; 26(4).
- J. T. Tamsma, H. J. Keizer, A. E. Meinders. Pathogenesis of malignant ascites: Starling's law of capillary hemodynamics revisited. - Annals of Oncology 12: 1353-1357. 2001.
- Rony A Adam, Yehuda G Adam. — Malignant ascites: past, present, and future. - VOLUME 198, ISSUE 6, P999-1011, JUNE 01, 2004. DOI: https://doi.org/10.1016/j.jamcollsurg.2004.01.035
- Michelle Meier, Frank V. Mortensen, Hans Henrik Torp Madsen. — Malignant ascites in patients with terminal cancer is effectively treated with permanent peritoneal catheter. — Acta Radiologica Open 4(7) 1–7. DOI: 10.1177/2058460115579934.
- RC Oey, HR van Buuren, RA de Man. — The diagnostic work-up in patients with ascites: current guidelines and future prospects. OCTOBER 2021, VOL. 74, NO. 8