Treatment of stage 2 hypertension, symptoms and causes
Stage 2 hypertension is arterial hypertension in moderate form. The upper blood pressure (systolic) is 160 - 179 mm Hg, and the lower blood pressure (diastolic) is 100 - 109 mm Hg. At this stage of the disease, periods of increased pressure are longer than with stage 1 hypertension. Arterial blood pressure in grade 2 hypertension rarely returns to normal.
Depending on the rate of change in the degree of hypertension, we can talk about normal and malignant arterial hypertension. In the second case, the disease progresses so quickly that it is often fatal. Hypertension is dangerous because an increase in the speed of blood movement through the vessels leads to thickening of their walls and an even greater narrowing of the arteries.
Risks of developing hypertension
The risk of developing hypertension or arterial hypertension - high blood pressure - consists of a number of factors. Accordingly, the more there are, the greater the likelihood that a person will become hypertensive.
Risk factors for developing hypertension:
- stress (stress hypertension) and mental stress. The stress hormone adrenaline increases your heart rate. It instantly constricts blood vessels;
- taking certain medications, for example, oral contraceptives, and various dietary supplements (iatrogenic hypertension);
- male gender;
- age over 35 years;
- pregnancy;
- diabetes;
- endocrinopathy of the adrenal glands, thyroid gland or pituitary gland;
- diseases of the hypothalamus;
- pyelonephritis;
- renal failure (nephrogenic hypertension);
- inactivity. Physical inactivity is accompanied by a slow metabolism - metabolism - and gradually weakens the body as a whole;
- excess salt in food. Table salt provokes arterial spasm and retains fluid in the body;
- excess body weight. Each extra kilogram increases blood pressure by 2 millimeters of mercury - mmHg;
- sudden change in weather;
- hereditary predisposition. The risk of getting sick is higher for those who have hypertension among first-degree relatives: father, mother, grandmothers, grandfathers, siblings. The more close relatives suffer from high blood pressure, the greater the risk;
- bad habits: smoking or drinking alcohol. Components of tobacco provoke spasms of blood vessels - involuntary contractions of their walls. This narrows the blood flow;
- atherosclerosis – blockage of blood vessels with plaques. Total cholesterol should not exceed 6.5 mmol/l of blood;
- chronic lack of sleep and other “provocateurs”.
Depending on the combination and degree of manifestation of the above factors, as well as the likelihood of cardiovascular complications in the next decade, there are 4 types of risk of developing arterial hypertension:
- low (risk less than 15%);
- average (from 15 to 20%);
- high (more than 20%);
- very high (more than 30%).
Risk factors for the appearance of arterial hypertension are also divided into 2 types based on the possibility of their elimination: correctable (correctable) and not. For example, a person may well quit smoking, but he is not able to change his ancestry. The amount of risk is summed up from a number of indicators. A patient with stage 1 hypertension who begins to abuse alcohol will significantly increase the percentage chance of developing complications.
Factors provoking arterial hypertension, features of the course of stage 1 disease, prognosis
High blood pressure is one of the common complaints voiced by patients when visiting a cardiologist. The reason for this phenomenon lies in the regular impact of adverse factors on humans. A modern resident of a metropolis is in a state of stress most of the time, eats unhealthy foods, moves little, and has bad habits. The initial stage in the development of dangerous health changes is stage 1 arterial hypertension. If such a diagnosis is confirmed, a person must begin treatment and strictly follow the doctor’s recommendations on taking preventive measures.
Under what conditions is the diagnosis established?
The main sign of hypertension is stable blood pressure (BP) levels equal to or exceeding 140/90 mmHg. The main factor in its stable preservation is a change in blood flow and a decrease in its speed. Reducing the internal lumen of blood vessels causes the heart to begin to work intensively, the body tries to restore blood circulation, as a result, the pressure inside the arteries increases. It is under such conditions that arterial hypertension occurs, the 1st degree of which is initial. With it, blood pressure is in the range of 140/90 mm Hg. up to 159/99 mm Hg.
It has been established that the pathology at this stage is potentially reversible. That is, provided that treatment is started in a timely manner and blood pressure is regularly adjusted, the patient can get rid of the dangerous condition. But timely diagnosis can be difficult because a person does not experience significant changes in well-being and does not seek medical help.
Causes, risk factors
There are many prerequisites for the occurrence of stage 1 arterial hypertension. The determining reason may be one, or more often several, from the list.
8
24/7
- Reaching a certain age. It is generally accepted that the critical milestone for the development of pathologies associated with cardiac disorders and vascular conditions is 50 years. But persistent high blood pressure can accompany a person even earlier - in men the disease develops from the age of 40, in women its signs accompany the onset of menopause.
- Drinking alcohol and smoking. The substances that a person receives through smoking are harmful, their action leads to the destruction of small vessels, capillaries, and a decrease in the elasticity of large arteries. Such processes lead to the fact that blood flow is hampered and blood pressure rises. Alcoholic drinks, when consumed regularly in significant doses, also lead to blood flow disorders.
- Exceeding the norm of cholesterol. Excess of this substance begins to be deposited on the inner walls of the arteries in the form of plaques. When they reach a significant size, the internal lumen of the vessels decreases, and blood moves through them with difficulty.
- Poor nutrition. Fatty foods prepared with preservatives and salt provoke an increase in cholesterol levels and fluid stagnation in tissues and internal organs, causing swelling, which causes increased blood pressure.
- Obesity. Excess weight is acquired for several reasons - high-calorie foods, a minimum of physical activity, the presence of diseases characterized by metabolic disorders. They cause dangerous processes that provoke hypertension - decreased elasticity of blood vessels, increased blood viscosity, a tendency to form blood clots, and disturbances in the functioning of the heart.
- Low physical activity, physical inactivity. Neglecting moderate exercise leads to the fact that metabolic processes important for the quality functioning of the cardiovascular system are disrupted, and a shortage of important elements forms in the blood.
- Stress, lack of rest - these factors negatively affect the heart and overstrain it. There is a rhythm disturbance, the hormone adrenaline is actively produced, which provokes increased contractility of the organ and an increase in blood pressure.
- Diseases of the endocrine system, diabetes.
- Hereditary predisposition. An increase in blood pressure can be provoked by the special structure of the heart, its blood vessels, congenital diseases of organs and systems that the child acquires from his parents.
Classification of the disease
Stage 1 arterial hypertension has 4 risk groups, each of which has characteristic symptoms. The diagnosis that is established for patients must have a direct indication of one of them. Risk groups display:
- the presence of concomitant pathologies;
- exposure to hazardous factors;
- lifestyle features;
- presence of bad habits.
The doctor, when classifying a patient into one of the risk groups, can determine the relative percentage of the likelihood of complications occurring.
There is a classification according to risk groups. It indicates possible complications that are likely to occur within 10 years of illness:
- low or grade 1 arterial hypertension risk 1 - complications are expected in less than 15% of patients;
- moderate, corresponds to arterial hypertension 1 risk 2 - the disease is complicated in 15-20% of cases;
- high, another name is arterial hypertension, stage 1, risk 3 - pathology will be accompanied by complications in 20-30% of people;
- hypertension 1 degree risk 4 - complications occur in 30% (or more) of patients, cardiomyopathy with hypertrophy of the left ventricle of the heart often develops.
As clinical practice shows, arterial hypertension, stage 1, risk 2, is the most common diagnosis confirmed by cardiologists.
8
24/7
Symptoms
Arterial hypertension of the 1st degree is rarely accompanied by characteristic manifestations. The patient may complain of different symptoms:
- the appearance of shortness of breath, difficulty breathing when performing actions associated with increased physical activity;
- swelling of the limbs, face;
- tachycardia;
- regular occurrence of headaches;
- a decrease in the amount of urine excreted from the body, a change in its color.
Diagnostics
The main symptom characteristic of the development of arterial hypertension of the 1st degree is a steady increase in blood pressure values with a rare independent decrease in values. It is this sign that the doctor recommends monitoring - pressure measurements should be taken by the patient regularly. It is necessary to use the tonometer at the same time (several times a day) for 3-4 weeks. The results must be recorded in writing.
To confirm stage 1 arterial hypertension, additional diagnostic procedures are necessary. These include instrumental examinations and laboratory tests.
In a clinical laboratory, a patient gives blood and urine. Their general analysis is carried out. The blood sample is also examined for its biochemical composition. Important indicators are the levels:
- cholesterol;
- hemoglobin;
- Sahara;
- ratio of microelements (potassium, calcium);
- presence of creatinine;
- hematocrit.
The peculiarities of equipping the clinic with diagnostic equipment and the amount of time available to confirm the diagnosis determine the choice of one or more methods for confirming the disease and associated pathologies. For most patients, it is enough to take an electrocardiogram and interpret its results, and conduct a chest x-ray.
To fully assess the patient’s condition, consultations with specialized specialists – an ophthalmologist, an endocrinologist, a neurologist – are required.
Treatment
When treating arterial hypertension of the 1st degree, an integrated approach is required. Blood pressure can be normalized not only with the help of medications or traditional medicine recipes; changing the patient’s usual lifestyle is of great importance. Unconditional implementation of all doctor’s recommendations is the basis for quality therapy:
- weight loss for patients with obesity, regardless of its degree;
- transition to a special diet, the menu includes only low-fat foods, vegetables, fruits, and a minimum amount of salt;
- moderate physical activity is selected individually, taking into account the patient’s health characteristics;
- rejection of bad habits;
- exclusion of stressful situations.
For drug therapy, the patient is prescribed traditional antihypertensive drugs:
- calcium channel blockers;
- beta blockers;
- ACE inhibitors;
- sartans;
- diuretics.
It should be remembered that any self-medication with high blood pressure is dangerous. The drugs used for therapy have many contraindications and have dangerous side effects. Increasing the dosage of a medicine or the wrong combination of drugs can cause significant harm to human health.
Forecast and prevention of the disease
The prognosis for the initial stage of the disease is favorable - timely, competent treatment and prevention guarantee recovery. To prevent the progression of hypertension, it is necessary to prevent its development in time. Preventive actions:
- constant monitoring of blood pressure indicators;
- undergoing diagnostic procedures - blood tests (general and biochemical), ECG;
- physical activity should be moderate but regular;
- nutritional control and weight normalization are necessary.
When the first signs of arterial hypertension of the 1st degree appear, you must immediately contact a medical institution and undergo examination by medical specialists.
8
24/7
The danger of high blood pressure
The main danger of hypertension is its complications, leading to disability and death.
The most severe complications:
- from the heart - heart attack, development of arrhythmia, heart failure;
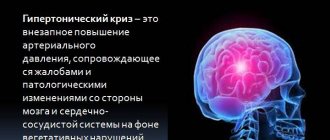
- in the brain - stroke, loss of memory and intellectual abilities (dementia);
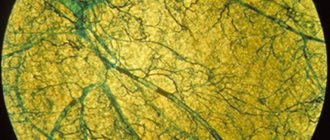
- from the eyes - severe vascular disorders in the retina;
- kidney – the occurrence of failure;
- vessels - aneurysm (sac-like expansion) of the aorta, the rupture of which leads to almost instant death.
What is stage 2 hypertension
Stage 2 hypertension is a condition characterized by a persistent increase in blood pressure to 160/100 and above. However, blood pressure rarely returns to normal on its own; drug treatment is required to correct the patient’s condition.
Stage 2 hypertension is more common in patients over 50 years of age and this is understandable. With age, changes occur associated with the deposition of cholesterol plaques and narrowing of the lumen of blood vessels, the load on the heart increases, which has to make more efforts to pump blood, and conditions arise for increased blood pressure.
Disability
After the patient undergoes a comprehensive examination of the body, the attending physician, if there are sufficient grounds, decides to refer the patient to a medical commission, which includes a board of physicians that has the authority to draw up a conclusion on the person’s incapacity for work due to the presence of a chronic disease. Hypertension of degree 2, risk 3, belongs to a group of similar pathologies and the patient actually has the right to receive the status of a disabled person. What disability group can be obtained for hypertension?
Third disability group.
In most cases, patients are assigned disability group 3, which entitles them to receive social assistance from the state based on the amount of the minimum pension. These are payments intended to ensure that a hypertensive patient has the opportunity to purchase medications that will quickly relieve a hypertensive crisis, or to keep it under constant control by regularly taking medications. Patients with disability group 3 and arterial hypertension of degree 2, risk 3, have the right to work, but the list of types of employment is significantly limited, since there is a high probability that the person will suddenly become ill, feel dizzy, or experience a jump in blood pressure with further loss of consciousness.
Therefore, after receiving the status of a disabled person of group 3, a hypertensive person cannot be allowed to work related to the performance of the following job duties:
- installation of metal connections and work with various objects on high-rise buildings and structures;
- driving vehicles, mechanisms, equipment and installations that belong to the category of increased danger, and loss of control over them can lead to an emergency situation;
- performing welding work using electric and gas equipment;
- mental employment, which involves intense mental activity throughout the working day;
- specialties related to psycho-emotional stress.
Patients with stage 2 hypertension with risk 3, who have received group 3 disabled status, are recommended to lead a measured lifestyle and work in positions that balance mental activity and minor physical activity.
Second disability group.
This disability group can also be assigned to a patient with arterial hypertension of degree 2 with risk 3, but only if the examination results revealed irreversible changes in the tissues of the following organs:
- kidneys;
- heart muscle;
- eyeball;
- brain;
- vessel walls.
In this case, a cause-and-effect relationship must be established, indicating that the disease arose precisely because of the presence of hypertension. There must also be a significant probability that the patient may at any time experience an ischemic cerebral stroke, myocardial infarction, visual impairment, or the development of renal failure. The general practitioner or cardiologist indicates these risk factors in the patient’s medical record and the referral sheet to the medical commission, which establishes the patient’s disability with recommendations for assignment of disabled status. The presence of disability group 2 excludes the opportunity to work and lead an active lifestyle. It is believed that a patient with this group can perform only the most basic actions. The ICD code for hypertension stage 2, risk 3 is 10:11.
Symptoms of stage 2 hypertension
Stage 2 hypertension has ambiguous symptoms and treatment. Increased blood pressure may be accompanied by the following symptoms:
- Throbbing pain in the temporal region;
- Swelling of the face, especially the eyelids;
- The facial skin is hyperemic, and spider veins appear over time;
- Hands swell;
- It gets dark in the eyes, “spots” periodically flicker;
- At the same time, there is aching pain in the back of the head;
- After waking up, there is no cheerfulness, fatigue and apathy persist throughout the day;
- Periodic noise in the head;
- Emotional lability – low threshold of excitability;
- Dilated blood vessels of the eyes (sclera);
- Compaction of the ventricular wall (resistance to blood flow is compensated);
- Involuntary urination due to renal failure;
- Heart rate increases with the slightest exertion;
- There are problems with remembering.
Hypertension of the 2nd degree, symptoms can change depending on its characteristics: a primary independent form or a secondary one, as a complication of another disease.
Causes of arterial hypertension
Experts fail to establish the causes of arterial hypertension in 90% of cases. In 10% of cases, the disease can develop as a complication of another disease or as a result of taking medications. The risk of developing hypertension syndrome may increase due to several factors:
- hereditary predisposition;
- age and gender of the person;
- smoking;
- frequent stressful situations;
- drinking alcohol in large quantities;
- excessive consumption of salt in food;
- low mobility and obesity;
- kidney diseases;
- metabolic disorder;
- diabetes.
Risk 2 for stage 2 arterial hypertension
When establishing the risk of a characteristic illness, doctors take into account the age, gender, and presence of chronic diseases in the body of a clinical patient. This information helps predict clinical outcome and reduce the likelihood of serious health complications and disability. Risk 2 for arterial hypertension of the 2nd degree means that irreversible processes in internal organs under the influence of surges in blood pressure are observed only after 10 years, the probability of stroke and heart attack is 20%.
Arterial hypertension: treatment with modern methods
The choice of treatment for hypertension is made by specialists based on research data. Treatment methods for arterial hypertension are divided into non-pharmacological and medicinal.
Patients diagnosed with mild hypertension, in particular stage 1 arterial hypertension, may be exempted by their doctor from taking special medications. The main method of non-drug treatment is changing the patient’s lifestyle:
- rejection of bad habits;
- weight control;
- regular moderate physical activity. Daily activities such as moderate walking or light strength training are effective;
- reducing stress. During stressful situations, a person’s blood pressure may increase; it can be lowered with the help of massage, breathing exercises or meditation;
- including foods rich in macro- and microelements in the diet and reducing salt intake.
Medicines for arterial hypertension are prescribed to patients when non-drug therapy has proven ineffective within 3-4 months, and there are risk factors. Thus, arterial hypertension 2 risk 3 requires taking special medications. The number of drugs is determined by blood pressure and the presence of concomitant diseases.
Modern doctors prescribe drugs for the treatment of arterial hypertension in accordance with one of the strategies: monotherapy or combination therapy. When drawing up a treatment plan, the question of the admissibility of using one drug is the most pressing for the specialist.
In monotherapy, a patient with grade I is prescribed one drug at the beginning of the course of treatment. An important factor when prescribing a drug is its effectiveness in reducing the risk of complications. Currently, to control blood pressure, doctors use the most studied drugs belonging to two groups: thiazide-like and thiazide diuretics, which have a diuretic effect.
Combination therapy is prescribed to patients with a high degree of risk, as well as with stages II and III of the disease. With this method of treatment, drugs with different mechanisms of action are selected to lower blood pressure and reduce possible side effects.
Experts on the question of how, if a patient has arterial hypertension, how to treat this disease with drugs, prefer to use several groups of drugs:
- beta blockers. For several decades, beta blockers have been used as the mainstay of treatment for hypertension in children and adolescents. However, multiple side effects have now been identified, and therefore their use has become limited. Experts include the main side effects: sleep disturbances, increased blood glucose levels, weakness and mood swings. An important condition when using these funds is an electrocardiogram and regular monitoring of blood sugar;
- Diuretics are prescribed to patients for a long period; they remove excess fluid from the body. Side effects include: fainting, decreased calcium levels in the blood;
- calcium channel blockers. Drugs in this group are used quite widely to treat patients; doctors give preference to drugs with a long period of action. Side effects of blockers include: gastrointestinal disorders, rapid heartbeat, weakness, dizziness and swelling;
- ACE inhibitors. The mechanism of action of these drugs is to block the action of enzymes that are involved in the formation of a vasoconstrictor;
- alpha adenoblockers. The effect of drugs in this group is manifested in a decrease in pressure through blocking receptors located in the artery wall.
Arterial hypertension 2 degrees risk 4
Risks of arterial hypertension 2 degrees The presence of a “bouquet” of diseases (atherosclerosis, diabetes, ischemia) allows us to state that the patient has acquired a diagnosis of hypertension 2 degrees, 4 risk. Arterial hypertension at this stage only complicates the situation. This diagnosis is given to patients who have survived 1-2 heart attacks, regardless of the affected area.
It should be clarified that one hundred risk is a predictable concept, not an absolute one. It only indicates the likelihood of a complication developing. If the patient understands the danger of his situation and takes appropriate measures, the diagnosis can be corrected. Hypertensive patients who adhere to a healthy lifestyle and constantly monitor their condition can live a long and fulfilling life.
While with a burdened anamnesis and high risk, life expectancy is significantly shorter. Timely diagnosis and adequate treatment aimed at reducing blood pressure can extend your life and improve your quality of life.
Consequences of hypertension
The higher your blood pressure, the harder the work your heart has to do to maintain normal blood circulation. Therefore, if hypertension is not treated, the walls of the heart first thicken or hypertrophy, which increases the risk of the heart working intermittently, and later the walls of the heart become thinner, which leads to disruption of the blood supply to the tissues and the heart itself and is accompanied by the appearance of shortness of breath, fatigue, and swelling in the legs. These signs often indicate the development of heart failure, which is the inability of the heart muscle to perform its normal pumping function.
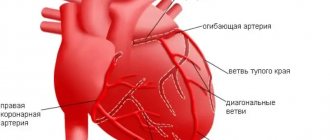
High blood pressure accelerates a process known as atherosclerosis, which is the formation of fatty deposits on the walls of the arteries, causing them to harden, thicken, and reduce the lumen of the vessels. If the coronary arteries that supply blood to the heart are affected, angina pectoris or angina pectoris develops. As the process progresses, one of the arteries may become completely blocked, then part of the heart muscle stops receiving blood, and myocardial infarction develops. Atherosclerosis can affect any part of the arterial bed. If cerebral vessels are damaged, a patient with hypertension is highly likely to develop a cerebral stroke, which impairs motor abilities, speech and memory. When the blood vessels of the eyes, kidneys and lower extremities are affected, there is a high risk of developing blindness, renal failure and “intermittent claudication”.
Treatment of stage 2 hypertension
How to treat stage 2 hypertension? The scheme is drawn up by the local therapist. If necessary, a consultation with a cardiologist and neurologist is scheduled. Traditional methods of treating stage 2 hypertension include:
- To eliminate blood thickness (thin the blood flow), you should take Aspirin, Cardiomagnyl, Heparin, Aspicard.
- To normalize blood pressure, diuretics (diuretics) are prescribed, such as Diuver, Furosemide, Piretanide, Torasemide, Veroshpiron, Ravel.
- For this diagnosis, thiazides (thiazide drugs) such as Arifon, Chlorthalidone, Indapamide are recommended.
- To reduce blood cholesterol, you should take lipid-lowering drugs such as Atorvastatin, Atoris, Liprimar, Zovasticor.
- In order to dilate blood vessels, antihypertensive drugs of different groups are prescribed, such as Physiotens, Artil, Bisoprolol, Lisinopril.
It is important to consider that the quality of treatment largely depends on compliance with the instructions for their use. Self-medication for hypertension is dangerous. Such experiments can result in disability. The therapist selects the treatment regimen individually, taking into account the age, build and other health characteristics of the individual patient.
Diet for hypertension
In order for the kidney vessels to function normally, hypertensive patients with any stage of the disease must adhere to certain nutritional rules. For example, it is important to control the water and salt balance of the body, to prevent the formation of stagnation and, as a consequence, stage 2 hypertensive crisis. Fatty, fried, sweet and smoked foods are prohibited.
Seven foods that lower blood pressure:
- Blueberries – Blueberries are rich in natural substances called flavonoids.
- Fresh leafy greens such as fenugreek leaves, kale, mint leaves, patchouli, dill greens, mustard leaves, curry leaves, beet greens, Swiss chard, arugula, broccoli, celery and spinach are high in potassium
- Potatoes - contain a lot of potassium and magnesium
- Beets – Nitrates in beet juice are known to lower blood pressure
- Skim milk is an excellent source of calcium plus low fat levels
- Oatmeal is a high-fiber, low-fat, low-sodium food.
- Bananas – Adds potassium to your diet.
Therapeutic nutrition for stage 2 hypertension allows boiled lean meats, cereals, vegetables and fruits on the menu. Green tea and diuretic herbal decoctions have beneficial properties.
Folk remedies
When treating illness at home, many people prefer to use folk remedies. This therapy involves the use of medicinal plants that have a positive effect on the cardiovascular system.
You can treat the disease with the following recipes:
- Treatment can also be carried out with peppermint, cinquefoil, chamomile, and yarrow. These herbs go well together.
- Prepare a decoction of motherwort, horsetail, marsh cudweed, and valerian root. All plants must be taken in the same quantity. This remedy has diuretic effects and allows you to cope with single surges in blood pressure.
- Bee products and citrus fruits are actively used in the treatment of hypertension.
- You can treat with viburnum juice. To reduce blood pressure, it should be consumed three times a day, a quarter glass.
Folk remedies help cope with unpleasant symptoms of the disease and speed up the effectiveness of traditional therapy. Such recipes have proven their benefits over many centuries. People whose bodies do not tolerate medications well turn to this type of therapy. But it is important to remember that treatment of the disease with traditional recipes can only be carried out after consultation with a doctor.
Prevention
Your healthcare provider will likely also suggest a variety of lifestyle changes, including:
- Maintaining a healthy weight;
- A diet rich in fruits, vegetables and low-fat dairy products;
- To give up smoking;
- Limiting salt intake in the diet;
- Limit alcohol consumption. For most adults, this means that it is normal to drink up to one drink per day for women of all ages and men over the age of 65, and up to two drinks per day for men 65 or younger;
- Exercise at least 30 minutes a day. These include walking, jogging, strength training, yoga, and cardio exercises such as cycling.
On your part, methodical adherence to medical recommendations and organization of the correct regimen are required. A healthy lifestyle is the path to recovery. Remember this.