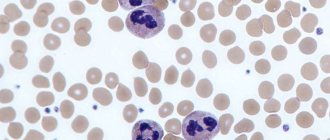
Neutrophils are the largest group of granulocytes, the main function of which is phagocytosis (destruction) of pathogenic flora in the human body.
Neutropenia is a decrease in the number of neutrophils in the blood, which leads to the risk of bacterial and fungal infections.
In a healthy state, protection of the immune “borders” is provided by mature segmented neutrophils. Younger band neutrophils also help to “control” the situation, but there are much fewer of them (this is clearly visible from the results of a blood test, where normally mature neutrophils number from 42-72%, and young ones only from 1-6%).
But, in the event of certain diseases, the ratio of all types of neutrophils (segmented, band, myelocytes, metamyelocytes) is sharply disrupted, which leads to a pathological increase in neutrophils or their decrease (neutropenia).
At the same time, the number of neutrophils in human blood is not stable, unlike other cell groups of the leukocyte formula. The maturation, development and normal ratio of these granulocytes are affected not only by congenital and acquired pathologies, but also by severe emotional shock, stress, dietary disturbances, etc.
Neutropenia in children should be carefully investigated to prevent both severe pathologies and radical treatment without serious reasons.
Classification of severity of neutropenia:
- Light (1-1.5 x 109/l);
- Moderate (0.5-1 x109/l);
- Heavy (less than 0.5 x109/l).
If the level of neutrophils decreases critically, this leads to the development of infection in the intestines, mouth, thereby causing digestive system disorders, gingivitis, stomatitis, fungal skin lesions, etc.
Severe neutropenia in the presence of cancer pathology has an extremely adverse effect on the functioning of the immune system, leading to progressive inflammation and infections, including death.
Etiology
Neutrophils develop in the bone marrow within 15 days, remain in the bloodstream for about 8 hours, constitute the overwhelming cellular part of the leukocyte formula, and when “pests” are detected, they are immediately sent to eliminate them.
The main causes of neutropenia that disrupt this physiological process:
- Development of pathogenic flora in the body (bacteria, viruses, fungi).
- Exposure to radiation, chemotherapy.
- Pathologies in the functioning of the bone marrow.
- Folic acid deficiency.
- Congenital pathologies of internal organs, glands and systems.
Neutropenia in children can also develop due to disruption of the pancreas and retarded mental development (Shwachman-Diamond-Oski syndrome).
Neutropenia is divided into:
- Spicy;
- Chronic.
Acute neutropenia develops rapidly due to the rapid consumption/destruction of neutrophils, chronic - due to a decrease in the production of granulocytes or excessive splenic secretion.
- Primary;
- Secondary.
Primary neutropenia is associated with internal disorders (congenital pathologies, idiopathic neutropenia, cyclic neutropenia, benign ethnic), secondary - due to the influence of external factors on the maturation and development of bone marrow cells.
Why does this state matter to us?
Leukocytes are responsible for immunity and resistance to various unfavorable factors, therefore, when their level in the blood decreases, the body’s “defense” is primarily affected.
In this case, a person becomes more vulnerable to any infection: bacterial, viral or fungal.
In most cases, with the development of infectious complications, specialized antitumor treatment should be postponed. Consequently, in addition to the main danger for humans, which lies precisely in the infectious process, we are also faced with the fact that we have to postpone the treatment of cancer indefinitely until we deal with the infection.
Secondary neutropenia
Secondary neutropenia most often develops due to:
- Taking certain medications (antibiotics, antihistamines, antipyretics, barbiturates, analgesics);
- Development of infections;
- Immune reactions;
- Bone marrow infiltration.
Secondary neutropenia provokes pathologies:
- Liver, spleen, kidneys;
- Pancreas, thyroid gland;
- Aplastic anemia;
- Megaloblastic anemia;
- Myelodysplastic disorders;
- Myelofibrosis, leukemia;
- Sepsis, HIV, Felty's syndrome;
- Rh-conflicting neutropenia;
- Lymphoproliferative diseases, etc.
In the case of secondary neutropenia, it is not the blood “test” that needs to be treated, but the patient with specific symptomatic manifestations.
Primary and secondary neutropenia should be distinguished, since in the first case, a decrease in the level of neutrophils is the only manifestation, while secondary ones develop on the basis of infections, systemic autoimmune pathologies and onco-neoplasia.
Prevention
- The essence of preventing agranulocytosis is to provide patients at risk of developing this condition with careful and regular hematological monitoring. This is necessary, first of all, during the period of use of myelotoxic drugs.
- It is important to exclude the use of those medications that have previously provoked manifestations of immune agranulocytosis .
- It is also important to practice general preventive measures: strengthen the body's defenses, practice physical activity, healthy eating.
- All infectious diseases should be treated promptly and under the supervision of a physician.
Clinical manifestations
In most cases, neutropenia occurs without any symptoms. Symptoms of a decrease in neutrophils usually occur only if secondary neutropenia has developed against the background of certain pathologies.
General symptoms of neutropenia:
- Increased body temperature;
- Recurrent stomatitis, gingivitis, glossitis;
- Marked weakness;
- Increased sweating;
- Chills;
- Difficulty urinating (burning);
- Cough (against the background of pneumonia, inflammation in the lungs);
- Fungal skin lesions.
As a result of a sharp decrease in granulocytes, febrile neutropenia may also develop. This is a febrile state aggravated by tachycardia, tremor, chills, increased blood pressure, up to the development of cardiovascular collapse.
Febrile neutropenia usually develops as a result of oncopathologies, exposure to radiation or chemotherapy, in the form of a hyperergic reaction of the body to toxic influences (cytostatics, decay of healthy and cancer cells).
It can also manifest itself against the background of a severe infectious process, which is provoked by staphylococci, streptococci, clostridia, and, less commonly, fungi and viruses. In more rare cases, febrile neutropenia may develop from primary autoimmune neutropenia.
Pathogenesis
The pathogenesis of different forms of agranulocytosis is different, and for many it has not yet been studied well enough. In autoimmune forms of the disease, the death of granulocytes occurs due to the influence of autoantibodies. In hapten agranulocytosis, the mechanism of the individual reaction of the body has not been fully studied. When haptens are administered after the first occurrence of hapten agranulocytosis, this condition will recur again.
Neutrophils
Granulocytes (neutrophils) provide protection to the body from attacks by bacteria and fungal infections. With the development of neutropenia, the response to such infections is ineffective.
The limit of the lower norm of neutrophils is 1500/μl in representatives of the Caucasian race; in people of the Negroid race this figure is slightly lower - about 1200/μl. The number of these cells is unstable - depending on the influence of various factors, it can change over a short period of time.
When the number of neutrophils decreases to <500/μl, an infectious process can develop due to the influence of endogenous microflora (in the intestines, in the mouth). If the number of these cells is reduced to <200/μl, the inflammatory response may be suppressed and typical signs of such a process (leukocytes in the urine, in the area of infection, leukocytosis) may not be observed.
In acute neutropenia , especially when combined with other factors (oncological disease, etc.), the function of the immune system is significantly impaired, which can subsequently lead to fulminant fatal infections. The risk of developing infectious processes is also affected by the integrity of the skin, mucous membranes, blood supply and tissue nutrition. People with severe neutropenia most often develop the following infectious diseases: pneumonia , furunculosis , septicemia .
The presence of places where vascular catheters were placed and injections were performed additionally increases the risk of developing skin infections. The most common pathogens are Staphylococcus aureus, coagulase-negative staphylococci, but other bacteria can also provoke the pathological process. People with agranulocytosis often develop other diseases: colitis , paraproctitis , stomatitis , otitis , sinusitis , etc. Those patients who have prolonged neutropenia after chemotherapy , stem cell transplantation, high doses of corticosteroid drugs are prone to developing fungal infections.
Diagnostics
Diagnosis can be planned, unscheduled (in the presence of specific symptoms), and can also be carried out if the attending physician has any suspicions (unusual or frequently recurring infections).
A routine blood test in children under 1 year of age is carried out once every 3 months, after a year - once every 6 months (including adults).
If the diagnosis indicates a decrease in neutrophils in the blood, the following should be additionally prescribed:
- Screening study for neutropenia;
- Differentiation of neutropenia from other pathologies;
- Clarification of the form of neutropenia;
- Study of the mechanisms of development of this condition in a patient.
Next, the dynamics of the leukocyte formula indicators is assessed (after previous infections, between them, after recovery), including ESR (erythrocyte sedimentation rate), color index, etc.
Determining the cause of neutropenia may include the following diagnostic procedures:
- Visual inspection.
- Physical examination (assessment of the condition of all mucous membranes).
- X-ray.
- CT, ECG, ultrasound, MRI.
- Laboratory tests of blood (general analysis, biochemical), urine.
- Cultural seeding (to determine the type of bacteria and fungi).
- Biopsy.
- Bone marrow studies (to determine the cause of specific neutropenia, for leukemia, aplastic anemia, myelofibrosis).
In the case of severe acute neutropenia, a comprehensive diagnosis should be performed as quickly as possible.
If congenital pathology is considered, diagnosis includes molecular genetic testing of neutropenia.
A single blood test, which showed a low level of granulocytes, cannot make a definitive diagnosis. Since these are the only blood cells whose concentration can change daily, due to their short “life” in the bloodstream (6-8 hours).
To accurately confirm the patient’s condition, the blood test must be repeated at a short time interval (the time for testing is set by the doctor).
General information
Neutropenia or agranulocytosis is a condition characterized by a decrease in the number of neutrophil granulocytes in the blood. With severe neutropenia in a person, the likelihood of developing fungal and bacterial infections, as well as the severity of their course, increases. With agranulocytosis, the level of leukocytes decreases to less than 1•10 per 9/L due to a decrease in the number of granulocytes (less than 0.75•10 per 9/L) and monocytes .
There are several forms of the disease depending on the pathogenesis. Speaking about neutropenia - what it is, it should be noted that this condition was first described in 1922. Currently, due to the active use of cytostatic treatment and various medications, the frequency of manifestation of this syndrome has increased.
To diagnose this condition, it is necessary to determine the number of leukocytes in the blood and the leukocyte formula. However, during the diagnostic process, it is very important to find out the cause of this manifestation in order to provide adequate treatment.
Why this condition can occur, and what treatment methods are used depending on the cause of neutropenia, will be discussed in this article.
Treatment
Intermittent neutropenia usually occurs without symptoms or severe infectious complications, and therefore does not require therapeutic treatment. Especially if the patient carefully observes the rules of personal hygiene, eats foods that have been heat-treated (raw fish dishes, meat with blood are not allowed in case of neutropenia), uses gloves when cleaning, and protects the skin from prolonged exposure to the sun.
With secondary neutropenia, treatment is aimed primarily at eliminating the underlying disease, which led to a pathological decrease in granulocytes.
At the Spizhenko Clinic, treatment of neutropenia is carried out taking into account the cause and clinical symptoms and may include:
- Antibacterial therapy.
- Antifungal therapy.
- Immunotherapy.
- Use of glucocorticoids.
Including treatment of associated conditions (ulcers, stomatitis, gingivitis) by rinsing the mouth with saline solution, using antiseptics (chlorhexidine), nystatin, clotrimazole, fluconazole (for candidiasis).
In case of acute lesions of the mucous membranes, an additional diet (with a predominance of liquid food in the diet) and local anesthesia are prescribed. If the decrease in neutrophils occurred as a result of taking medications, the way out of the situation is to stop using them and switch to alternative treatment.
Medicines
that lead to neutropenia:
- Anticonvulsants (Diazepam, Phenytoin, Sodium Valproate).
- Antidepressants (Clozapine, Haloperidol).
- Antibiotics (Doxycycline, Lincomycin, Cephalosporin, Penicillin, Vancomycin).
- Antiviral (Acyclovir, Zidovudine).
- Anthelmintics (Levomizole, Mebenzadol).
- Antituberculosis (Streptomycin, Rifampicin, Isoniazid, Ethambutol).
- Antifungals (Griseofulvin, Mycozolon, Amorolfine).
Including analgesics (Ibuprofen, Indomethacin, Amidopyrine, Acetylsalicylic acid, Phenylbutazone).
Treatment of febrile neutropenia
Febrile neutropenia requires immediate medical intervention (within 1 hour!).
For neutropenic fever the following is prescribed:
- Antimicrobial therapy;
- Emergency diagnostics (culture of blood, urine, secretions from the mouth, catheterization sites, vagina/urethra, ultrasound of internal organs, radiography).
The basis of modern antibacterial treatment for FN (febrile neutropenia) is beta-lactam antibiotics.
At the Spizhenko Clinic you can undergo a comprehensive study of neutropenia, determine the exact cause and receive the most correct treatment (if necessary).
Neutropenia is not a “sentence”, but also not a reason to leave this situation without competent medical attention.
How to prevent infection
Below are some ways to prevent infection:
- Do not accept guests who have a cold or who have recently had an infection.
- Wear a mask when visiting public places, using public transport or being in crowded places. It will help protect you from a cold or respiratory infection.
- Do not treat your teeth unless absolutely necessary. Consult your healthcare provider before undergoing any procedure.
- Ask your healthcare provider when you can again: use tampons;
- use dental floss;
- use suppositories (solid soluble medications);
- give enemas;
- have sex.
to come back to the beginning
Is it possible to increase the level of leukocytes and neutrophils?
Chemotherapy drugs are toxic substances. There are indications and contraindications for their use, because they can both help the patient and cause great harm if used thoughtlessly. The only appropriate and reasonable method to increase the level of white blood cells and neutrophils is to wait.
Yes this is true.
Firstly, because each organism has its own characteristics and is not always able to recover by the time specified by the recommendations.
The intervals between cycles are optimal, but a deviation from the timing by 1-2 weeks (sometimes more, if necessary) is acceptable if there are contraindications to chemotherapy.
Secondly, any drugs that stimulate an increase in the level of leukocytes and neutrophils are dangerous because after several such stimulations, the bone marrow reserve can be depleted, and after this, recovery will take much longer and will be associated with possible complications.
If leuko- and neutropenia is constant, and the body does not recover properly even with increasing intervals between cycles, then specialized drugs are prescribed, which should be used only under the supervision of a doctor in strictly indicated situations.
Any so-called immunomodulators, immune stimulants will not bring any benefit, there will be no effect from them, because leukocytes will still decrease during chemotherapy, as it should be, but at the same time such drugs can provoke the development of undesirable reactions.