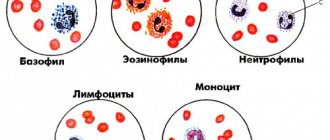
Neutrophils are the largest group of granulocytes, the main function of which is phagocytosis (destruction) of pathogenic flora in the human body.
Neutropenia is a decrease in the number of neutrophils in the blood, which leads to the risk of bacterial and fungal infections.
In a healthy state, protection of the immune “borders” is provided by mature segmented neutrophils. Younger band neutrophils also help to “control” the situation, but there are much fewer of them (this is clearly visible from the results of a blood test, where normally mature neutrophils number from 42-72%, and young ones only from 1-6%).
But, in the event of certain diseases, the ratio of all types of neutrophils (segmented, band, myelocytes, metamyelocytes) is sharply disrupted, which leads to a pathological increase in neutrophils or their decrease (neutropenia).
At the same time, the number of neutrophils in human blood is not stable, unlike other cell groups of the leukocyte formula. The maturation, development and normal ratio of these granulocytes are affected not only by congenital and acquired pathologies, but also by severe emotional shock, stress, dietary disturbances, etc.
Neutropenia in children should be carefully investigated to prevent both severe pathologies and radical treatment without serious reasons.
Classification of severity of neutropenia:
- Light (1-1.5 x 109/l);
- Moderate (0.5-1 x109/l);
- Heavy (less than 0.5 x109/l).
If the level of neutrophils decreases critically, this leads to the development of infection in the intestines, mouth, thereby causing digestive system disorders, gingivitis, stomatitis, fungal skin lesions, etc.
Severe neutropenia in the presence of cancer pathology has an extremely adverse effect on the functioning of the immune system, leading to progressive inflammation and infections, including death.
Etiology
Neutrophils develop in the bone marrow within 15 days, remain in the bloodstream for about 8 hours, constitute the overwhelming cellular part of the leukocyte formula, and when “pests” are detected, they are immediately sent to eliminate them.
The main causes of neutropenia that disrupt this physiological process:
- Development of pathogenic flora in the body (bacteria, viruses, fungi).
- Exposure to radiation, chemotherapy.
- Pathologies in the functioning of the bone marrow.
- Folic acid deficiency.
- Congenital pathologies of internal organs, glands and systems.
Neutropenia in children can also develop due to disruption of the pancreas and retarded mental development (Shwachman-Diamond-Oski syndrome).
Neutropenia is divided into:
- Spicy;
- Chronic.
Acute neutropenia develops rapidly due to the rapid consumption/destruction of neutrophils, chronic - due to a decrease in the production of granulocytes or excessive splenic secretion.
- Primary;
- Secondary.
Primary neutropenia is associated with internal disorders (congenital pathologies, idiopathic neutropenia, cyclic neutropenia, benign ethnic), secondary - due to the influence of external factors on the maturation and development of bone marrow cells.
Secondary neutropenia
Secondary neutropenia most often develops due to:
- Taking certain medications (antibiotics, antihistamines, antipyretics, barbiturates, analgesics);
- Development of infections;
- Immune reactions;
- Bone marrow infiltration.
Secondary neutropenia provokes pathologies:
- Liver, spleen, kidneys;
- Pancreas, thyroid gland;
- Aplastic anemia;
- Megaloblastic anemia;
- Myelodysplastic disorders;
- Myelofibrosis, leukemia;
- Sepsis, HIV, Felty's syndrome;
- Rh-conflicting neutropenia;
- Lymphoproliferative diseases, etc.
In the case of secondary neutropenia, it is not the blood “test” that needs to be treated, but the patient with specific symptomatic manifestations.
Primary and secondary neutropenia should be distinguished, since in the first case, a decrease in the level of neutrophils is the only manifestation, while secondary ones develop on the basis of infections, systemic autoimmune pathologies and onco-neoplasia.
Clinical manifestations
In most cases, neutropenia occurs without any symptoms. Symptoms of a decrease in neutrophils usually occur only if secondary neutropenia has developed against the background of certain pathologies.
General symptoms of neutropenia:
- Increased body temperature;
- Recurrent stomatitis, gingivitis, glossitis;
- Marked weakness;
- Increased sweating;
- Chills;
- Difficulty urinating (burning);
- Cough (against the background of pneumonia, inflammation in the lungs);
- Fungal skin lesions.
As a result of a sharp decrease in granulocytes, febrile neutropenia may also develop. This is a febrile state aggravated by tachycardia, tremor, chills, increased blood pressure, up to the development of cardiovascular collapse.
Febrile neutropenia usually develops as a result of oncopathologies, exposure to radiation or chemotherapy, in the form of a hyperergic reaction of the body to toxic influences (cytostatics, decay of healthy and cancer cells).
It can also manifest itself against the background of a severe infectious process, which is provoked by staphylococci, streptococci, clostridia, and, less commonly, fungi and viruses. In more rare cases, febrile neutropenia may develop from primary autoimmune neutropenia.
Main symptoms of neutropenia
The rate at which neutropenia occurs depends on the severity of the infection, as well as the degree to which the level of these blood cells decreases.
Usually, patients first develop stomatitis, tonsillitis, and pharyngitis. Due to the lack of movement of leukocytes, the inflammation is fibrous-necrotic in nature. A gray coating forms on the mucous membranes, which indicates the development of a bacterial process. Infectious agents enter the general bloodstream and rapidly spread throughout the body. The patient develops headache, apathy, nausea, and body temperature can reach 40 degrees. Also characteristic symptoms of neutropenia include:
- Rapid formation of ulcers
. Initially they spread through the mucous membranes of the cheeks. In the future, this can lead to gangrene of facial tissues. Then the gastrointestinal tract is affected: necrosis of the mucous membrane of the stomach, intestines, and esophagus occurs; - Due to damage to the gastrointestinal tract, severe pain and bloating
. Deep disorders are manifested by hemorrhages. The risk of developing jaundice increases; - Pneumonia
. With neutropenia, it occurs atypically and, if untreated, spreads to neighboring organs. Tears and gangrene form on the lungs. Inflammation can be determined by a severe cough, shortness of breath, chest pain when breathing; - Damage to the genitourinary system
. The infection affects the bladder, urethra, or uterus. In this case, the patient experiences pain in the lower abdomen and sharp pain when urinating. Women are characterized by the appearance of whitish vaginal discharge; - Disturbances in the functioning of the heart
. Due to general intoxication of the body, venous and arterial hypotension develops. When listening to the heart, functional murmurs are present; - Kidney damage
. Against the background of the activity of infectious agents, the body removes protein. Blood and epithelial cells of the renal tubules are also found in the urine; - Development of septic complications
. Pathogenic agents rapidly spread throughout the body and cause numerous disorders. Due to saprophytic flora, blood poisoning can occur. In this case, the disease is very difficult, the body temperature rises to 41-42 degrees. Black rashes appear all over the body.
Neutropenia is a serious illness that, if safety measures are not followed, leads to serious complications and even death. If all the doctor’s recommendations are followed, the patient will be able to protect himself from such consequences. Mild neutropenia is determined only by the results of a general blood test. Maintenance medications are prescribed to prevent more serious symptoms from worsening.
Each patient with this pathology should be as attentive to their health as possible. Especially if he is in a high-risk group. You should definitely consult a doctor if these symptoms appear:
- Body temperature increased to 38 degrees;
- Chills or profuse sweating;
- Redness, pain, swelling with minor damage to the skin;
- Shortness of breath, cough;
- Itching, discharge from the genitals;
- Painful and frequent urination;
- Increasing abdominal pain;
- Sore throat, oral cavity.
Diagnostics
Diagnosis can be planned, unscheduled (in the presence of specific symptoms), and can also be carried out if the attending physician has any suspicions (unusual or frequently recurring infections).
A routine blood test in children under 1 year of age is carried out once every 3 months, after a year - once every 6 months (including adults).
If the diagnosis indicates a decrease in neutrophils in the blood, the following should be additionally prescribed:
- Screening study for neutropenia;
- Differentiation of neutropenia from other pathologies;
- Clarification of the form of neutropenia;
- Study of the mechanisms of development of this condition in a patient.
Next, the dynamics of the leukocyte formula indicators is assessed (after previous infections, between them, after recovery), including ESR (erythrocyte sedimentation rate), color index, etc.
Determining the cause of neutropenia may include the following diagnostic procedures:
- Visual inspection.
- Physical examination (assessment of the condition of all mucous membranes).
- X-ray.
- CT, ECG, ultrasound, MRI.
- Laboratory tests of blood (general analysis, biochemical), urine.
- Cultural seeding (to determine the type of bacteria and fungi).
- Biopsy.
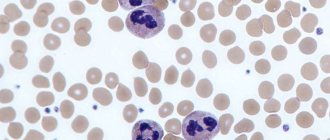
- Bone marrow studies (to determine the cause of specific neutropenia, for leukemia, aplastic anemia, myelofibrosis).
In the case of severe acute neutropenia, a comprehensive diagnosis should be performed as quickly as possible.
If congenital pathology is considered, diagnosis includes molecular genetic testing of neutropenia.
A single blood test, which showed a low level of granulocytes, cannot make a definitive diagnosis. Since these are the only blood cells whose concentration can change daily, due to their short “life” in the bloodstream (6-8 hours).
To accurately confirm the patient’s condition, the blood test must be repeated at a short time interval (the time for testing is set by the doctor).
Diagnostic methods
Neutropenia often develops in patients who are susceptible to infections. People who have undergone radiation or chemical therapy are at increased risk. Neutropenia can be detected by a general blood test. Based on the results, the doctor will be able to determine the infectious process in the body. Additionally, diagnostics includes the following studies:
- Bacterial blood culture – identifies pathological agents;
- General urinalysis – determines kidney function;
- Myelograms – studies of bone marrow composition;
- X-ray of the lungs – diagnoses pneumonia.
Treatment
Intermittent neutropenia usually occurs without symptoms or severe infectious complications, and therefore does not require therapeutic treatment. Especially if the patient carefully observes the rules of personal hygiene, eats foods that have been heat-treated (raw fish dishes, meat with blood are not allowed in case of neutropenia), uses gloves when cleaning, and protects the skin from prolonged exposure to the sun.
With secondary neutropenia, treatment is aimed primarily at eliminating the underlying disease, which led to a pathological decrease in granulocytes.
At the Spizhenko Clinic, treatment of neutropenia is carried out taking into account the cause and clinical symptoms and may include:
- Antibacterial therapy.
- Antifungal therapy.
- Immunotherapy.
- Use of glucocorticoids.
Including treatment of associated conditions (ulcers, stomatitis, gingivitis) by rinsing the mouth with saline solution, using antiseptics (chlorhexidine), nystatin, clotrimazole, fluconazole (for candidiasis).
In case of acute lesions of the mucous membranes, an additional diet (with a predominance of liquid food in the diet) and local anesthesia are prescribed. If the decrease in neutrophils occurred as a result of taking medications, the way out of the situation is to stop using them and switch to alternative treatment.
Medicines
that lead to neutropenia:
- Anticonvulsants (Diazepam, Phenytoin, Sodium Valproate).
- Antidepressants (Clozapine, Haloperidol).
- Antibiotics (Doxycycline, Lincomycin, Cephalosporin, Penicillin, Vancomycin).
- Antiviral (Acyclovir, Zidovudine).
- Anthelmintics (Levomizole, Mebenzadol).
- Antituberculosis (Streptomycin, Rifampicin, Isoniazid, Ethambutol).
- Antifungals (Griseofulvin, Mycozolon, Amorolfine).
Including analgesics (Ibuprofen, Indomethacin, Amidopyrine, Acetylsalicylic acid, Phenylbutazone).
Treatment of febrile neutropenia
Febrile neutropenia requires immediate medical intervention (within 1 hour!).
For neutropenic fever the following is prescribed:
- Antimicrobial therapy;
- Emergency diagnostics (culture of blood, urine, secretions from the mouth, catheterization sites, vagina/urethra, ultrasound of internal organs, radiography).
The basis of modern antibacterial treatment for FN (febrile neutropenia) is beta-lactam antibiotics.
At the Spizhenko Clinic you can undergo a comprehensive study of neutropenia, determine the exact cause and receive the most correct treatment (if necessary).
Neutropenia is not a “sentence”, but also not a reason to leave this situation without competent medical attention.
Infectious complications, leukopenia and neutropenia
Infectious complications, leukopenia and neutropenia
Infections are caused by the growth of various microorganisms, such as bacteria, viruses or fungi, inside the human body.
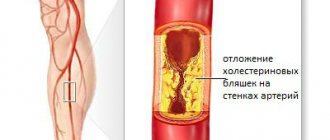
Infections can begin in any organ, but most often they occur in those parts of the body that are in close contact with the external environment, for example in the skin, mucous membranes of the digestive tract (oral cavity, esophagus, intestines), respiratory tract (larynx, trachea, bronchi, lungs) and organs of the genitourinary system. Normally, the body is protected from most pathogens of infectious diseases by the immune system, which can effectively destroy microorganisms. However, during the period of antitumor therapy, the functioning of the immune system may be disrupted - treatment methods such as radiation therapy, chemotherapy, as well as some “targeted” drugs can damage the bone marrow, in which the cells necessary for the functioning of the immune system - leukocytes - are formed. There are many forms of leukocytes, the most important of which are neutrophils - cells that play a major role in the body’s resistance when it “collides” with pathogens of bacterial infections. Poor diet, lack of sleep and stress also weaken the immune system.
The severity of suppression of the immune system function reflects the number of neutrophils in the blood. Normally, their number exceeds 2.0 * 10^9 cells per 1 liter of blood (you can also find the designation 2000 cells per 1 μl). A decrease in their number is designated by the term “neutropenia”. Depending on the severity of neutropenia, the following degrees of severity are distinguished:
- 1st degree – neutrophil count <2000 cells/μl, but more than 1500 cells/μl (<2.0*10^9/l, but ≥ 1.5*10^9);
- Grade 2 – neutrophil count <1500 cells/µl, but more than 1000 cells/µl (<1.5*10^9/l, but ≥ 1.0*10^9). With most drug regimens, a decrease in the number of neutrophils to this level is an indication for delaying the next course of treatment;
- grade 3 – neutrophil count <1000 cells/µl, but more than 500 cells/µl (<1.0*10^9/l, but ≥ 0.5*10^9);
- 4th degree – number of neutrophils <500 cells/μl, (<0.5*10^9/l);
With the development of “deep” neutropenia - degrees 3-4, you should especially carefully monitor your health and regularly measure your body temperature.
“Febrile” neutropenia – the number of neutrophils <1000/μl (<1.0*10^9/l) in combination with an increase in temperature >38.3 oC or with an increase in temperature ≥38.0, provided it persists for 1 hour and longer.
Typical symptoms of infection include: fever (temperature increased to 38 oC or higher), cough or sore throat, diarrhea, ear or sinus pain, skin rash, pain when urinating or change in urine color, genital discharge paths, etc. Be sure to consult your doctor if any of the above symptoms occur.
It is worth considering that taking certain medications, such as non-steroidal anti-inflammatory drugs such as paracetamol, aspirin, ibuprofen, as well as glucocorticosteroids (dexamethasone, methylprednisolone, prednisolone, etc.) can reduce body temperature and mask other symptoms of infection. This can lead to serious consequences; be sure to tell your doctor if you have taken or are constantly taking these or other drugs with a similar mechanism of action.
To diagnose neutropenia, a general (clinical) blood test is used; blood for analysis is taken from a finger or from a vein. If the development of an infection is suspected, depending on its clinical picture, additional examination methods are carried out, for example, urine analysis, stool analysis, chest x-ray, abdominal ultrasound, etc.
Infectious complications and “febrile” neutropenia in cancer patients are dangerous and potentially life-threatening complications. Patients receiving antitumor treatment are recommended to regularly (for example, once a week) monitor their general blood count and are advised to always have antibacterial drugs with them. Consult your doctor for more information.
What can I do to prevent the infection from developing?
Your doctor will give you advice on necessary precautions during treatment, such as the following:
- To maintain the processes of formation of leukocytes and neutrophils, good nutrition with a sufficient amount of proteins and vitamins in the diet is extremely important; eat more meat, fish, seafood and other products. Monitor your weight during treatment; if it steadily decreases, be sure to inform your doctor about this;
- Wash your hands well, especially before eating. Avoid contact with germs. Try not to contact people who have cold symptoms. Thoroughly wash everything you eat, thoroughly heat-treat all meat and fish products you eat, and wash all fruits and vegetables before eating.
- Keep your body clean. If you have a catheter or venous port, keep the skin around it dry and clean. Use only a soft toothbrush, brush your teeth well and regularly, and check your mouth for any sores. In case of trauma to the skin, for example, by cutting yourself, carefully treat the injury site. Try not to visit crowded places unless necessary.
Treatment and prevention of neutropenia
If neutropenia develops again and again during treatment, or the development of infectious complications is noted during therapy, your doctor may decide to reduce (reduce) the doses of anticancer drugs. Reducing the dose of anticancer drugs reduces their negative impact on hematopoietic processes and, in many cases, helps prevent the development of neutropenia.
The so-called “granulocyte colony-stimulating factors (G-CSF)”, for example filgrastim, peg-filgrastim, etc. G-CSF promotes the formation of immune system cells in the bone marrow.
Typically, G-CSF is administered 24 to 72 hours after chemotherapy, either subcutaneously or intravenously. Their use makes it possible to effectively maintain the number of neutrophils and leukocytes in the blood and carry out more aggressive chemotherapy. Most patients give themselves these injections themselves, the most convenient is injection under the skin of the abdomen. A lot of training materials on the technique of performing them (for example) have been published on the Internet. Discuss with your doctor whether G-CSF is appropriate for your individual case.
ATTENTION! Infectious complications arising during antitumor treatment can pose an immediate threat to life. Do not self-medicate, consult a doctor.