Today, atherosclerotic cardiosclerosis is rightfully considered one of the most common diseases developing in people who have reached old age. In addition, the pathology is also one of the most dangerous due to the high probability of various complications that can lead not only to a deterioration in the patient’s quality of life, but also to the risk of death.
As you know, preventing any disease is much easier than treating it, so “you need to know the enemy by sight.” To prevent atherosclerotic cardiosclerosis and be able to recognize the early stages of the pathology, you should know in detail about the mechanism of its occurrence, predisposing factors, clinical manifestations and other aspects of the course of the disease.
Symptoms and signs
The severity of clinical manifestations directly depends on the degree of proliferation of connective tissue in the myocardium and the percentage of damaged cardiomyocytes. As a result of a decrease in the number of functioning cells, the ability of the heart muscle to pump blood is impaired, which leads to its stagnation in the systemic or pulmonary circulation. If the left side of the heart is affected, congestion occurs in the lungs, which causes shortness of breath (difficulty breathing), which worsens with physical exertion.
Lack of air is especially common at night, which is caused by the horizontal position of the body. The patient is forced to take the “orthopneic” position (sitting on the bed, leaning widely on it with his hands).
When the right side of the heart is damaged, blood stagnates in the systemic circulation. There is coldness and a feeling of chilliness in the arms and legs, heaviness and aching pain in the right hypochondrium, swelling mainly in the lower third of the legs.
Due to heart rhythm disturbances, attacks of dizziness, lightheadedness, and darkening of the eyes appear. With more severe arrhythmias, a person may lose consciousness.
Causes of cardiosclerosis
The Great Medical Encyclopedia connects the occurrence of pathology with the development of other diseases. Myocarditis, myocardial dystrophy, ischemic heart disease, myocardial infarction - everything that leads to necrosis of muscle tissue counts. The publication mentions three main causes of the disease:
- Inflammatory processes that affect the heart muscle and negatively affect its mobility.
- Unnatural increase in heart volume.
- Narrowing of adjacent vessels and the development of hypoxia.
Modern medicine lists the causes of cardiosclerosis as:
- Heredity.
- Bad habits (alcoholism, smoking, drug use, etc.).
- Stress and lack of proper rest.
- Insufficient or increased physical activity.
- systematic overeating; excessive consumption of spicy, fatty foods.
Causes
Myocarditis, and, consequently, this type of cardiosclerosis develops due to the following reasons.
- Coxsackie viruses, ECHO, herpes simplex viruses, influenza viruses, Epstein-Barr viruses, cytomegaloviruses.
- Bacteria: staphylococci, streptococci, enterococci, mycobacterium tuberculosis, less often - chlamydia, mycoplasma, rickettsia, borrelia, diphtheroids.
- Parasites and fungi: toxoplasma, trichinella, echinococcus, candida, aspergillus.
- Taking medications. Inflammation in the heart muscle can be caused either by the direct toxic effect of medications or by an indirect allergic reaction. Such medications include antibiotics, antituberculosis drugs, antidepressants and antitumor immunosuppressants (cytostatics).
- Autoimmune pathologies: acute rheumatic fever, systemic lupus erythematosus, systemic scleroderma, ankylosing spondylitis (ankylosing spondylitis).
The mechanism of pathology development
The pathogenesis (mechanism of development) of cardiosclerosis is as follows: after the resolution of acute inflammatory processes in the myocardium, so-called fibroblast growth factors are released from the destroyed cells. They stimulate the production of the main protein of connective tissue - collagen.
Large quantities of it form fibers that gradually replace normally functioning areas of the heart muscle. As a result, the pumping function of the myocardium deteriorates, and various rhythm disturbances occur.
However, this scenario does not always occur. Most people recover completely from myocarditis without significant residual effects. Why some patients develop cardiosclerosis and others do not is still a mystery. This may depend on the amount of cellular damage, the state of the immune system and many other factors.
Symptoms
As mentioned above, cardiosclerosis is the growth of connective tissue in the myocardium, which usually occurs after the death of muscle fibers or in parallel with this process. Clinical manifestations of cardiosclerosis directly depend on the type of pathology, of which there are four in medical practice.
Myocardial cardiosclerosis. The formation of a pathological process originates at the site of inflammation that occurs in the myocardium. The cause is proliferative and exudative foci in the stroma of the heart muscle, or destructive changes in myocytes (muscle cells). For this type of cardiosclerosis, the prerequisites are a history of allergic and infectious diseases, and the presence of chronic infectious foci.
Myocardial cardiosclerosis most often tends to develop in younger people. On the electrocardiogram (ECG), this disease manifests itself as diffuse changes in general or with large damage to the right ventricle. At the same time, deterioration of conductivity and rhythm disturbances are observed more often than manifestations of chronic heart failure (CHF).
The increase in heart size occurs evenly or with a bias to the right. Blood pressure is within normal limits, only sometimes a decrease is observed. Symptoms of chronic circulatory failure (CI) usually manifest themselves in the right ventricular type. In most cases, there are no deviations in biochemical blood parameters. Heart sounds are weakened, and a pathological third sound is often heard above the apex of the organ.
Diffuse changes in cardiosclerosis
Atherosclerotic cardiosclerosis. The disease, as a rule, develops quite slowly and is diffuse in nature. Occurs in the absence of focal necrotic changes in the myocardium. The development of pathology is caused by metabolic disorders and hypoxia, as a result of which slowly progressive dystrophy, atrophy and death of individual muscle fibers occur.
With the death of receptor cells, the myocardium loses sensitivity to oxygen, which ultimately leads to ischemic heart disease. However, clinical symptoms may remain mild for a long time. With further formation of connective tissue in the myocardium, the functional requirements for the remaining intact (healthy) myocytes increase accordingly.
Compensatory hypertrophy develops, and then dilatation (increase in chamber volume) of the heart. Basically, there is an enlargement of the left ventricle, and later the symptoms of heart failure (HF) are added - palpitations, shortness of breath, swelling of the legs, dropsy of the cavities and sometimes pulmonary edema.
As the disease progresses, dysfunction of the sinus node appears, for example, bradycardia. The formation of scar processes at the base of the valves, in the tendon threads and papillary muscles in a certain number of cases can cause the development of aortic or mitral valve stenosis, or heart failure of varying degrees of severity.
Auscultation reveals a weakening of heart sounds, especially the first at the apex; often a systolic murmur is detected in the aorta, up to an extremely rough sound characteristic of sclerosis (stenosis) of the aortic valve. A systolic murmur may also be heard at the apex, which is the result of relative incompetence of the mitral valve. NK most often develops in such situations according to the left ventricular type.
In atherosclerotic cardiosclerosis, blood pressure is higher than normal, biochemical parameters also undergo changes, expressed in hypercholesterolemia and an increase in beta-liproproteins. This type is very characterized by conduction and rhythm disturbances - often atrial fibrillation (atrial fibrillation), extrasystole, as well as blockades of various parts of the conduction system of varying severity.
Post-infarction cardiosclerosis. The pathology is focal in nature and develops against the background of replacement of a dead portion of the heart muscle with young connective tissue. The clinical picture is similar to the symptoms of atherosclerotic cardiosclerosis. Primary cardiosclerosis. An extremely rare type of disease. This includes cardiosclerosis, which forms with certain types of collagenosis, congenital fibroblastosis, etc.
Reference! The prognosis for cardiosclerosis is based on the extent of damage to the heart muscle, the presence and types of conduction and rhythm disturbances.
Changes in the myocardium in post-infarction cardiosclerosis
Diagnostics: how to suspect and determine
From personal practical experience I can say that the main thing is to know how the disease developed. A thorough survey allows you to establish the fact of myocarditis. It may be indicated by the appearance of pain in the heart, a feeling of palpitations, shortness of breath and constant weakness.
A general examination (physical examination) of the patient also plays an important role. In such patients, I usually pay attention to the color of the lips (it may be bluish), swollen veins in the neck, thickening of the terminal phalanges of the fingers (the so-called drumstick sign) and an enlarged liver.
Auscultation of the heart and lungs occupies a special place. The patient can hear noises, dull tones, irregular rhythm, and moist rales in the lower parts of the lungs. In severe and advanced cases, when there is severe circulatory insufficiency, an auscultatory phenomenon appears - “gallop rhythm”, characterized by the appearance of a third tone between two physiological ones.
After a survey and general examination of the patient, I make a preliminary diagnosis. To confirm or exclude it, you need to undergo an additional examination, including the following.
- General and biochemical blood tests - they do not provide enough data to diagnose cardiosclerosis itself, but sometimes they reveal abnormalities that could cause the development of myocarditis.
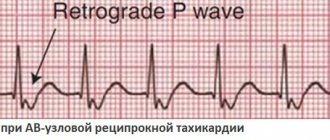
- Electrocardiography. The ECG shows nonspecific changes: ST segment elevation and negative T wave. Cardiac rhythm and conduction disturbances are often detected in the form of supraventricular and ventricular extrasystoles, atrial fibrillation and flutter, atrioventricular block and bundle branch block.
- Chest X-ray - may reveal enlarged heart borders and signs of pulmonary congestion.
- Echocardiography (ultrasound of the heart, ECHO-CG) - allows you to see thickening of the myocardial walls, dilatation (expansion) of the atria and ventricles, areas of impaired muscle contractility.
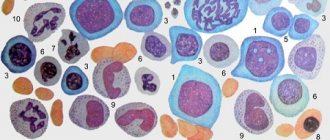
- Endomyocardial biopsy - according to modern recommendations, the diagnosis of cardiosclerosis is established by histological examination of the myocardium. However, due to the technical complexity, I rarely prescribe this procedure to my patients.
Treatment and its methods
The need for hospitalization depends on the severity of the patient's condition. In most cases, outpatient treatment is sufficient. The use of antiviral, antibacterial, and antifungal drugs is pointless, since at the time of the formation of cardiosclerosis the pathogen has already left the body.
The first stage of treatment is to limit physical activity. Professional sports are strictly contraindicated. Aerobic exercise and physical therapy are allowed. I explain to my patients that they should follow a low-salt diet, consuming no more than 2-3 grams per day. This is necessary to prevent fluid stagnation in the body.
The basis of treatment is drug therapy. To slow the progression of heart failure, I use medications from the following pharmacological groups: ACE inhibitors (Perindopril, Ramipril), beta-blockers (Bisoprolol, Nebivalol) and mineralocorticoid receptor antagonists (Spironolactone). For severe congestion, I prescribe diuretics—loop diuretics (“Furosemide”, “Torasemide”).
Treatment methods for arrhythmias are determined by their type, severity and accompanying symptoms. With atrial fibrillation and flutter, blood clots form in the cavities of the heart, which can migrate and clog a vessel in an organ, such as the brain, thereby causing an ischemic stroke. Therefore, to prevent thrombosis, I use anticoagulants (Warfarin, Dabigatran, Apixaban, Xarelto).
If arrhythmias are accompanied by symptoms such as dizziness and fainting, it is worth considering the option of taking medications that normalize cardiac activity, such as Propafenone, Sotalol. If there is resistance to drug therapy, surgical intervention is performed - radiofrequency ablation. For severe atrioventricular blockade, installation of a pacemaker is indicated.
Treatment methods
To select the most appropriate treatment tactics for atherosclerotic cardiosclerosis, the patient is prescribed a full range of diagnostic procedures. These measures are necessary to determine the degree of damage to the myocardium by connective tissue scars, the type of disease, the number of foci and to determine the cause of the pathology. The list of examinations most often includes:
- Dynamic ECG;
- echocardiogram;
- MRI;
- examination of coronary vessels (if coronary artery sclerosis is suspected).
There is no single approach to the treatment of cardiosclerosis. The complex of therapeutic measures being developed is aimed at eliminating the causes of pathology - inflammation of the heart muscle, atherosclerosis in coronary heart disease or the consequences of myocardial infarction. Thus, with the post-myocardial form of cardiosclerosis, the emphasis will be on the treatment of an allergic reaction or infection that led to the onset of the disease.
In case of diffuse atherosclerotic form, it will be necessary to reduce the cholesterol content in the patient’s blood and prescribe treatment aimed at restoring blood flow in the coronary arteries, as well as correcting blood pressure. For this purpose, anticoagulants and vasodilators are used. To reduce the symptoms of heart failure, diuretics, cardiac glycosides, beta blockers, etc. are prescribed.
In case of severe obstruction of the patency of the coronary arteries, in some situations the question of surgical intervention, such as coronary artery bypass grafting or stenting, may arise. During the treatment of cardiosclerosis, the patient’s diet, lifestyle and physical activity must be adjusted. Developing healthy habits and following basic nutritional rules is one of the important aspects of recovery from atherosclerotic cardiosclerosis.
Complications: what causes death and in what cases
Adverse consequences are observed in diffuse forms of cardiosclerosis. These include acute heart failure, including pulmonary edema and cardiogenic shock (a sharp decrease in the pumping function of the heart).
With severe rhythm disturbances, sudden cardiac death may occur due to ventricular fibrillation and asystole (complete cardiac arrest). These conditions very often end in death. They occur in approximately 5-10% of cases of post-myocardial cardiosclerosis.
Typology of the disease
Today, two approaches to the classification of cardiosclerosis are proposed. The first relies on the history of the disease and proposes to subdivide it into atherosclerotic and myocardial. The second approach is based on the localization of the disease, depending on which cardiosclerosis can be either diffuse or focal. Let's look at these terms in more detail:
- The atherosclerotic form of the disease got its name in honor of the pathology that causes it - atherosclerosis of the arteries.
- Myocardial cardiosclerosis is a direct consequence of various types of myocarditis.
- The diffuse type of the disease is diagnosed when necrosis affects muscle tissue relatively evenly.
- In focal cardiosclerosis (also known as scar), connective tissue replaces muscle tissue in individual areas of the heart, varying in size.
Consequences of cardiosclerosis
- Aneurysms and heart defects.
- Arrhythmia.
- Thromboembolism.
- Chronic fatigue syndrome.
- Chronic heart failure.
Clinical case
A 49-year-old man came to see me with complaints of weakness, increased fatigue, difficulty breathing, and frequent attacks of dizziness.
Last night I lost consciousness, which was the reason for visiting the doctor. During the interview, it turned out that six months ago, after a cold, the patient developed chest pain, to which the patient did not attach much importance. Auscultation revealed a weak, irregular heartbeat of 42 beats per minute. The ECG revealed complete atrioventricular block, the ventricular contraction rate was 35-47 per minute. Echo-CG showed thickening of the myocardial walls, zones of hypokinesis (reduced contractility) and a small ejection fraction (45%). I suspected postmyocardial cardiosclerosis. At the medical consultation, it was decided to perform an endomyocardial biopsy. The resulting histological specimen revealed myocardial fibrosis and degenerative cell changes.
The final diagnosis was: “Myocarditis, unspecified. Complications: NYHA class II CHF, complete AV block.” The patient was prescribed medications to treat heart failure and had a permanent pacemaker implanted. After the operation, the patient feels satisfactory, dizziness and shortness of breath are no longer bothersome.