Situations with GPP
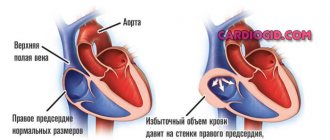
Venous blood from the venae cava enters the right atrium. Overload of the right atrium occurs when blood enters from the vena cava in excess or with pulmonary hypertension, when blood from the right atrium to the right ventricle cannot pass immediately and completely. As a result, the atrium cavity begins to gradually expand and the wall thickens.
Another reason for overload of the right atrium is hypertension in the pulmonary circulation, which leads to hypertension in the right ventricle. For this reason, blood from the PP cannot immediately pass into the ventricle, which also leads to GPP. The load on the right side of the heart also increases with chronic lung diseases. The main reason is excess blood and pressure.
This condition occurs when there is stenosis of the tricuspid valve, which separates the atrium from the ventricle. In this case, some of the blood gets stuck in the atrium. Most often, this defect occurs after a rheumatic attack, with bacterial endocarditis.
Another defect is the insufficiency of the specified valve, in which its valves do not close completely and some of the blood returns. This condition occurs when the left ventricle dilates. Pressure load will occur with pulmonary pathologies: bronchitis, emphysema, asthma, genetic disease of the pulmonary artery. These diseases increase the volume of blood in the ventricle, and after this the atrium becomes overstrained. This is why overload of the right atrium and right ventricle are so often combined.
To restore normal blood flow, the atrium has to push blood out with greater force, and it hypertrophies. Overload of the right atrium develops gradually when the causative disease remains undiagnosed and untreated.
The time is individual for each patient, but the result is always depletion of the compensatory capabilities of the heart muscle and the onset of decompensated heart failure in a chronic course.
What is right atrium load?
Overload of the right side of the heart occurs when pressure in the pulmonary arteries increases and the formation of cor pulmonale. The causes of this pathological condition can be very different, but most often the following factors contribute to hypertrophic changes in the right atrium:
- heredity;
- congenital heart defects;
- mitral stenosis and tricuspid valve prolapse;
- right ventricular hypertrophy;
- stable arterial hypertension;
- lung diseases: emphysema, bronchiectasis, asthma, chronic bronchitis with obstruction, etc.;
- obesity;
- metabolic acidosis;
- chronic stress.
According to WHO, more than 7 million people die from heart disease every year worldwide. Signs of right atrium overload – shortness of breath with minimal exertion, heaviness in the chest. If you experience similar symptoms, do not hesitate to visit a doctor.
Right atrium overload
What is right atrial overload?
The task of the heart muscle is to pump blood throughout the body, while simultaneously saturating all tissues and organs with oxygen. From the right atrium, it passes through a special valve and enters the right ventricle. The valve's job is to prevent blood from flowing back. Instead, she moves on.
Signs of right atrium overload - pain and heaviness in the chest
Passing through the pulmonary circulation, it is saturated with oxygen and enters the aorta.
Overload of the right atrium develops in a situation when the amount of blood in it becomes more than acceptable. Its cavity gradually expands and the wall thickens.
Right atrial hypertrophy
The load on the right atrium is determined by the amount of blood that enters it, as well as how the blood is released during atrial contraction. If an excess amount of blood enters, the pressure on the chamber walls will increase, which will inevitably be accompanied by overload.
If there is a problem with the valve between the atrium and the right ventricle in the form of a narrowing, blood from the atrium will flow out with difficulty, and some of the blood will be retained in the atrium.
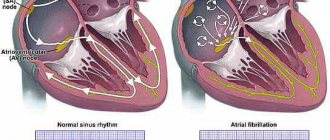
The heart pumps blood throughout the body. From the atria, blood enters the ventricles through the openings and is then pushed out into the vessels.
The right atrium is able to accommodate a certain volume of blood, if for some reason this volume exceeds the permissible level, the muscle tissue of the heart begins to work more actively to expel this excess volume, protective mechanisms are launched and the muscle tissue grows - hypertrophies, the walls of the atrium thicken - so it is easier for them to cope with the load.
This condition is right atrial hypertrophy. All causes leading to hypertrophy can be divided into two large groups: heart disease and lung disease. Let's look at these reasons in more detail:
- Chronic lung diseases: chronic obstructive pulmonary disease, bronchial asthma, pulmonary emphysema. With lung pathology, the pressure in the pulmonary artery system increases, the pressure in the right ventricle and then the right atrium increases, and hypertrophy of the right chambers of the heart occurs;
- Deformation of the chest: kyphosis, severe scoliosis;
- Changes in the tricuspid valve: narrowing (stenosis) or insufficiency. If the opening connecting the right ventricle and the right atrium is narrowed, blood cannot flow into the ventricle in full; the right atrium becomes overfilled, thickens, and subsequently expands; blood stagnates in the atrium and in the vena cava system. In case of valve insufficiency, blood, on the contrary, pours abundantly into the atrium, with contraction of the ventricle, which also leads to thickening and hypertrophy;
- Myocarditis;
- Endocarditis;
- Congenital heart defects: atrial septal defect, Ebstein's anomaly, tetralogy of Fallot.
Mechanism of development and types of hypertrophy of the right atrium
With defects of the tricuspid valve (this is the three-cuspid septum between the right atrium and the ventricle), the opening through which blood normally flows freely from the atrium into the ventricle is greatly narrowed or does not close enough.
This disrupts intracardiac blood flow:
- after filling the ventricle at the time of diastole (relaxation), an extra portion of blood remains in the atrium;
- it puts more pressure on the myocardial walls than during normal filling and provokes their thickening.
With pathology in the pulmonary circulation (pulmonary diseases), blood pressure in the pulmonary vessels and in the right ventricle increases (the pulmonary or pulmonary circulation begins from there).
This process prevents the free flow of the required volume of blood from the atrium into the ventricle; part of it remains in the chamber, increases pressure on the walls of the atrium and provokes the growth of the muscular layer of the myocardium.
Most often, right atrial hypertrophy develops against the background of cardiovascular disorders, but sometimes it becomes a consequence of regular physical activity or myocardial necrosis.
Depending on the factor under the influence of which the thickening of the chamber walls appeared, there are:
- Regenerative hypertrophy due to scarring at the site of necrosis (after a heart attack). The atrial myocardium grows around the scar, trying to restore cell function (conduction and contraction).
- Replacement as a way for the heart muscle to compensate for circulatory deficiencies under the influence of various pathologies and negative factors.
- Working – a form that develops under the influence of regular physical activity (professional training), as a protective mechanism for increased heart rate, hyperventilation of the lungs, increased pumped blood volume, etc.
2Causes of overload
In medical practice, hypertrophy of the right atrium, compared to the left, is quite rare. This is due to the fact that the left ventricle is responsible for hemodynamics (blood movement through the vessels) in the systemic circulation and is subject to considerable stress when the right ventricle directs blood to the pulmonary circulation.
And excessive load on the ventricle, as a rule, becomes the cause of functional changes in the accompanying atrium. The right atrium experiences overload as pressure in the pulmonary artery increases.
This moment is influenced by various circumstances:
- pulmonary diseases: bronchitis, bronchial asthma, pulmonary embolism (blockage of the arterial bed of a paired organ with a blood clot), emphysema (excessive accumulation of air in the organs), pneumonia or pneumonia;
- narrowing of the tricuspid valve, which separates the right atrium and ventricle. The valve opening decreases, and with it the amount of flowing blood;
- congenital changes in heart structures (defects);
- myocardial infarction;
- regular physical activity.
Changes in wall thickness and dilatation of the internal cavity of the right atrium appear with increasing load: venous blood collects in the right parts of the heart, which enters the pulmonary circulation through the pulmonary artery and is saturated with oxygen in the lungs.
Right atrium pressure overload is characteristic of tricuspid valve stenosis. This is an acquired heart defect, in which the area of the opening between the atrium and the ventricle decreases. Tricuspid valve stenosis may be due to endocarditis.
With another acquired heart defect, tricuspid valve insufficiency, the right atrium experiences volume overload. In this condition, blood from the right ventricle, when it contracts, flows not only into the pulmonary artery, but also back into the right atrium, causing it to work under overload.
Congenital malformations such as tetralogy of Fallot can lead to right atrial hypertrophy. Right atrium pressure overload is characteristic of tricuspid valve stenosis. This is an acquired heart defect, in which the area of the opening between the atrium and the ventricle decreases. Tricuspid valve stenosis may be due to endocarditis.
The right atrium is enlarged in some congenital heart defects. For example, with a significant atrial septal defect, blood from the left atrium enters not only the left ventricle, but also through the defect into the right atrium, causing its overload.
Congenital malformations such as tetralogy of Fallot can lead to right atrial hypertrophy.
Right atrium pressure overload is characteristic of tricuspid valve stenosis. This is an acquired heart defect, in which the area of the opening between the atrium and the ventricle decreases. Tricuspid valve stenosis may result from endocarditis.
In the practice of cardiologists, overload of the left atrium is more common, but the right atrium can also be subject to excessive load. The reasons for this phenomenon are:
- chronic pulmonary diseases (bronchial asthma, chronic bronchitis, emphysema),
- pathology of the tricuspid valve (its narrowing or insufficiency),
- congenital heart and vascular defects,
- cardiomyopathies, endocarditis, myocarditis,
- endocrine diseases (thyrotoxicosis),
- chest injury or deformation.
All these reasons lead to an increase in pressure in the pulmonary artery, and the formation of chronic pulmonary heart occurs.
Signs of right atrial hypertrophy
Right atrium hypertrophy is expressed by pain in the chest, respiratory problems, and fatigue. Often, unfavorable symptoms are preceded by: pneumonia, exacerbation of bronchial asthma, pulmonary artery embolism, etc.
After treatment of the underlying disease, anxiety symptoms may subside and even disappear completely. In addition to the clinical manifestations of pulmonary problems, with hypertrophy there may be signs of venous stagnation. Alarming signs of right atrial hypertrophy are characterized by:
- cough, shortness of breath, deterioration of respiratory function;
- swelling;
- paleness of the skin, cyanosis;
- dulling of attention;
- minor tingling, discomfort in the heart area;
- heart rhythm pathology.
In most cases, hypertrophy is asymptomatic, and the manifestation of clinical symptoms is noted already in an advanced stage. Consult your doctor immediately if you notice rapid heartbeat, dizziness (loss of consciousness), swelling of the lower extremities.
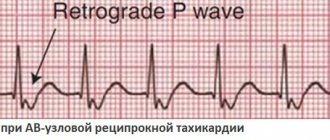
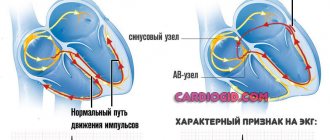
With hypertrophy of the right atrium, the EMF created by it increases, while the excitation of the left atrium occurs normally. The top figure shows the formation of the P wave normally:
- excitation of the right atrium begins slightly earlier and ends earlier (blue curve);
- excitation of the left atrium begins somewhat later and ends later (red curve);
- the total vector of the EMF of excitation of both atria draws a positive smoothed P wave, the leading edge of which forms the beginning of excitation of the right atrium, and the rear edge forms the end of excitation of the left atrium.
With hypertrophy of the right atrium, the vector of its excitation increases, which leads to an increase in the amplitude and duration of the first part of the P wave (lower picture), due to excitation of the right atrium.
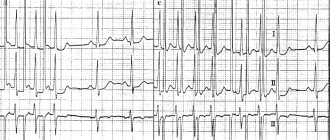
With hypertrophy of the right atrium, its excitation ends simultaneously with the excitation of the left atrium or even slightly later. As a result, a tall, pointed P wave is formed - a characteristic sign of right atrium hypertrophy:
- The height of the pathological P wave exceeds 2-2.5 mm (cells);
- The width of the pathological P wave is not increased; less often - increased to 0.11-0.12 s (5.5-6 cells);
- As a rule, the apex of the pathological P wave is symmetrical;
- A pathological high P wave is recorded in standard leads II, III and enhanced lead aVF.
Characteristic signs of a pathological P wave with hypertrophy of the right atrium in various leads:
- In standard lead I, the P wave is often negative or smoothed (less often, a high, pointed P wave is observed in leads I, aVL);
- Lead aVR is characterized by the presence of a deep, pointed negative P wave (usually its width is not increased);
- In chest leads V1, V2, the P wave becomes high, pointed or biphasic with a sharp predominance of the first positive phase (normally, the P wave in these leads is biphasic, smoothed);
- Occasionally, the P wave in lead V1 is weakly positive, weakly negative, or smoothed, but in leads V2, V3 a high pointed P wave is recorded;
- The greater the hypertrophy of the right atrium, the greater the number of chest leads with a high, pointed positive P wave (in leads V5, V6 the P wave is usually reduced in amplitude).
Right atrium activation time is measured in leads III or aVF or V1. With hypertrophy of the right atrium, an increase in the time of its activation in these leads is characteristic (exceeds 0.04 s or 2 cells).
With right atrial hypertrophy, the Macruse index (the ratio of the duration of the P wave to the duration of the PQ segment) is often less than the lower acceptable limit - 1.1.
An indirect sign of right atrium hypertrophy is an increase in the amplitude of the P waves in leads II, III, aVF, while the pathological P wave in each lead is larger in amplitude than the following T wave (normally PII, III, aVF
Source: https://serdse.top/pravoe-predserdie/
Other diseases leading to GPP
The development of right atrium overload can be provoked by:
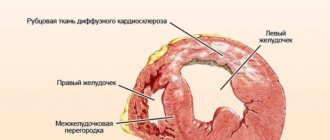
- Myocardial remodeling - this phenomenon is considered part of post-infarction cardiosclerosis, when a scar develops at the site of necrosis. Healthy cardiomyocytes become more voluminous - they thicken, which outwardly looks like hypertrophied muscle. This is also a compensatory mechanism and most often involves the left ventricle. This creates another combination of right atrial overload and left ventricular diastolic overload.
- Postmyocardial cardiosclerosis - scar tissue is formed by the same mechanisms, but after inflammatory processes in the myocardium.
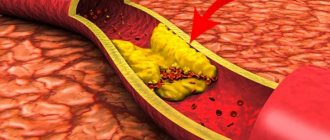
- Coronary heart disease - here we are talking about blockage of the coronary artery with a thrombus or plaque of atherosclerosis. This necessarily causes myocardial ischemia, and the contractile function of cardiomyocytes is impaired. Then the areas of the myocardium adjacent to the affected areas begin to thicken compensatoryly.
- Hypertrophic cardiomyopathy - occurs due to gene disorders in which uniform thickening of the myocardium of the entire heart muscle occurs. It is more often typical for children and involves the myocardium of the right atrium, then overload of the right atrium in the child is recorded.
Of the congenital pathological conditions of the heart muscle, heart overload is caused by:
- Defective septum between the atria. With such a deviation, the heart supplies blood to the right and left half of the heart under the same pressure, as a result of which the atrium receives an increased load.
- Ebstein's anomaly is a rare defect in which the atrioventricular valve leaflets are adjacent to the right ventricle rather than to the atriogastric ring. Then the right atrium merges with part of the right ventricle and also hypertrophies.
- Transposition of the great vessels - the main arteries of the cardiovascular system change their anatomical position - the main artery of the lungs is separated from the left parts of the heart, and the aorta is separated from the right. In these cases, GPP occurs in a child under 1 year of age. This is a very serious deviation.
- It is also possible to overload the right atrium in adolescents prone to fanatical sports. Regular physical activity is a common cause of HPP.
Right atrium overload: signs, causes, treatment methods, reviews
According to WHO statistics, more than 5 million people die every year from heart pathologies. Right atrium overload (RAO) or its hypertrophy is rare among cardiac pathologies, but its significance is great because it entails changes in other body systems.
A little physiology
The human heart includes 4 chambers, each of which, for certain reasons, can enlarge and hypertrophy. Typically, hypertrophy is an attempt by the body to overcome any organ failure with this compensation. Hypertrophy of the heart does not become an independent disease - it is a symptom of other pathologies.
The main function of the heart is to create blood flow to supply all tissues and organs with nutrients and oxygen.
Situations with GPP
Venous blood from the venae cava enters the right atrium. Overload of the right atrium occurs when blood enters from the vena cava in excess or with pulmonary hypertension, when blood from the right atrium to the right ventricle cannot pass immediately and completely. As a result, the atrium cavity begins to gradually expand and the wall thickens.
Another reason for overload of the right atrium is hypertension in the pulmonary circulation, which leads to hypertension in the right ventricle. For this reason, blood from the PP cannot immediately pass into the ventricle, which also leads to GPP. The load on the right side of the heart also increases with chronic lung diseases. The main reason is excess blood and pressure.
This condition occurs when there is stenosis of the tricuspid valve, which separates the atrium from the ventricle. In this case, some of the blood gets stuck in the atrium. Most often, this defect occurs after a rheumatic attack, with bacterial endocarditis.
Another defect is the insufficiency of the specified valve, in which its valves do not close completely and some of the blood returns. This condition occurs when the left ventricle dilates.
Pressure load will occur with pulmonary pathologies: bronchitis, emphysema, asthma, genetic disease of the pulmonary artery. These diseases increase the volume of blood in the ventricle, and after this the atrium becomes overstrained.
This is why overload of the right atrium and right ventricle are so often combined.
To restore normal blood flow, the atrium has to push blood out with greater force, and it hypertrophies. Overload of the right atrium develops gradually when the causative disease remains undiagnosed and untreated.
The time is individual for each patient, but the result is always depletion of the compensatory capabilities of the heart muscle and the onset of decompensated heart failure in a chronic course.
Other diseases leading to GPP
The development of right atrium overload can be provoked by:
- Myocardial remodeling - this phenomenon is considered part of post-infarction cardiosclerosis, when a scar develops at the site of necrosis. Healthy cardiomyocytes become more voluminous - they thicken, which outwardly looks like hypertrophied muscle. This is also a compensatory mechanism and most often involves the left ventricle. This creates another combination of right atrial overload and left ventricular diastolic overload.
- Postmyocardial cardiosclerosis - scar tissue is formed by the same mechanisms, but after inflammatory processes in the myocardium.
- Coronary heart disease - here we are talking about blockage of the coronary artery with a thrombus or plaque of atherosclerosis. This necessarily causes myocardial ischemia, and the contractile function of cardiomyocytes is impaired. Then the areas of the myocardium adjacent to the affected areas begin to thicken compensatoryly.
- Hypertrophic cardiomyopathy - occurs due to gene disorders in which uniform thickening of the myocardium of the entire heart muscle occurs. It is more often typical for children and involves the myocardium of the right atrium, then overload of the right atrium in the child is recorded.
Of the congenital pathological conditions of the heart muscle, heart overload is caused by:
- Defective septum between the atria. With such a deviation, the heart supplies blood to the right and left half of the heart under the same pressure, as a result of which the atrium receives an increased load.
- Ebstein's anomaly is a rare defect in which the atrioventricular valve leaflets are adjacent to the right ventricle rather than to the atriogastric ring. Then the right atrium merges with part of the right ventricle and also hypertrophies.
- Transposition of the great vessels - the main arteries of the cardiovascular system change their anatomical position - the main artery of the lungs is separated from the left parts of the heart, and the aorta is separated from the right. In these cases, GPP occurs in a child under 1 year of age. This is a very serious deviation.
- It is also possible to overload the right atrium in adolescents prone to fanatical sports. Regular physical activity is a common cause of HPP.
Symptomatic manifestations of pathology
GPP itself has no symptoms. Only symptoms associated with the underlying disease, which are complemented by venous stagnation, may be of concern.
Then we can say that signs of overload of the right atrium are shortness of breath even with minor exertion, pain behind the sternum.
Circulatory failure and cor pulmonale may develop. With cor pulmonale:
- shortness of breath in a horizontal position and with the slightest exertion;
- cough at night, sometimes mixed with blood.
Insufficient blood flow:
- heaviness in the right side of the chest;
- swelling in the legs;
- ascites;
- dilatation of veins
There may also be causeless fatigue, arrhythmias, tingling in the heart, and cyanosis. If these complaints arose only during infections and for the first time, you can count on their disappearance after treatment. For monitoring, a dynamic ECG is performed.
Diagnostics
There are no specific signs of pathology. It is only possible to assume the presence of overloads if a person suffers from chronic lung pathologies or has problems with valves.
In addition to palpation, percussion and auscultation, an ECG is used, which is used to determine some signs of right atrium overload on the ECG. However, even these indicators may be present only temporarily and disappear after the processes are normalized. In other cases, a similar picture may indicate the beginning of the process of atrial hypertrophy.
Ultrasound helps determine the increase in pressure and the volume of blood located in various parts of the heart. This method can detect disorders in all parts of the heart and blood vessels.
Pulmonary heart (P-pulmonale)
With it, pathological changes occur in the pulmonary circulation, and this is the main reason for overload of the right atrium.
On the ECG this is reflected by a modified P wave (atrial wave). It becomes tall and pointed in the form of a peak instead of the smooth apex of normal.
Functional overload of the right atrium on the ECG can also give an altered P - this is noted, for example, with overactivity of the thyroid gland, tachycardia, etc. Deviation of the heart axis to the right does not always occur only with HPP; it can also be normal in high asthenics. Therefore, other studies are used for differentiation.
If signs of right atrium overload are detected on the ECG, the patient is recommended to undergo echocardiography. It is considered safe for any category of patients and can be repeated many times over time. Modern devices can give answers about the thickness of the heart walls, the volume of the chambers, etc.
Together with echocardiography, the doctor may also prescribe Doppler ultrasound, then you can obtain information about hemodynamics and blood flow.
If there is a divergence of opinions, CT or radiography is prescribed. X-ray examination shows abnormalities of the right atrium and ventricle. Their contours merge with the contours of the vessels. In addition, an x-ray will show the condition of other structures of the chest, which is very valuable in case of pulmonary pathology as the root cause of HPP.
Consequences of GPP
In chronic diseases of the pulmonary system, the active alveoli are replaced by fibrous tissue, and the gas exchange area becomes smaller. Microcirculation is also disrupted, which leads to increased pressure in the pulmonary circulation. The atria have to actively contract, which ultimately causes their hypertrophy.
Thus, the complications and consequences of GPP are:
- expansion of the heart chambers;
- circulatory disorders, first in the small and then in the large circle;
- formation of the pulmonary heart;
- venous congestion and heart valve insufficiency.
If left untreated, pulse irregularities and attacks of heart failure may develop, which can lead to death.
Treatment
Normalizing the size of the atrium and improving the functioning of the heart muscle is only possible if the underlying disease – the cause of the pathology – is treated. Such treatment is always complex; monotherapy does not make sense.
In the presence of pulmonary pathology, these are bronchodilators (tablets and inhalers), antibacterial therapy for bacterial etiology of disorders, anti-inflammatory drugs.
For bronchiectasis, surgical treatment is used.
In case of heart defects, the best solution is corrective surgery. After heart attacks and myocarditis, it is necessary to prevent remodeling with the help of antihypoxic and cardioprotective drugs.
Antihypoxants are indicated: “Actovegin”, “Mildronate”, “Mexidol” and “Preductal”. Cardioprotectors: ACEs or angiotensin II receptor antagonists (ARA II). They can actually slow down the onset of chronic heart failure. More often than others, Enalapril, Quadropril, Perindopril, etc. are prescribed.
Nitrones, beta blockers (“Metoprolol”, “Bisoprolol”, “Nebivalol”, etc.), ACE inhibitors, antiplatelet agents that prevent the formation of blood clots, statins that normalize the amount of cholesterol are required.
Also used in treatment are glycosides (according to indications) and antiarrhythmics, agents that improve metabolic processes in the heart muscle. Judging by the reviews, good results were obtained when prescribing Riboxin.
Relapse Prevention
If drug therapy is the prerogative of the doctor, greater responsibility falls on the patient himself. Without his participation, the efforts of doctors will not produce results.
A person must definitely reconsider his lifestyle: give up smoking and alcohol, establish proper nutrition, eliminate physical inactivity, adhere to a daily routine, exercise moderate physical activity, and normalize body weight.
If pathologies of the cardiovascular and pulmonary systems become chronic, they cannot be completely cured.
The condition can only be improved by preventing exacerbations of these pathologies. Then the load on the cardiac system decreases.
GPP and pregnancy
During pregnancy, the body undergoes enormous changes not only in terms of hormonal balance, but also in the functioning of internal organs.
A difficult situation arises when diagnosing right atrium overload during pregnancy, which in this situation is considered an extragenital disease.
The diagnosis must not only be established, but also the woman’s ability to bear a fetus and give birth.
The best option, of course, is to diagnose heart pathologies before conception, but this does not always happen. Most often, pregnant women with heart pathologies are hospitalized three times during gestation; this is done to monitor the condition over time.
When first admitted to the hospital, the defect is examined, the activity of the process is determined and the work of the blood circulation is assessed, taking into account the question of a possible termination of pregnancy.
Repeated hospitalization is necessary because the physiological stress of the body to maintain the functioning of the heart muscle in a woman reaches its peak. The third hospitalization helps doctors choose the method of delivery.
Preventive actions
Prevention of right atrium hypertrophy begins with a review of the lifestyle, which involves proper balanced nutrition and a rational work and rest schedule.
If you are not a professional athlete and you do not necessarily need Olympic medals, do not show stubborn fanaticism in playing sports. This exhausts the body and exhausts the heart. The pressure in the circulatory system increases, and hypertrophy will not take long to occur.
Daily walks of an hour a day, swimming, and cycling are quite enough.
Another problem is eliminating stress. They also have a very negative impact on the functioning of the heart and the entire body as a whole. Yoga, meditation, and relaxation can help solve the problem.
Source: https://FB.ru/article/397136/peregruzka-pravogo-predserdiya-priznaki-prichinyi-metodyi-lecheniya-otzyivyi
Symptomatic manifestations of pathology
GPP itself has no symptoms. Only symptoms associated with the underlying disease, which are complemented by venous stagnation, may be of concern.
Then we can say that signs of overload of the right atrium are shortness of breath even with minor exertion, pain behind the sternum.
Circulatory failure and cor pulmonale may develop. With cor pulmonale:
- shortness of breath in a horizontal position and with the slightest exertion;
- cough at night, sometimes mixed with blood.
Insufficient blood flow:
- heaviness in the right side of the chest;
- swelling in the legs;
- ascites;
- dilatation of veins
There may also be causeless fatigue, arrhythmias, tingling in the heart, and cyanosis. If these complaints arose only during infections and for the first time, you can count on their disappearance after treatment. For monitoring, a dynamic ECG is performed.
Is the condition dangerous if a load on the right atrium is detected on the ECG?
If the right atrium (RA) is overfilled with blood or pressure overload, myocardial hypertrophy subsequently occurs. Signs of this condition are shortness of breath, dizziness, fainting, and irregular contractions. Treatment requires an impact on the disease that caused overstrain of the heart muscle (lung disease, valvular heart disease).
Causes of increased load on the right atrium of the myocardium
In order for the load on the cardiac muscle of the RA to increase when blood is ejected into the ventricle, the pressure in it must increase due to an obstruction (tricuspid valve stenosis) or the blood volume must increase.
This situation occurs with reverse reflux (valvular insufficiency), high pressure in the right ventricle (heart defects).
Diseases leading to overload, and subsequently hypertrophy of the PP, may differ in adulthood and childhood.
In adults
The most common pathologies accompanied by a large load on the right atrium:
- chronic bronchitis (obstructive);
- bronchial asthma;bronchial asthma
- emphysema of pulmonary tissue;
- hardening of the lungs (pneumosclerosis);
- multiple cysts;
- bronchiectasis;
- tuberculosis infection;
- sarcoidosis;
- pneumonia;
- occupational lung diseases;
- chest injuries and deformities, operations;
- obesity;
- pulmonary hypertension (primary and secondary forms);
- autoimmune diseases;
- thrombosis, embolism and atherosclerosis of pulmonary vessels;
- tumors in the chest.
All these processes disrupt the ejection of blood from the right ventricle into the lungs, which leads to its overstrain and subsequent hypertrophy, and the RA is affected for the second time.
Also causes of pathological changes include rheumatism, endocarditis involving the tricuspid valve.
Excessive load on the RA occurs with tricuspid stenosis, insufficiency and combined acquired defect of this valve.
We recommend reading the article on myocardial hypertrophy. From it you will learn about the mechanism of development and types of myocardial hypertrophy, as well as about the diagnosis and treatment of the disease.
And here is more information about left atrial hypertrophy.
The child has
The first place among the factors of PP overload is taken by heart defects, in which circulatory disorders occur in the pulmonary circulation:
Right atrium overload
The addition of hypertrophy of the right parts of the heart occurs with decompensation of circulatory failure of the left ventricular type. This is due to the increase in congestion in the lungs, which over time complicates the work of the right atrium.
Signs and symptoms of stress
If overstrain of the PP occurs against the background of acute inflammatory processes or exacerbation of bronchial asthma, bronchitis, then there are no characteristic symptoms, or the overload is manifested by an excessive increase in shortness of breath during physical activity. If the underlying diseases are heart defects, then the signs are:
- increasing weakness and fatigue;
- cardiopalmus;
- pain and heaviness in the liver area;
- indigestion;
- cyanotic or icteric skin tone;
- swelling in the legs;
- accumulation of fluid in the abdominal cavity;
- pulsation of neck veins.
Is it dangerous
Increased load on the right atrium does not have negative consequences if it is possible to eliminate its cause - through medical or surgical treatment of the underlying disease. With unoperated heart defects, heart failure and congestive processes in the internal organs develop quite early, many of which have irreversible consequences.
In the later stages, fluid accumulates in the abdominal cavity (ascites), chest (hydrothorax), pericardial sac (hydropericardium), liver cirrhosis and severe rhythm disturbances occur.
ECG readings of load on the right atrium
Short-term manifestations of PP overload can be detected by recording an ECG at the time of an asthma attack, thromboembolism, or extensive pneumonia:
- pulmonary (pulmonary) P wave;
- increase in the first (right atrial part) P;
- high and pointed P in leads 2 and 3, aVF.
These symptoms disappear after the patient’s condition normalizes, or their severity decreases significantly. With hypertrophy, the P waves are high-amplitude, pointed, and have a normal duration.
ECG changes with increasing pulmonary hypertension and chronic overstrain of the RA are usually combined with symptoms of right ventricular hypertrophy . If an overload is detected, chest X-ray, cardiac ultrasound with Doppler ultrasound, CT and MRI are indicated to find the cause of the abnormalities.
Diagnostics
There are no specific signs of pathology. It is only possible to assume the presence of overloads if a person suffers from chronic lung pathologies or has problems with valves.
In addition to palpation, percussion and auscultation, an ECG is used, which is used to determine some signs of right atrium overload on the ECG. However, even these indicators may be present only temporarily and disappear after the processes are normalized. In other cases, a similar picture may indicate the beginning of the process of atrial hypertrophy.
Ultrasound helps determine the increase in pressure and the volume of blood located in various parts of the heart. This method can detect disorders in all parts of the heart and blood vessels.
Pulmonary heart (P-pulmonale)
With it, pathological changes occur in the pulmonary circulation, and this is the main reason for overload of the right atrium.
On the ECG this is reflected by a modified P wave (atrial wave). It becomes tall and pointed in the form of a peak instead of the smooth apex of normal.
Functional overload of the right atrium on the ECG can also give an altered P - this is noted, for example, with overactivity of the thyroid gland, tachycardia, etc. Deviation of the heart axis to the right does not always occur only with HPP; it can also be normal in high asthenics. Therefore, other studies are used for differentiation.
If signs of right atrium overload are detected on the ECG, the patient is recommended to undergo echocardiography. It is considered safe for any category of patients and can be repeated many times over time. Modern devices can give answers about the thickness of the heart walls, the volume of the chambers, etc.
Together with echocardiography, the doctor may also prescribe Doppler ultrasound, then you can obtain information about hemodynamics and blood flow.
If there is a divergence of opinions, CT or radiography is prescribed. X-ray examination shows abnormalities of the right atrium and ventricle. Their contours merge with the contours of the vessels. In addition, an x-ray will show the condition of other structures of the chest, which is very valuable in case of pulmonary pathology as the root cause of HPP.
Consequences of GPP
In chronic diseases of the pulmonary system, the active alveoli are replaced by fibrous tissue, and the gas exchange area becomes smaller. Microcirculation is also disrupted, which leads to increased pressure in the pulmonary circulation. The atria have to actively contract, which ultimately causes their hypertrophy.
Thus, the complications and consequences of GPP are:
- expansion of the heart chambers;
- circulatory disorders, first in the small and then in the large circle;
- formation of the pulmonary heart;
- venous congestion and heart valve insufficiency.
If left untreated, pulse irregularities and attacks of heart failure may develop, which can lead to death.
Treatment
Normalizing the size of the atrium and improving the functioning of the heart muscle is only possible if the underlying disease – the cause of the pathology – is treated. Such treatment is always complex; monotherapy does not make sense.
In the presence of pulmonary pathology, these are bronchodilators (tablets and inhalers), antibacterial therapy for bacterial etiology of disorders, anti-inflammatory drugs.
For bronchiectasis, surgical treatment is used.
In case of heart defects, the best solution is corrective surgery. After heart attacks and myocarditis, it is necessary to prevent remodeling with the help of antihypoxic and cardioprotective drugs.
Antihypoxants are indicated: Actovegin, Mildronate, Mexidol and Preductal. Cardioprotectors: ACEs or angiotensin II receptor antagonists (ARA II). They can actually slow down the onset of chronic heart failure. The most commonly prescribed drugs are Enalapril, Quadropril, Perindopril, etc.
Nitrones, beta blockers (Metoprolol, Bisoprolol, Nebivalol, etc.), ACE inhibitors, antiplatelet agents that prevent the formation of blood clots, statins that normalize the amount of cholesterol are required.
Also used in treatment are glycosides (according to indications) and antiarrhythmics, agents that improve metabolic processes in the heart muscle. Judging by the reviews, good results were obtained when prescribing Riboxin.
Atrial flutter - symptoms and treatment
Drug treatment
Drug therapy involves taking drugs that restore sinus rhythm.
The main antiarrhythmic drugs are:
- amiodarone (cordarone);
- sotalol (sotahexal);
- propafenone (ritmonorm);
- verapamil;
- cardiac glycosides.
The combination of these antiarrhythmic drugs increases the effectiveness of treatment.
Amiodarone and sotalol are class III antiarrhythmic drugs.
Amiodarone is most effective in preventing the development of atrial fibrillation, as well as arrhythmia after a heart attack. It has been proven to improve survival in patients with severe circulatory failure. May improve myocardial contractility [5]. Contraindicated in hypo- and hyperthyroidism.
Sotalol, as a means of preventing atrial fibrillation, is less effective than amiodarone. The safest dose of this antiarrhythmic drug for atrial flutter is 120 mg twice a day. But for life-threatening heart rhythm disturbances, the dose of sotalol can reach 640 mg per day. The most common side effects of the drug include symptoms of digestive tract disorders: abdominal pain and diarrhea [5]. Contraindicated in COPD and severe bronchial asthma.
Propafenone is a class I antiarrhythmic drug. Its preventive effect is weaker than that of amiodarone and sotalol. Long-term use of this drug increases the risk of repeated attacks of arrhythmia. It can lead to side effects such as shortness of breath, dizziness, vomiting, changes in taste, constipation, headaches, abdominal pain, blurred vision, ataxia and diarrhea [5].
Verapamil is a class IV antiarrhythmic drug. Its effectiveness is lower than that of amiodarone and sotalol, and fairly high doses are required to prevent flutter attacks. Side effects include a decrease in heart rate to 50 beats per minute, hypotension and progression of heart failure.
Among cardiac glycosides, digoxin is most often used. Typically, this drug is prescribed for a combination of atrial flutter and circulatory failure.
The antiarrhythmic effect of glycosides does not develop immediately: after about two weeks from the start of treatment. Long-term use increases the risk of overdose. Other reasons that increase the risk of overdose include low levels of potassium, magnesium, oxygen and high levels of magnesium in the blood, kidney and liver failure, old age, poor general condition of the body and taking diuretics.
If it is necessary to take diuretics, preference should be given to potassium-sparing diuretics, for example veroshpiron. At the same time as taking diuretics, you need to monitor your heart rhythm [5].
Considering that atrial flutter most often occurs against the background of low potassium levels in the blood, potassium supplements are added to standard drug therapy:
- 4% potassium chloride solution;
- asparkam;
- Panangin.
Among other things, all patients with atrial flutter and fibrillation are advised to take anticoagulants to prevent the formation of blood clots [5][13].
Electropulse therapy
When symptoms of heart failure appear, preference is given to electrical pulse therapy - EIT. It is carried out using a special device - a defibrillator. One of its electrodes is fixed slightly outward from the apex of the heart, the other to the right of the sternum. If atrial flutter is present and the patient is stable, start with a 25 J shock.
After the procedure, the patient must remain in bed during the day. He is prescribed antiarrhythmic and antithrombotic therapy. Atrial function is restored within a few days after the flutter attack has stopped.
If there are no complications, the patient is discharged from the hospital 6-7 days after EIT [5]. In rare cases, complications are possible: systemic embolism, ventricular tachycardia, acute left ventricular failure, ventricular fibrillation, myocardial damage, extrasystole, hypertension, sinus tachycardia and bradycardia.
When atrial flutter is combined with sick sinus syndrome, permanent pacing . This effect on atrial rhythm significantly reduces the risk of developing flutter attacks.
Ablation
With typical atrial flutter, preference is given to ablation - the destruction of pathological electrical foci.
Ablation, which is carried out using high-frequency currents, is called radiofrequency. The destruction of pathological foci using low temperatures, down to −70 °C, is called cryoablation.
In radiofrequency ablation, a catheter is inserted into the atrium through the common femoral or subclavian vein. Using electrical signals sent through the catheter, the doctor finds the arrhythmogenic zone and begins to influence it through the electrode. After this, the doctor re-checks the electrical activity of all chambers of the heart to ensure the effectiveness of the procedure and ends the operation. The effectiveness of this method is 95% [14].
Open heart surgery aimed at isolating the atrium is also possible However, they are difficult to perform and are not performed in patients with severe heart failure.
Relapse Prevention
If drug therapy is the prerogative of the doctor, greater responsibility falls on the patient himself. Without his participation, the efforts of doctors will not produce results. A person must definitely reconsider his lifestyle: give up smoking and alcohol, establish proper nutrition, eliminate physical inactivity, adhere to a daily routine, exercise moderate physical activity, and normalize body weight. If pathologies of the cardiovascular and pulmonary systems become chronic, they cannot be completely cured.
The condition can only be improved by preventing exacerbations of these pathologies. Then the load on the cardiac system decreases.
Eliquis® (apixaban) for non-valvular atrial fibrillation
To date, the only drug with the INN apixaban registered in Russia is Eliquis®. This drug is a direct selective inhibitor of coagulation factor Xa, due to which it interrupts the coagulation cascade and prevents the formation of blood clots.
The superiority of apixaban over warfarin was demonstrated in the double-blind, randomized international clinical trial ARISTOTLE, the results of which were published in 20117. We analyzed data from 18,201 patients with atrial fibrillation and risk of stroke, divided into groups of patients taking INR-guided warfarin or apixaban.
The study results showed that apixaban, compared with warfarin, reduced the risk of stroke by 21%, the risk of major bleeding by 31%, and overall mortality by 11%.
Thus, to date, Eliquis® is the only direct oral anticoagulant that has shown superiority over warfarin in patients with NAF according to three main clinical indicators based on CT results.
In addition, the advantage of apixaban is its favorable safety profile. The drug has low renal excretion (renal excretion 27%), which allows its use in mild to moderate renal impairment8.
Also, Eliquis® at the full therapeutic dose (5 mg twice daily) is suitable for most patients with NFP and does not increase the risk of gastrointestinal bleeding7.
The treatment regimen for the drug on an outpatient basis looks very simple and is easy for the patient to remember: one 5 mg tablet twice a day, regardless of meals. (2.5 mg twice daily if two or more of the following are present: age 80 years or older, body weight 60 kg or less, or plasma creatinine concentration ≥1.5 mg/dL (133 µmol/L) ; or with creatinine clearance 15–29 ml/min).
GPP and pregnancy
During pregnancy, the body undergoes enormous changes not only in terms of hormonal balance, but also in the functioning of internal organs. A difficult situation arises when diagnosing right atrium overload during pregnancy, which in this situation is considered an extragenital disease. The diagnosis must not only be established, but also the woman’s ability to bear a fetus and give birth.
The best option, of course, is to diagnose heart pathologies before conception, but this does not always happen. Most often, pregnant women with heart pathologies are hospitalized three times during gestation; this is done to monitor the condition over time.
When first admitted to the hospital, the defect is examined, the activity of the process is determined and the work of the blood circulation is assessed, taking into account the question of a possible termination of pregnancy.
Repeated hospitalization is necessary because the physiological stress of the body to maintain the functioning of the heart muscle in a woman reaches its peak. The third hospitalization helps doctors choose the method of delivery.
Preventive actions
Prevention of right atrium hypertrophy begins with a review of the lifestyle, which involves proper balanced nutrition and a rational work and rest schedule. If you are not a professional athlete and you do not necessarily need Olympic medals, do not show stubborn fanaticism in playing sports. This exhausts the body and exhausts the heart. The pressure in the circulatory system increases, and hypertrophy will not take long to occur. Daily walks of an hour a day, swimming, and cycling are quite enough.
Another problem is eliminating stress. They also have a very negative impact on the functioning of the heart and the entire body as a whole. Yoga, meditation, and relaxation can help solve the problem.