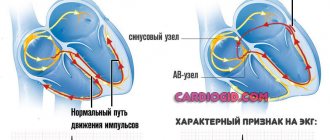
The heart independently generates electrical impulses, and the sinus node (SU) helps it cope with the task. The latter plays the main role. In other words, the SG is part of the conduction system of the heart. It regulates the activity of the myocardium by reproducing impulses. With its dysfunction, the rhythm of the heart muscle changes, its contractions become irregular. The pathology code according to ICD-10 is I49.5. Although adolescents with unexpressed symptoms of sinus node dysfunction may even be drafted into the army, it is important to promptly determine the causes of the pathology in order to prescribe the correct treatment.
general information
Rhythm disturbances also have another name – sick sinus syndrome (SSNS). It is caused by weakening or cessation of the automatic control function. Against the background of the pathology, a violation of impulse formation and conduction from the SG to the atria is noted. The main symptom is bradycardia, a condition in which the myocardial rhythm becomes rarer. The latter causes an increased risk of sudden cardiac arrest in people suffering from CVS.
More often, pathology is observed in the elderly (over 60-70 years old), regardless of gender. Sick sinus syndrome is rarely recorded in children and adolescents. The percentage of distribution is a maximum of 0.05%. In addition to the true disorder, which is provoked by an organic lesion, autonomic sinus node dysfunction (ASD) in children and adults, as well as medication, is noted. Then it is possible to eliminate the violations by drug denervation of the myocardium or the abolition of drugs that provoked inhibition of impulse formation and conduction.
Treatment of sick sinus syndrome
Almost all people with sick sinus syndrome should be treated with a permanent pacemaker.
A pacemaker is a very small machine that is surgically implanted in the chest or abdomen to regulate the heartbeat. This occurs by sending electrical impulses to the heart.
Almost half of pacemaker implantations are performed due to problems related to sinus node dysfunction. Surgery to implant a pacemaker is generally well tolerated by people, and most people experience no complications.
A pacemaker is especially important for people with sick sinus syndrome for two reasons. Firstly , these people have a relatively high risk of fainting (from those long pauses when atrial fibrillation ends). And second , many of the medications that are often used to treat atrial fibrillation—beta blockers, calcium channel blockers, and antiarrhythmic drugs—can significantly worsen sinus node disease.
Improvements in pacemaker technology have contributed significantly to improving the outlook for patients with sinus node dysfunction. Pacemakers provide missing electrical impulses from a faulty sinusoidal node. Pacemakers are not a cure, but they are a very effective treatment for SSSS.
The introduction of a pacemaker will prevent fainting and allow the doctor to treat atrial fibrillation much safer.
Classification
The clinical picture of the disorder may include minor signs or feelings of weakness, palpitations and fainting (Morgagni-Adams-Stokes syndrome). Features of symptoms form the basis for the classification of pathology. However, there are other parameters by which types of SSSU are distinguished - according to the flow, recording signs of disturbance during Holter ECG monitoring (HM).
Based on the nuances of symptoms, the disorder is divided into three forms. They are presented schematically as follows:
| Forms | Options | Description |
| Latent | — | There are no clinical or ECG symptoms. The buildup can only be recognized by electrophysiological tests. There are no work restrictions. Implantation of a cardiac device is not necessary |
| Compensated | Bradysystolic | The symptoms are not obvious, but the patient suffers from weakness and complains of dizziness. There are work restrictions. Implantation of the device is not prescribed |
| Bradytahisystolic | Among the clinical manifestations, paroxysmal tachyarrhythmias are noted. Implantation of a special device may be recommended in cases of decompensation of the cardiovascular system during antiarrhythmic treatment. | |
| Decompensated | Bradysystolic | Characterized by severe bradycardia, symptoms of pathologies of cerebral blood flow (dizziness, fainting), heart failure provoked by bradyarrhythmia. In this case, going to work is prohibited and an implantation operation is performed. |
| Short's syndrome | Paroxysmal tachyarrhythmias are noted with it. Patients are unable to work; recommendations for implantation of a cardiac device are similar | |
| Constant | Tachysystolic | Work ban. But there is no appointment for implantation of the device |
| Bradysystolic | Work is limited. Implantation of a cardiac device is prescribed for cerebral symptoms |
For your information! According to etiology, primary (when the sinoatrial zone has organic lesions) and secondary (due to failures of autonomic regulation) forms are distinguished.
There are several more parameters that can serve as the basis for the classification of SSSU. Cardiologists distinguish two:
- Depending on the recording of symptoms with HM ECG. Development can be latent, when there are no manifestations, or intermittent - they are noticeable when sympathetic tone decreases. If signs of SSSU are detected during daily HM ECG, the development is manifest.
- According to the nature of the disease. Acute development is recorded during a heart attack, and stable or slowly progressive development is also recurrent.
Causes and risk groups
Among exogenous influences, a common cause of pathology is excessive pressure of the parasympathetic nervous system on the pacemaker. In addition, cases of primary SSSU are also identified. The disorder is caused by organic lesions of the sinoatrial zone in the following conditions:
- cardiac pathology;
- idiopathic degenerative and infiltrative diseases;
- hypothyroidism;
- musculoskeletal dystrophy;
- age-related amyloidosis, scleroderma heart;
- malignant neoplasms of the myocardium.
The development of secondary SSSS is provoked by exogenous factors affecting the sinoatrial zone. Among the latter, hyperkalemia, hypercalcemia, and drug therapy are noted, in which the automaticity of the pacemaker decreases. As a rule, this condition is caused by taking b-blockers, clonidine, dopegit, cardiac glycosides.
VDSU occupies a special place. It is often noted against the background of hyperactivation of the paired nerve. As a result, the rhythm slows down and the decrease in excitability of the sinoatrial node prolongs. An increase in tone is observed during physiological processes - sleep, urination, defecation, coughing, swallowing, vomiting. The following conditions can cause pathological activation of the paired nerve:
- diseases of the pharynx, genitourinary and digestive tracts, which have abundant innervation;
- hypothermia;
- hyperkalemia;
- sepsis;
- increased intracranial pressure.
Due to strong neuroticism, autonomic dysfunction is observed in young people. And in athletes, due to the pronounced predominance of the tone of the paired nerve, a rare heart rhythm may be noted. The latter cannot be considered a sign of SSSS, since the increase in heart rate (HR) corresponds to the load.
For your information! Although trained athletes often develop true sick sinoatrial node syndrome due to dystrophy against the background of other pathologies.
Causes of pathology
The most common cause of sinus node dysfunction among external factors is the excessive influence of the parasympathetic nervous system on the sinus node. The parasympathetic system in the body is a section of the nervous system responsible for the functioning of internal organs.
This condition occurs in the following cases:
- under influences traumatic to the nervous system: mechanical, chemical and others;
- with oncological processes developing in the brain;
- during hemorrhage of the subarachnoid type;
- changes and disturbances in the electrolyte composition, which occurs when systematically taking various medications, most often from the groups of adrenergic blockers and cardiac glycosides.
Sinus node dysfunction in children is caused by the following reasons:
- surgical interventions that were caused by congenital pathologies: heart defects, disorders of its individual parts, underdevelopment of valves and blood vessels;
- damage to the nervous system – central and autonomic;
- autoimmune diseases;
- inflammatory processes - myocarditis, occurring in the heart muscles.
The most common reason why the atrial node in children and adolescents ceases to control the heart rhythm is autonomic dysfunction of the sinus node.
Consequences of pathology
Pathology is more common in older people. Although young people, as well as children and adolescents, are diagnosed with the disorder. SSS can cause persistent sinus bradycardia, when the heart rate becomes less than 45 beats per minute. Against the background of the development of pathology, the frequent occurrence of sinus extrasystoles is recorded - the myocardium is blocked for 2-3 seconds.
Dysfunction if left untreated can lead to other consequences. Among them, doctors note:
- Fainting conditions.
- Frequent attacks of tachycardia with unstable restoration of heart rhythm.
- Thromboembolic complications.
- Development of stroke.
- Alternating attacks of fibrillation with slow heart rate.
- Atrial flutter.
Symptoms of sick sinus syndrome
The most noticeable symptoms are usually those associated with a slow heart rate and these include:
- easy fatigue;
- dizziness;
- rapid heartbeat (irregular heart rhythm);
- slow heart rate (bradycardia);
- syncope;
- chest pain;
- sleep disorders;
- memory problems;
- shortness of breath;
- confusion, changes in logical thinking, personality and behavior.
Some people with sick sinus syndrome experience these symptoms only when they try to exert themselves (increase their activity) and feel fine when at rest. In these cases, the main problem is the inability to increase the heart rate appropriately during activity, a condition called "chronotropic incompetence."
Sick sinus syndrome and atrial fibrillation
People with sinus node disease who also have episodes of atrial fibrillation (atrial fibrillation) often experience symptoms caused by sinus bradycardia, and in addition they may have symptoms of tachycardia (increased heart rate), especially rapid heartbeat. People with episodes of both slow and fast heart rates are said to have bradycardia-tachycardia syndrome or "brady-tachy syndrome" (i.e., alternating periods of tachycardia and bradycardia).
The most unpleasant symptom associated with brady-tachy syndrome is fainting. Loss of consciousness usually occurs immediately after the sudden cessation of atrial fibrillation, resulting in a prolonged pause in the heart rate.
This long pause occurs because when the sinus node is already “sick,” an episode of atrial fibrillation tends to further suppress its function. Thus, when atrial fibrillation suddenly stops, it may take a few seconds for the sinus node to “wake up” and begin generating electrical impulses again.
During this interval, there may be no heartbeat for 10 seconds or more, resulting in confusion or fainting.
When to see a doctor?
It is important to see your doctor immediately if you experience the following signs, especially if you have a personal or family history of heart disease. These may be symptoms of a heart attack or early cardiac arrest. Signs to look out for include:
- constant fatigue;
- chest pain;
- labored breathing;
- profuse sweating;
- constant dizziness;
- pain or discomfort in the upper body;
- confusion or panic is common;
- abdominal pain;
- nausea and vomiting;
- frequent fainting.
See your doctor as soon as possible if you experience any of the above symptoms of SSSS.
Symptoms
Patients with the development of pathology experience discomfort due to disturbances in the functioning of the gastrointestinal tract. Dysfunctions are caused by insufficient oxygen supply to organs. Other patients complain of problems with the urinary system: urine is not excreted from the body in the required volume (small quantities). Sufferers of SSSS may notice that the pulse becomes slower and a feeling of “cardiac arrest” occurs.
Clinical manifestations in SSSU concern changes. The latter are summarized in the table:
| Change group | Characteristics of symptoms |
| Are common | Pale and sagging epidermis, coldness in the extremities, loss of muscle tone, lameness when moving |
| Cerebral | Feeling of tinnitus, loss of sensitivity, emotional instability, fainting, memory impairment |
| Heartfelt | Rhythm problems, shortness of breath at rest, chest pain |
With dysfunction of the sinoatrial pacemaker, fainting is observed, which goes away on its own or requires resuscitation. Loss of consciousness can be caused by sudden turns of the head, sneezing; slight or severe cough, clothing tight to the neck (collar, tie). Regular bradycardia is combined with neurological disorders. Among the latter, cardiologists name the following:
- Increased excitability.
- Deterioration of memory.
- Sleep disorders.
- The appearance of problems with speech.
- Weakness.
Diagnostic methods
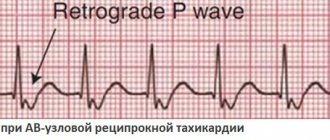
An anamnesis collected at the patient’s first visit and examination results help to make an accurate diagnosis. If the development of SSSS is suspected, an ECG is indicated. It is performed on all patients. However, it provides detailed information in case of severe clinical picture. According to ECG information, the main manifestations of the pathology are sinus bradycardia, cardiac arrest, post-extrasystolic depression, and atrial fibrillation in chronic development.
For your information! Symptoms of bradycardia and tachycardia are characteristic of half of the patients suffering from SSSS.
Holter monitoring
When diagnosing pathology, the most informative type of study is carried out over one to two days. The test makes it possible to determine myocardial pathologies, including other rhythm disturbances. Thanks to the study, it is possible to identify signs characteristic of CVS and evaluate heart rate dynamics. The latter varies greatly among healthy people due to additional influences - state of rest or excitement, time of day, age, gender.
But in general, the following values have been identified: if there are no pathologies of the cardiovascular system and other serious diseases, the average daytime frequency is 80-90 beats/min, at night the indicator is 55-70 beats/min. Significant manifestations of SSSU are moments (for several minutes or more) of bradycardia with a frequency of less than 50 beats/min, and even more reliably – up to 40. Among the disadvantages of this type of monitoring is the inability to determine SSSS due to regulatory dysfunction.
Medication tests
To assess the significance of changes detected on the ECG and exclude VDS, this method is used. There are several types of samples, presented in tabular form:
| Name | Description |
| Atropine test | Effective in determining the VDSU in young patients. The medication is administered intravenously at a rate of 0.02 mg/kg. The picture is evaluated after 3 minutes. If heart rate increases to 90 or more beats/min. or no less than 25%, this is the norm. A negative result is not a reason to exclude pacemaker dysfunction, since injection of the substance does not relieve hypersympathicotonia. To organize a complete blockade of the pacemaker to determine its actual impulses, injections of obsidan 0.1 mg/kg are given alternately intravenously over 5 minutes. or 5 mg orally and 10 minutes later. – atropine. The indicator is calculated as follows: 118.1-(0.57 x age) |
| Isoproterenol | The substance (2-3 mcg/kg) is administered intravenously. The procedure for performing the test, as well as the criteria, are similar to those mentioned above |
| Adenosine triphosphate (ATP) | The test is carried out by quick injection into a vein. ATP has a two-phase effect: in the first two to three seconds it suppresses the automatism of the synovial system and the conduction function, and then stimulates the appearance of reflex tachycardia. The latter is provoked by peripheral vasodilation. Such tests can be performed after atropine administration |
For your information! If a person’s initial heart rate is above 90 beats/min. Initially, there is no point in injecting atropine.
With physical activity
When performing such tests with normal sinoatrial node function, a submaximal heart rate is noted. But this only happens if the test is not stopped due to the development of ischemia, a rise in blood pressure, severe shortness of breath or physical fatigue of the patient, leading to the inability to continue the load. Insufficient increase in heart rate is an indicator of pathology:
- at the first stage – less than 90 beats/min;
- on the second – up to 100;
- on the third and fourth – less than 110-125.
Intracardiac electrophysiological study
Based on its results, it is possible to determine the recovery time of the SA node, which is considered an indicator of its automaticity. The latter will be greater if it takes less time to restore functions. They suppress the operation of the node with pulses of frequent electrical cardiac stimulation. If the time exceeds the values typical for healthy people, we can talk about SSSU. However, the reliability of the study is not higher than 70%. In patients with asymptomatic dysfunction, the test is not advisable.
Prevention
In many cases, sick sinus syndrome cannot be prevented. However, preventing the diseases that lead to sick sinus syndrome (see above) can improve overall cardiovascular health and likely prevent the syndrome.
Eating well, exercising, maintaining a healthy weight, and quitting tobacco can prevent many heart problems. Medicines to prevent heart disease may also help.
Treatment
Therapy for SSSU and the sequence of actions depend on the form of the disease, symptoms and severity of the course. With minimal disturbance, symptomatic treatment and regular monitoring by a cardiologist will suffice. But in some cases, treatment can go as far as implantation of a pacemaker. Absolute indications are:
- Morgagni-Edams-Stokes attack recorded at least once;
- bradycardia;
- dizziness, presyncope, coronary insufficiency, high arterial hypertension;
- development of bradycardia against the background of other types of arrhythmia requiring the prescription of antiarrhythmic drugs, which is impossible in case of conduction disturbances.
If the pathology has moderate manifestations, medications are indicated. The action of the latter should be aimed at eliminating tachy- or bradycardia. But the effectiveness of drug therapy is extremely low. If pathology is noted against the background of an inflammatory process, short-term treatment with corticosteroids is used. But the dosage is high.
Since the appearance of SSSU occurs due to certain reasons, they are eliminated whenever possible. If the factor that provoked the disorder was ischemic myocardial disease, the primary task is to restore blood flow in its vessels. This prevents heart attack. If the reason is related to the use of certain medications, they are gradually withdrawn in order to identify the drug that inhibits the functioning of the systemic system and replace it with a suitable one.
For your information! If the syndrome is caused by a heart defect, and the patient quickly develops cerebral insufficiency at a young age, the cardiologist may recommend surgical intervention.
It is important to eliminate all factors that provoke problems with SU. To achieve the goal, cardiologists recommend:
- Moderately and whenever possible, exercise, which is necessary for a healthy myocardium.
- Stop smoking or reduce the number of cigarettes you smoke per day.
- Eliminate alcoholic drinks from your diet.
- Drink strong tea or coffee, tonics, in small quantities. It is necessary to agree on the dosage with your doctor.
- Monitor the condition of the collar area. Nothing should put pressure on her.
Is autonomic dysfunction of the sinus node dangerous in children?
With pronounced symptoms, the condition requires serious treatment and identification of the causes. If in young children tachycardia is more often caused by stress, then in adolescents this syndrome appears due to the rapid growth of internal organs.
When there are no threatening factors - the heart is normally developed, there is no history of diseases, you should be additionally examined for the presence of infections.
- Streptococci and staphylococci, which are dormant in the body, can significantly influence the occurrence of arrhythmias and provoke inflammatory diseases of the heart and organs with which it interacts.
- With sinus node dysfunction in adolescents, an ectopic rhythm was recorded emanating from the coronary sinus area.
- Bradycardia in infants is caused by impaired cerebral circulation due to intrauterine hypoxia, hypothyroidism is caused by perinatal pathology. Parents notice the child’s abnormal condition by pale skin, poor appetite, and shortened waking time.
- Older children and teenagers experience causeless fatigue and impaired attention.
- If sinus node dysfunction is caused by the body growing up, then you need to wait until the child grows up and the condition stabilizes.
- The most dangerous condition is considered to be when dysfunction of the sinus node leads to frequent occurrence of sinus pauses - the sinus node ceases to stimulate the atria for a sufficiently long period of time. This causes a long-term disturbance of consciousness. At this time, other parts of the heart - the atria and ventricles - take over the production of the heart rhythm, but the restructuring takes time.
- Fortunately, in children this condition occurs only in cases of severe pathologies, in most cases with an overdose or allergy to the effects of medications that support cardiac activity.
Preventive actions
Prevention of the development of SSSS consists of a number of measures that are aimed at identifying and treating dangerous etiological conditions. To prevent disturbances in the work of the pacemaker, take antiarrhythmic drugs that affect automaticity and conduction with caution. To prevent atrial fibrillation in patients with the syndrome, it is necessary to perform cardiac pacing.
For a long time, the indications for “prophylactic” implantation of a pacemaker were unreasonably expanded. The procedure does not increase life expectancy even in patients with severe clinical symptoms of pacemaker dysfunction. But it only eliminates symptoms, primarily syncope. Additional preventive measures:
- Compliance with the principles of balanced nutrition.
- Regular physical activity.
- Elimination of psycho-emotional stress.
- Controlling blood sugar levels.
Do they take you into the army?
At the medical commission at the military registration and enlistment office, the complaints of a young guy can sometimes be ignored. If a young man suspects dysfunction, he should first undergo an examination at a local clinic. Both permanent and temporary health problems can hinder service. And in order to deal with them, the commission may grant a deferment for a second medical examination.
But she doesn’t always make the right decision on her own. The patient should go to the hospital in a timely manner and be constantly monitored by a cardiologist if there are disturbances in the functioning of the myocardium. Then, at the medical examination at the military registration and enlistment office, the conscript will know for sure whether he can serve with a disruption in the functioning of the pacemaker. Negligence and inattention of medical staff can cause serious pathologies in the future. There are many facts when soldiers lost consciousness on the obstacle course and were sent straight from the exercise to the hospital.
If a guy is diagnosed with dysfunction without other disorders, he will still have to serve in the army. But doctors can give a delay in subsequent treatment. A violation against the background of other serious heart pathologies may be exempt from military obligations, since any physical activity can aggravate the young man’s condition and cause irreparable harm to health.
For your information! If the guy is sure that the medical commission ignored the complaints, you need to contact an experienced lawyer and consult with your doctor.
When a conscript is unfit
A young man is exempt from military service if, against the background of dysfunction, he is diagnosed with another myocardial disease. Experts call these:
- ischemic disease;
- failure;
- vice;
- cardiosclerosis;
- mitral valve prolapse;
- IHD;
- cardiac conduction disturbance;
- IVR implantation.
A young man is unfit for service in the event of a surgical intervention that is associated with dysfunction of the cardiovascular system. A young man will not be called up if the health risk is too great. Paroxysmal ventricular therapy with frequent attacks is a reason for refusal to serve. Suitability is determined depending on the type of pathology and the cause of its development. The decision always remains with the commission. But it is important not to delay treatment of the disease, so as not to regret the consequences later, which may be sadder than the fear of serving in the military.
Establishment of suitability category
If a young man has been diagnosed and confirmed with SSSU, then he is assigned category “D” (clause “a” of Article 44). Such a conscript will not be fit for the army. He is given a military ID and is not called up for service. During the examination conducted by the VVC, the severity of angina pectoris and manifestations of heart failure are not taken into account.