© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
When treating a patient with arrhythmia, the doctor must take into account the subtype and characteristics of a particular cardiac arrhythmia. This is due not only to the need for competent emergency care during an attack of tachycardia, but also to the correct determination of indications for surgical treatment in the future, if such a need arises. That is why the emergency doctor, the cardiologist on duty, and the outpatient clinic therapist need to be able to clearly and quickly determine the main criteria for tachycardia on the ECG, and also remember the drugs that can be administered to a patient with this type of arrhythmia. This is especially true for AV nodal tachycardia, or tachycardia from the atrioventricular junction.
What it is?
Atrioventricular nodal reentrant tachycardia (AVNRT) is a variant of supraventricular palpitations. It occurs in the presence of a stable circular wave of impulses in the atrioventricular node and the adjacent septal region of the myocardium. It is registered in approximately 50% of cases. It is worth noting that in practice, compared to other arrhythmias, this type is quite rare. It is more often diagnosed in women under 40 years of age and in older people. Signs of heart damage may be absent.
A high heart rate can provoke a sharp drop in blood pressure and the development of fainting.
Shapes and types
Atrioventricular rhythm occurs:
- Accelerated AV nodal rhythm - contractions per minute within 70 ÷ 130 beats. The disorder occurs as a result of: myocarditis,
- glycoside intoxication,
- rheumatic attack,
- myocardial infarction,
- heart operations.
- negative reaction to taking medications,
AV rhythm occurs in the following manifestations:
- when atrial excitation occurs first,
- the ventricles and atria receive impulses at the same time, and their contraction also occurs at the same time.
Read below about the reasons for the appearance of ectopic and other types of AV nodal rhythm.
Causes and mechanisms of occurrence
Etiological factors are divided into two groups:
- congenital - these include Wolff-Parkinson-White syndrome;
- acquired - diseases suffered by the patient during his life and contributing to the development of reciprocal tachycardia (myocarditis, etc.).
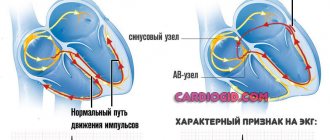
The heartbeat increases in this case due to the presence in the atrioventricular node of two types of electrical impulse conduction, which are interconnected (the phenomenon of longitudinal dissociation of the AV connection). They are called the “fast” or beta path, and the “slow” - alpha path.
A specific start is the occurrence of spontaneous extrasystole (extraordinary contraction of the heart). In this case, the first of the paths should not be ready to receive the signal (refractory state). Thus, AV conduction will be carried out along the alpha beam. Along the “fast” tract that has emerged from rest, the excitation wave travels in the opposite direction and merges with the first one. Subsequently, they circulate in the AV junction, and the re-entry circuit (circular movement of the impulse) is closed.
Basic methods for diagnosing cardiac conduction disorders
1. ECG (electrocardiogram)
A standard 12-lead ECG at rest can identify all the main types of cardiac conduction disorders: sinoatrial and atrioventricular block, bundle branch block. Drug tests in combination with ECG are almost never used at present.
2. Holter monitoring (monitoring) ECG
This type of study allows you to record an ECG for a day or more. It allows you to determine whether the patient has significant pauses (cardiac arrest). Pauses longer than 3 seconds are considered significant. If there are no significant pauses, installation of a pacemaker is almost never indicated.
3. Electrophysiological study of the heart (EPS)
This is the most reliable, but complex and expensive method for diagnosing arrhythmias. EPI is performed only in a hospital and requires the installation of several catheters in the veins of the arms and legs. Electrodes are inserted into the heart through these catheters and cardiac stimulation is performed—arrhythmias are caused and eliminated, and their parameters are examined.
To detect the most common types of cardiac conduction disorders, there is a simpler type of EPI - transesophageal EPI. In this case, a thin wire (probe-electrode) is inserted through the mouth or nose into the esophagus and the left atrium is stimulated through it. This type of study is performed on an outpatient basis. In particular, transesophageal EPI makes it possible to determine how long after cessation of stimulation the function of the sinus node (that is, its own pacemaker) is restored - this is necessary in order to make a diagnosis of sick sinus syndrome, one of the most common types of conduction disorders in the elderly.
Signs on ECG
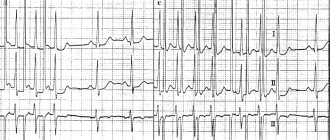
The paroxysm of a typical reciprocal tachycardia is clearly visible on the ECG. Its main differences:
- the presence of a retrograde P wave occurring immediately after the QRS complex;
- absence of P due to its overlap with the QRS;
- heart rate 160-200 beats per minute;
- the presence of the rSr' pseudo-complex in lead V1 (indirect sign).
At the same time, atypical forms of AV nodal reciprocal tachycardia look different on the electrocardiogram.
How does AV reciprocal tachycardia manifest?
An attack of this rhythm disorder is unlikely to go unnoticed by the patient. Usually there is a rapid onset, perhaps after exposure to a provoking factor or against the background of complete well-being. However, the patient suddenly experiences a feeling of rapid, sometimes irregular heartbeat, accompanied by a headache, pain in the heart area, a feeling of lack of air, and a pre-fainting state. Sweating, redness or pallor of the skin, coldness and chilliness of the hands and feet, a feeling of internal trembling, fear of death and other autonomic disorders may be observed.
The attack may go away on its own (more often than not), or it may require emergency medical attention due to extremely poor health and the severe general condition of the patient.
The continuously relapsing form of AV tachycardia is also manifested by a periodically occurring sensation of rapid heartbeat, causing significant discomfort to the patient.
Classification and types
Modern cardiological communities have recognized the division of atrioventricular nodal reciprocal tachycardia into the following 3 types:
- slow-fast - a typical option in which the electrical impulse from the atria through the Aschoff-Tavara node passes along the “slow” path, and back along the “fast” path;
- fast-slow - an atypical form, which is the opposite of the first option;
- slow-slow - a rare type: the current passes through two “slow” beams.
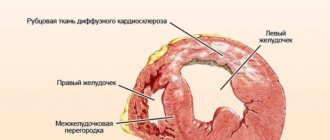
The course of the disease can be paroxysmal (attacking) and chronic. The latter option is rarely observed. Over time, it leads to expansion of the cavities of the heart and the formation of tachycardiomyopathy. Paroxysms, in turn, are characterized by an acute spontaneous onset and the absence of long-term complications.
Wolff-Parkinson-White syndrome (WPU, WPW)
WPW syndrome is caused by the presence of an abnormal bundle of Kent, a connection between the atrium and one of the ventricles. With this pathology, the formation of atrioventricular reciprocal tachycardia through the re-entry mechanism is also possible. There are two types:
- orthodromic - forward along a specialized conduction system, back from the ventricles along an additional atrioventricular connection;
- antidromic - from the atria through the anomalous bundle of Kent and back through the AV node.
Treatment
If sinus bradycardia is observed and the junctional rhythm manifests itself for a short time, then this phenomenon is not treated.
In the case when the rhythm disturbance manifests itself clearly and leads to deterioration of blood circulation, then therapeutic procedures are provided.
Therapeutic
Treatment of rhythm disturbances consists of measures that will convert the atrioventricular rhythm to sinus. They treat major diseases and affect the autonomic system.
- How to decipher an ECG analysis, norms and deviations, pathologies and diagnostic principles
Healthy habits always help with heart health:
- walks in the open air,
- loads should be moderate,
- quitting cigarettes,
- positive thinking.
Medication
The specialist may prescribe medications:
- isoprenaline - used intravenously, combining the drug with a glucose solution or
- atropine – used intravenously.
Medicines may cause unwanted effects:
- angina pectoris
- decrease in pressure,
- ventricular arrhythmias.
If these medications are not suitable for the patient, then the doctor may use aminophylline intravenously or in tablet form instead.
If, before treating atrioventricular rhythm, drugs that could cause rhythm disturbances were used, they should be discontinued. This:
- digitalis preparations,
- guanethidim,
- quinidine,
- antiarrhythmics
- and others.
Operation
In case of rhythm disturbances caused by serious heart disease, measures are required to restore and maintain the correct heart rhythm. To do this, a simple operation is performed to introduce a pacemaker into the patient’s body.
Folk remedies
You can drink infusions and decoctions of herbs. Prescriptions should definitely be discussed with the doctor who is observing the patient.
Recipe No. 1
In a glass of boiling water, infuse herbs and seeds, taken in equal quantities (20 g):
- goldenrod grass,
- flaxseed (ground),
- motherwort grass,
- valerian root,
- viburnum shoots.
The infusion is drunk in small sips for a month.
- Heart scintigraphy in Moscow
Recipe No. 2
Prepare an infusion with components taken in equal quantities (40 g), mixing them with a glass of boiling water:
- lemon balm,
- motherwort grass,
- buckwheat flowers,
- goldenrod grass.
The decoction is drunk in small sips for fourteen days. After a week's break, repeat taking the herbal infusion the same way as the first time.
Expert advice: how to treat
To reduce the heart rate at home, I allow vagal tests to be used independently. For example, you can use one of the following recommendations:
- strain at the height of inspiration (Valsalva method);
- press on the eyeballs (Aschner);
- massage the area of the carotid sinus (anterolateral parts of the neck at the level of the thyroid cartilage).
These methods make it possible to reduce the heart rate, and in some cases even stop an attack of nodal reciprocal tachycardia.
Of the pharmacological agents, the drugs of choice are ATP or Isoptin. The route of administration is intravenous. To prevent paroxysms, I use the following antiarrhythmic medications:
- retard (long-acting) forms of "Verapamil";
- "Allapinin";
- "Etatsizin";
- "Propaphenone".
I often recommend surgical intervention to my patients, which consists of catheter ablation (destruction by electric current) of the “slow” pathway of the atrioventricular node. Cure occurs in 95% of patients. But I want to warn that in 0.5% of cases, a serious complication develops during the operation - persistent AV block of the II-III degree. It requires the installation of a pacemaker.
Atrioventricular nodal reentrant tachycardia (AVNRT)
Atrioventricular nodal reentry tachycardia (AVNRT) is a supraventricular tachyarrhythmia with a re-entry mechanism using the approaches to the atrioventricular (AV) node and the compact AV node. Pulse with tachycardia is usually in the range of 140-250 beats/min.
Epidemiology
AVNRT is the most common form of supraventricular tachyarrhythmia (SVT) and is not usually associated with structural heart disease.
Prevalence
Approximately 70% of patients with AVNRT are women. In women, AVNRT first begins to manifest at a younger age (29±16 years) than in men (39±16 years). Concomitant organic heart disease exists in only approximately 15% of cases.
The reasons why AVNRT occurs more often in women than in men are unclear. Cabrera JA et al (1998) observed anatomical features of the heart structure (wide coronary sinus, which takes on a funnel-shaped shape during venographic studies) in patients with AVNRT.
Classification and mechanisms
Schematic representation of the mechanism of formation of AVNRT.
AV nodal conduction is functionally divided into fast and slow pathways with different electrophysiological properties. The different electrophysiological properties of the two groups of fibers in this area are the basis for the formation of re-entry of excitation (re-entry) and the existence of tachycardia. With an extraordinary contraction of the atria (for example, with an atrial extrasystole), a conduction block occurs in the fast part and the impulse is conducted through the His bundle to the ventricles through the slow channel, and through the fast channel conduction goes back to the atria, and then again to the “slow” part. Thus, a re-entry loop is formed, which underlies AVNRT.
There are three main forms of AVNRT. Typical AVNRT uses a slow anterograde pathway and a fast retrograde pathway (slow-fast, or slow-fast type). Rare forms are fast-slow (fast-slow type) and slow-slow (slow-slow type) AVNRT.
+More details about the mechanisms of AVNRT for specialists At first it was believed that the re-entry circle was limited to the compact part of the atrioventricular node, but later evidence appeared that the perinodal atrial tissue is an integral part of the re-entry loop. However, it has been shown that AVNRT can exist without the participation of atrial tissue. For AVNRT to occur, two functionally and anatomically different channels are required. In most cases, the fast pathway is located near the apex of Koch's triangle. The slow pathway is located posterior and inferior to the pars compacta of the RV and runs along the septal edge of the tricuspid valve annulus at or just above the coronary sinus. Reentry circle diagram for typical AV nodal reentrant tachycardia
During a typical AVNRT, the slow pathway acts as the antegrade leg of the loop, while the fast pathway is the retrograde leg (i.e., slow-fast re-entry of the atrioventricular node). The slow channel impulse is conducted through the His bundle to the ventricles, and the fast channel conduction goes back to the atria, resulting in a P wave of 40 ms duration, which is superimposed on the QRS complex or occurs immediately after it (less than 70 ms), which often leads to to the appearance of pseudo-r' in lead V1.
In rare cases (5-10%), the tachycardia loop has the opposite direction, i.e. conduction occurs antegrade through the fast channel and retrograde through the slow channel (fast-slow re-entry of the atrioventricular node, or atypical AVNRT), leading to the appearance of a long RP interval. The P wave, negative in leads III and aVF, is recorded before the QRS. There are rare cases when both sections of the tachycardia circle consist of slowly conducting tissue (slow-slow re-entry of the RV), the P´ wave is recorded after the QRS (i.e., the RP interval is greater than or equal to 70 ms).
Clinic AVURT
The disease occurs in the form of attacks of frequent rhythmic heartbeat, which begins and stops suddenly. The duration of AVNRT paroxysm is from several seconds to several hours, and the frequency of their occurrence is from daily attacks of arrhythmia to 1-2 times a year. Pulse with tachycardia is usually in the range of 140-250 beats/min. An attack of AVNRT is accompanied by palpitations, dizziness, and pulsation in the neck.
Diagnostics
Electrocardiogram of patient N. during an attack of a typical AVNRT. Heart rate 170/min.
12-lead electrocardiography (ECG) can diagnose AVNRT. With normal sinus rhythm, as a rule, no changes are detected on the ECG. During a typical AVNRT attack, the ECG shows tachycardia with a ventricular rate of 140 to 250 per minute. A retrograde P wave of 40 ms duration superimposes or occurs immediately after the QRS complex (less than 70 ms), often resulting in a pseudo-r' in lead V1.
Conducting an electrophysiological study in modern cardiology is an absolute indication in patients with AVNRT.
Treatment of an attack of tachyarrhythmia during AVNRT
The attack can be effectively stopped by performing reflex techniques (Valsalva maneuver, massage of the carotid sinuses). Among the pharmacological agents, the drugs of choice are verapamil, adenosine, obzidan, and novocainamide. Medicines can be prescribed either orally or parenterally.
Treatment AVNRT
Areas of influence on the slow (α) pathways of the AV junction and the effectiveness of arrhythmia elimination in various perinodal areas.
Today, radiofrequency catheter ablation (RFA)
AVNRT is the most effective method of treating this arrhythmia, which allows the patient to completely stop taking antiarrhythmic drugs.
The effectiveness of RFA AVNRT is 98-99%. Complications
in the form of the development of high-degree AV block when modifying the slow part using RFA occurs in 1%.
It is based on the destruction of the fibers of the “slow” part in the lower part of Koch’s triangle. RFA AVNRT is an absolute indication in patients suffering from this arrhythmia. A contraindication
to this operation is the patient’s preference for ongoing antiarrhythmic therapy.
A number of antiarrhythmic drugs can be used to treat patients with frequent and persistent attacks of AVNRT who prefer continuous oral therapy and refuse catheter ablation. Standard therapy includes calcium channel blockers, beta blockers, and digoxin. When treating patients without structural myocardial pathology who are resistant to drugs that slow down AV conduction, preference is given to class Ic antiarrhythmic drugs - flecainide and propafenone. In most cases, class III drugs such as sotalol or amiodarone are not used. Class Ia drugs - quinidine, procainamide and disopyramide - are used to a limited extent because they require a long-term prescription regimen, have moderate effectiveness and have a proarrhythmogenic effect. Source: Revishvili A.Sh. In the book: Bockeria L.A., Golukhova E.Z. (ed.) Clinical cardiology: diagnosis and treatment. M.: Publishing house NTsSSKh im. A.N. Bakuleva; 2011
Case from practice
A 42-year-old woman came to me with complaints of a strong heartbeat and a growing feeling of fear.
This was the first time she had symptoms. An urgent electrocardiogram showed the presence of a heart rate of up to 190 beats per minute, intermittent P waves in leads II, III and AvF. ECG changes indicated an atypical variant of AV nodal tachycardia. The patient received Adenosine intravenously, after which the paroxysm was successfully stopped. She refused planned surgical treatment, and therefore she was recommended to take prophylactic Verapamil.
If you want to know everything about tachycardia, we recommend watching the video below at the link. Causes, symptoms, diagnosis and signs that it’s time to see a doctor - talk about all this in 7 minutes. Enjoy watching!
Characteristic symptoms
Junctional tachycardia is a disease that is accompanied by unpleasant symptoms that significantly impair a person’s quality of life. The main symptom of the disease is a feeling of heart fluttering. In addition, a person is observed:
- lack of air;
- discomfort in the chest area;
- dizziness;
- pain in the heart;
- severe weakness and decreased performance.
In the nodal form of tachycardia, if you tense your abdominal muscles and hold your breath for a while, the heartbeat slows down.
In severe cases, the disease leads to loss of consciousness and attacks of suffocation.