Cardio website
The medical portal 03online.com
provides medical consultations via correspondence with doctors on the website. Here you get answers from real practitioners in your field. At the moment, on the site you can get a consultation in 45 areas: an allergist, venereologist, gastroenterologist, hematologist, genetics, gynecologist, homeopath, dermatologist, children's gynecologist, children's neurologist, children's surgeon, children's endocrinologist, nutritionist, immunologist, cardiologist, cardiologist, cosmetologist, cosmetologist, cosmetologist speech therapist, ENT specialist, mammologist, medical lawyer, narcologist, neurologist, neurosurgeon, nephrologist, oncologist, urologist, orthopedist-traumatologist, ophthalmologist, pediatrician, plastic surgeon, proctologist, psychiatrist, psychologist, pulmonologist, rheumatologist, sexologist-andrologist , dentist, urologist, pharmacist, herbalist, phlebologist, surgeon, endocrinologist.
We answer 95.63% of questions.
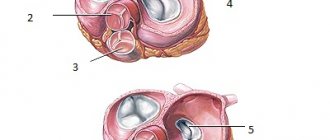
The valve apparatus of the heart is a formation in the form of leaflets that create conditions for the correct direction of blood flow between the chambers of the heart. At the required moment, under the influence of cardiac pressure, they open and close, which prevents the reverse direction of blood flow. Heart valves have a certain structure, shape and size.
INFECTIOUS ENDOCARDITIS: diagnosis, clinical course, treatment
Infective endocarditis (IE) is a serious disease with a high mortality rate. Without treatment, the mortality rate for IE is 100%. In recent years, there has been a significant increase in the number of patients with endocarditis in our country and abroad
Infective endocarditis (IE) is a serious disease with a high mortality rate. Without treatment, the mortality rate for IE is 100%. In recent years, there has been a significant increase in the number of patients with endocarditis in our country and abroad. According to various authors, today the incidence has increased in the elderly and senile, as well as among people under 30 years of age who use intravenous drugs [1, 2].
It is known that IE is a disease of an infectious nature with the primary localization of the pathogen on the heart valves and parietal endocardium, occurring with manifestations of systemic infection, vascular complications and an immune reaction [3, 4, 5].
Traditionally, the development of IE is associated with the presence of “intracardiac” risk factors, which include congenital and acquired heart defects, the presence of prosthetic valves, valve prolapse and other anomalies [6]. In recent years, patients with focal infection, as well as people who have had invasive research methods, including the installation of a subclavian catheter, have been classified as high-risk individuals [7]. A special risk group consists of drug addicts who practice intravenous drug administration, in whom IE occurs with damage to intact heart valves.
This paper summarizes the experience of diagnosing and managing patients with IE on the basis of the general therapeutic department of the Alexandrovskaya Hospital in St. Petersburg for the period 1998–2003. Diagnosis of the disease was carried out in accordance with Duke criteria [8]. The diagnosis of IE was assessed as reliable if two main criteria were present, namely:
We examined 105 patients with IE, of which in 80 people aged 18 to 30 years (first group), the main risk factor for the disease was injection drug addiction.
In the second group of patients (25 people), the main predisposing factors for the development of IE were congenital and acquired heart defects, as well as prosthetic valves.
In people of the older age group, an additional risk factor was degenerative-dystrophic changes in the heart valves.
The relationship between the nature of heart valve damage and risk factors for IE is presented in Table 1.
According to an echocardiographic study, 100% of patients in the first group had mobile vegetations on the leaflets of the tricuspid valve (TV), which was accompanied by the formation of its insufficiency of degrees I-III.
How does the heart apparatus work?
How many chambers are there in the human heart? How is blood circulation carried out?
A blood mass depleted of oxygen comes to the right atrium through the superior and inferior vena cava. When this section is compressed, blood passes into the right ventricle through the atrioventricular valve. After filling has occurred, the blood mass enters the pulmonary vessel and flows into the pulmonary circulation.
The pulmonary circulation is located in the pulmonary apparatus, which saturates the blood mass with oxygen molecules. Oxygenated blood travels through the pulmonary veins to the left atrium. After it is filled, blood flows through the mitral valve into the left ventricle, which then pushes it under pressure into the aorta. Next, the blood mass enters the systemic circulation and carries oxygen molecules to all organs.
Tingling in the heart area: causes and methods of relief.
What is cholesterol and is it different from cholesterol? Read about it here.
Heart valves
How many valves are there in the human heart?
A healthy human heart has four valves that function like gates: they open to let blood flow in and close to prevent it from flowing back out.
- left atrioventricular;
- tricuspid;
- aortic;
- pulmonary valve.
Left atrioventricular
The mitral valve plays an important role in the functioning of the heart and has the following components:
- atrioventricular ring made of connective tissue;
- valves and muscular apparatus;
- chords of tendons and ligaments.
The mitral heart valve connects the left atrium and the left ventricle. It consists of two valves: aortic and mitral. The number of valves may vary for each person, which is considered normal. According to research, most of half the population has two valves, while the rest may have three to five.
How does it function?
When it opens, blood is released through the atrioventricular passage from the left atrium into the left ventricle. During systolic contraction of the ventricle, the cardiac element closes. This is a very important point that will prevent blood from returning to the atrium. Next, the blood flow penetrates into the aorta, and from it into the hemodynamic channel of a large circle of the circulatory system.
Tricuspid
It connects the right atrium and the right ventricle and consists, respectively, of three triangular cusps (anterior, posterior and intermediate). In children, additional valves may be observed, which transform and disappear over time.
Aortic valve
Normally, the AC consists of three crescents. In 0.5% of the population, a congenital bicuspid valve is found, which is prone to degenerative changes with the development of combined aortic disease in the form of regurgitation and stenosis. In addition, these people have an increased risk of aortic dissection. A bicuspid valve can be diagnosed during a routine echocardiogram. In elderly patients, as well as with long-term arterial hypertension, focal sclerotic changes in the AV often occur without significant obstruction. Minimal aortic regurgitation is also common, especially in old age.
Aortic stenosis is the most common severe valvular heart disease in the European population and is an indication for surgical treatment. The disease begins with focal sclerosis, which, spreading, leads to severe thickening, calcification and immobility of the aortic semilunar cusps. These changes are well recognized by echocardiography. The presence of even mild aortic stenosis, in which only a slight acceleration of blood flow is noted (the maximum speed of 65% is a sign of severe regurgitation);
- calculation of the half-life of the pressure gradient between the aorta and the LV from the flow of aortic regurgitation recorded in continuous wave Doppler mode (a half-life of the pressure gradient of 16 cm/s indicates severe regurgitation.
An important part of the examination of patients with moderate and severe aortic regurgitation is the assessment of LV function (size and EF) and the diameter of the ascending aorta.
Signs of damage to the aortic valve in infective endocarditis are vegetation, newly emerging aortic regurgitation, structural defects of the semilunar valves and the transition of the process to perivalvular tissue with the formation of para-aortic abscesses and fistulas (for example, between the aortic root and left atrium). Such complications are especially well recognized during transesophageal examination.
Tricuspid valve
Primary lesions of the TC occur relatively rarely. An exception is infective endocarditis, which occurs mainly in drug addicts and patients with long-term central venous catheters installed. Endocarditis that occurs in patients with implanted pacemakers can also spread to the TC. Other causes of organic lesions of the breast include rheumatic disease, carcinoid syndrome, iatrogenic damage (for example, during pancreatic biopsy) and others (“Ebstein’s anomaly”).
TC stenosis is very rare and, as a rule, accompanies rheumatic MV lesions. An average gradient across the TC of >5 mm Hg is considered clinically significant. (measured in continuous wave Doppler mode).
Valvular or mild regurgitation on the TC is almost always present; it should not be considered a pathology. Except in patients with implanted pacemakers or defibrillators or current infective endocarditis, moderate to severe tricuspid regurgitation almost always occurs due to RV dilatation, the most common cause of which is pulmonary hypertension. It is also necessary to remember the causes of functional (relative) tricuspid regurgitation, such as AF, left-right shunt, or RV diseases, such as RV MI or cardiomyopathy.
Severe tricuspid regurgitation is indicated by a large proximal convergence zone, a large width of the base of the regurgitant jet (vena contracta), a dilated inferior vena cava that does not collapse on inspiration, and reverse systolic blood flow in the hepatic veins. The maximum flow velocity of tricuspid regurgitation is used to calculate the maximum systolic pressure in the RV, and therefore in the PA. Since the gradient determined by the simplified Bernoulli equation is the difference between the maximum RV and RA systolic pressures, the RA systolic pressure must be added to this gradient to calculate the absolute RV (or PA) pressure. This value is either taken as a constant (usually 10 mmHg) or calculated taking into account the filling of the jugular veins, respiratory changes in the diameter of the inferior vena cava, or the nature of blood flow in the hepatic veins. However, in many echocardiography rooms, the report reflects only the value of the maximum pressure gradient of tricuspid regurgitation.
Pulmonary valve
The PA valve cannot be assessed in detail either with transthoracic or transesophageal echocardiography. Pulmonary stenosis is almost always congenital and can be represented by subvalvular, valvular and supravalvular variants as part of complex congenital defects, for example, tetralogy of Fallot. Minimal pulmonary regurgitation is almost always present even in apparently healthy people. The degree of more serious pulmonary regurgitation is assessed on the basis of such signs as the severity of RV dilatation, shortening of the half-life of the pressure gradient of the regurgitant flow in continuous-wave Doppler mode (half-life of the pressure gradient of 4 m/s. The cause may be an increase in pressure - a phenomenon caused by a local high gradient pressure that occurs in these grafts due to their design. This pressure gradient is measured with continuous wave Doppler, but is higher than the true gradient between the LV and the ascending aorta, which leads to an overestimation of the measured gradient. Unfortunately, a high transvalvular pressure gradient caused by dysfunction (e.g. pannus or thrombosis) is no different from a high pressure gradient caused by valve design. These two gradients are not always additive, since in the case of obstruction the pressure gradient caused by the design of the prosthesis may even be reduced. Thus, For bicuspid valves (as well as other mechanical valves) in the aortic position with a high transvalvular gradient, it is necessary to either compare with the early postoperative gradient (when the prosthesis was presumably intact) or perform fluoroscopy or cardiac CT to accurately assess leaflet mobility.
Description
All heart valves are covered with endothelium. The three layers that form the basis of the valve apparatus have specific characteristics and are called fibrosa, spongiosa and ventricularis. During heart contractions, spongiosa, rich in glycosaminoglycans, facilitates the process of rearrangement of collagen and elastic fibers.
Vacular interstitial cells (VICs) are abundant in all layers of heart valves and contain a variety of dynamically targeted components. The regulation of collagen and other structural components is provided by enzymes synthesized by VIC. The integrity of valve tissue is maintained by the interaction of valve endothelial cells (VECs) with the VIC. Changes and remodeling of the valvular interstitial and endothelial structure contribute to disruption of the valve properties, and subsequently valve function.
Basics of proper operation of the valve apparatus:
- The valves are properly formed and flexible.
- The valves open completely, allowing the required amount of blood to pass freely through the opening.
- The valves close tightly, then blood does not flow back
Diagnosis and treatment
If you or your loved ones are experiencing the symptoms described above, we recommend getting tested. During diagnosis, the doctor monitors heart parameters at rest and during exercise.
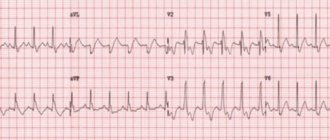
daily ECG monitoring,
chest x-ray,
CT and MRI using special equipment that allows you to examine the heart virtually between beats.
Such diagnostics are carried out not only during the initial examination of patients with suspected disease, but also in dispensary groups of patients with an already confirmed diagnosis.
Depending on the diagnostic results, the doctor prescribes the necessary treatment: therapy or surgery.
Therapy is aimed at preventing, preventing and alleviating relapses of the disease that became the root cause of the defect, as well as treating heart failure.
Surgical intervention is an extreme necessity, which due to age or complications may not be prescribed for all patients.
Typically, heart valve disease is a mechanical problem that can only be solved with surgery performed by a surgeon.
For stenosis, an operation is indicated to separate the fused valve leaflets and widen the atrioventricular opening - commissurotomy. If there is insufficiency, prosthetics are performed: replacement with a biological or mechanical analogue.
Mitral valve
The mitral valve was named after the mitre by Andreas Vesalius (De Humani Corporis Fabrica, 1543). This valve is located at the junction of the left atrium and the left ventricle. Its structure consists of five functional components:
- doors;
- annular space;
- chordae tendineae;
- papillary muscles;
- nearby myocardium.
The annulus fibrosus is an area of connective tissue containing discontinuous fibrous and muscle fibers that connect to the left atrium and ventricle. The anterior valve covers about one-third of the primary fibrous anterior part of the ring. Part of the anterior leaflet of the mitral valve is located in close proximity to the annular opening of the aortic valve. The ventricular, posterior, leaflet is attached to the posterior muscular half and two-thirds of the annular space. Due to the asymmetrical leaflets, the opening of the mitral valve is shaped like a funnel.
Chords from both the anterior and posterior papillary muscles are attached to each valve. The papillary muscles contract and extend the chordae during systole, which in turn promotes the closure of the mitral valve leaflets.
The mitral valve complex is separately distinguished, including the mitral valve and the left atrioventricular myocardium, endocardium and part of the aorta. This formation promotes the outflow of blood from the left ventricle. The forced passage of blood through the valve, as well as its tight closure during systole, is ensured by the coordination of the actions of the mitral-valve complex.
Associated diseases: mitral valve prolapse, mitral valve regurgitation, mitral valve stenosis.
Heart valves
The ability to assess valvular heart defects is one of the most important advantages of EchoCG. The following morphological changes of the valves can be identified: pathological thickening, calcification, space-occupying lesions (eg, fibroelastoma), excessive or limited leaflet mobility, functional integrity, and congenital anomalies (eg, bicuspid aortic valve). With infective endocarditis, new mobile formations attached to the valves (vegetations) can be found, as well as paravalvular abscesses, especially with a valve prosthesis. More long-term consequences of endocarditis are fistulas, leaflet perforations, and the formation of mitral pseudoaneurysms.
Pulmonary valve
Also known as the pulmonary valve. The structure of the pulmonary valve is similar to that of the aortic valve. The valves have a semilunar shape; normally there are three of them (anterior, left and right). Similar to the valves, the sinuses are called sinuses, which are united with the pulmonary trunk through an arched ring (sinotobular junction). Like other valves, the pulmonary valve also has a fibrous ring and a commissure.
Associated diseases: pulmonary valve stenosis, pulmonary valve regurgitation.
Tricuspid valve
Also known as the tricuspid valve. Located in the right half of the heart at the junction of the atrium and ventricle. Consists of 3 valves, chordae tendons (anterior, posterior) and the often identified third papillary muscle. The tricuspid valve does not have a clearly defined collagen ring. The three flaps are attached to an elliptical shaped fibrous ring. The direct attachment of the cuspid septum is a hallmark of the tricuspid valve. Prominent papillary muscles support the valves in the commissures.
Normal valve function requires structural integrity and coordinated interactions between multiple anatomical components. Various pathophysiological mechanisms can cause heart valve disease.
Associated diseases: tricuspid atresia, tricuspid regurgitation, tricuspid stenosis.
Prevention
To prevent illness, we recommend that you first take care of your health and body. Acquired heart valve defects also occur due to infections, so preventive measures should be taken.
Normalize your diet so that you get enough proteins, carbohydrates and fats in your diet. To do this, we recommend consuming mainly vegetables, fruits, cereals and lean fish.
Play sports, but adequately assess your capabilities. For diseases of the cardiovascular system, healthy walking is recommended, not running marathons.
Keep your blood pressure constant: no higher than 140 for systolic and 90 for diastolic. Keep a diary where you record your blood pressure every morning and evening, and try to avoid stressful situations. Frequent anxiety can cause arrhythmia.
These are all general tips for prevention. Only your doctor can choose what is right for you.
If you or your loved ones have suffered a serious illness or have symptoms of heart valve disease, be sure to consult a doctor.
The Chernaya Rechka Heart Medicine Center employs professional cardiologists who act in accordance with national and international clinical guidelines. We will perform a heart examination using modern diagnostic equipment, prescribe adequate treatment for heart disease, and also advise if surgical treatment is required. After the operation, if necessary, we will conduct a course of specialized cardiac rehabilitation.
Pay close attention to your health and don’t get sick!
Source
Heart sounds
The valve apparatus is directly involved in the formation of heart sounds, and when it changes, various types of noise can be formed.
If, for example, the valve does not close completely, then the blood returns to the previous chamber, creating a characteristic noise (for example, the systolic murmur of mitral regurgitation).
When the valves are stenotic (narrowed), blood flow is more difficult to pass through the opening, causing murmurs with other features (for example, diastolic murmur with tricuspid stenosis).
- First heart sound
It occurs due to the closure of the valves of the atrioventricular location (mitral and tricuspid). It begins with the onset of ventricular systole and is best heard in the auscultation region of the apex of the heart.
When determining additional sound components, the presence of vibrations of blood in the ventricular chambers, vibration of the chamber walls, or turbulent flow of blood ejected through the aortic opening into the sinus of Valsalva is assumed.
- Second heart sound
Its appearance is associated with the closure of the aortic and pulmonary valves, as well as with blood fluctuations in the aorta
Because the closure of the right and left semilunar valves does not occur simultaneously, the second heart sound is most often divided into two.
- Third heart sound
It is formed in the early diastole phase and is associated with the rapid filling of the ventricles with blood immediately after isometric relaxation. Sometimes this sound is heard by small children, but usually it is not perceived by the ear.
- Fourth heart sound
Occurs against the background of atrial contraction at the beginning of the cardiac cycle. In most cases, it cannot be heard with a stethoscope.
Thus, during auscultation, only the first and second tones can be clearly heard, which, depending on the place of auscultation, are heard differently. If a phonocardiogram is done, then you can clearly trace the severity of the tone and its correspondence to systole or diastole.
Similar articles
Electrocardiography is the main method for studying the electrical activity of the heart. Many heart diseases are determined using an ECG, which is considered the most accessible diagnostic method. To obtain accurate results, electrodes must be correctly applied during ECG recording.
Timely diagnosis plays an important role in the diagnosis of cardiovascular diseases. Often it is enough to conduct a standard ECG to make the correct diagnosis. In other cases, a diverse examination of the heart is required, which makes it possible to establish the exact cause of the disease and carry out effective treatment.
Tens of thousands of pacemaker implantations are performed annually. In some cases, they are installed only temporarily; for other indications, the device is used on an ongoing basis. In both options, the main purpose of using a heart stimulator is to improve a person’s quality of life.
Causes and symptoms
Heart valve defects can be congenital or acquired. The main causes of the development of heart valve defects are rheumatism, infections, myocardial and cardiovascular diseases.
Congenital heart valve defects develop before birth and depend on how the pregnancy progressed. Congenital heart valve defects are an extremely rare diagnosis, diagnosed only in 1% of cases. Congenital defects include defects of the aortic and pulmonary valves, which are treated by surgical intervention in the first years of the patient’s life.
Purchased . Acquired heart valve defects include transformations of the valve structure due to infections, inflammation, previous heart attacks, etc. Most of them arise as a result of a gradual change in the structure of the heart; in some cases, rheumatism leads to the defect.
All congenital and acquired defects have related symptoms that can appear at any age:
other manifestations of heart failure.
Initially, they appear during physical activity, but as pathologies develop, they will begin to appear in a calm state.
Among the types of heart valve defects, mitral valve prolapse is the most common. It occurs during heart contractions when the valve leaflets in the left atrium sag. The walls of the valve lose elasticity and it “leaks”.
Prolapse can be primary or secondary:
Primary prolapse refers to congenital valve defects. Connective tissue pathologies in this case are a genetic predisposition.
Secondary prolapse is an acquired defect. It occurs due to chest injury, rheumatism or myocardial infarction.
Prolapse does not have serious health consequences, and its symptoms do not interfere with life. However, they may not appear for a long time and most often bother people in old age, which is why they are written off as “age-related.” If you do not pay attention to the symptoms in time, complications may arise, such as arrhythmia and heart failure.
Symptoms also include complaints of pain in the heart area. They arise against the background of anxiety, are not associated with physical activity and are not relieved with medication. The pain is not intense, but long-lasting, accompanied by anxiety and rapid heartbeat.