Clinic of mitral valve lesions
Severe mitral stenosis leads to severe shortness of breath, which sharply reduces exercise tolerance.
Left atrial pressure almost always exceeds 25 mmHg. Art., the course of the disease is complicated by pulmonary hypertension, atrial fibrillation, thromboembolic syndrome. Atrial fibrillation: occurs with hemodynamically significant mitral stenosis in 80% of cases and can lead to a sharp deterioration of the condition as a result of a sudden increase in left atrial pressure and pulmonary edema. Thromboembolism of the arteries of the great circle occurs in 20% of cases, 80% of such patients have atrial fibrillation. Embolisms are multiple, repeated in 25% of cases; in half of the cases, cerebral artery embolism occurs. With severe pulmonary hypertension (more than 50 - 60 mmHg), survival rate is less than 3 years.
Publications in the media
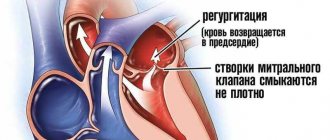
Mitral stenosis (MS) is a narrowing of the left atrioventricular orifice, which prevents the physiological flow of blood from it into the left atrium during systole of the left atrium.
Frequency. 0.05–0.08% of the population. In 90% of cases of all acquired heart defects, damage to the mitral valve is detected, 40% of mitral stenoses are isolated. The predominant age is 40–60 years. The predominant gender is female (2:1–3:1).
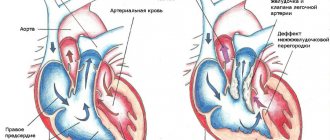
Etiology • The vast majority of cases (more than 95%) are of rheumatic etiology • A clear rheumatic history can be collected in 50–60% of patients • Almost always debuting before the age of 20 years, after 10–30 years the defect becomes clinically evident • Non-rheumatic cases of the defect include severe calcification of the leaflets and mitral valve rings, congenital anomalies (for example, Lutembashe syndrome - 0.4% of all congenital heart diseases), neoplasms and thrombi in the mitral valve and left atrium, massive vegetations on the mitral valve with infective endocarditis, restenosis after mitral commissurotomy or implantation of prostheses into the mitral position.
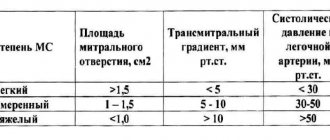
Pathophysiology • The normal area of the mitral orifice is 4-6 cm2 • Narrowing of the left AV orifice impedes the flow of blood from the left atrium to the left ventricle • Diastolic volume and pressure in the left atrium increase (usually in the range of 15-20 mmHg), an increased transmitral gradient occurs (usually within 10–15 mm Hg) • This leads to hyperfunction of the left atrium, its hypertrophy and tonogenic dilatation • The left atrium is a weak part of the heart, and the period of compensation for MS does not last long: the pressure in the heart increases even more left atrium, and then - at the mouths of the pulmonary veins, which leads to passive venous pulmonary hypertension, as well as active hypertension in the pulmonary circulation due to the prolonged Kitaev reflex (spasm of the arterioles of the pulmonary circulation in response to increased pressure at the mouth of the pulmonary veins) • Difficult work of the right ventricle, its hyperfunction, hypertrophy develop, myogenic dilatation, relative tricuspid valve insufficiency and congestion in the veins of the systemic circulation develop quite quickly • Supraventricular tachyarrhythmias are often observed • There are four degrees of MS: minor (mitral orifice area [MO] is more than 3, 0 cm2), moderate (MO area - 2.3-2.9 cm2), pronounced (MO area - 1.7-2.2 cm2) and critical (MO area - 1.0-1.6 cm2).
Clinical picture and diagnosis
• Complaints •• Increased fatigue (20% of all cases) • Interruptions in the work of the heart • Dyspnea (occurs when the area of the heart muscle narrows to less than 2.0 cm2) or cardiac asthma (the most sensitive symptom) • Cough, hemoptysis (the most specific symptom found in 10% of patients) • Ortner's syndrome - hoarseness • History of rheumatic attacks and systemic emboli (20% of all patients and 80% of patients with atrial fibrillation, of which 25% are multiple and repeated) • Angina occurs in 10–15% of cases ( causes - concomitant coronary atherosclerosis, coronary artery embolism, subendocardial ischemia with severe pulmonary hypertension).
• Symptoms associated with enlargement of the left atrium •• Cassio's symptom - delay of the first tone after the apical impulse •• Nesterov's symptom, or two hammers - palpable alternating impulses of the left atrium and left ventricle •• Popov's symptom - reduced filling of the pulse in the arteries of the left upper limb •• Botkin-I symptom - visual decrease in the left half of the chest •• Botkin-II symptom - crepitus and wheezing along the left edge of the sternum •• Auenbrugger symptom - epigastric pulsation of the left ventricle.
• Valvular symptoms •• Diastolic cat purring at the apex of the heart •• Romberg's symptom - flapping 1st sound at the apex of the heart •• The sound of the mitral valve opening (heard at the apex of the heart no later than 0.12 seconds after the 2nd sound), creating, together with Romberg's murmur auscultatory picture of the melody of mitral stenosis, or the rhythm of a quail •• At the apex, low-frequency diastolic murmur is determined in different variants - presystolic, protodiastolic, holodiastolic with proto- and presystolic amplification •• Presystolic murmur is heard with a normal rhythm, the murmur disappears with atrial fibrillation, which often complicates mitral stenosis •• With pronounced stenosis, the murmur may completely disappear •• Often, along with diastolic murmur, systolic murmur is also heard, due to concomitant mitral insufficiency, relative tricuspid insufficiency, and systolic murmur can also be of intraventricular origin •• The murmur of mitral insufficiency is carried out in the left axillary region, tricuspid insufficiency - to the right (on the sternum and to the right of it), intraventricular murmur - upward, the murmur of mitral stenosis intensifies with load (squats, raising legs) and does not go anywhere (“dies where it originates”).
• Symptoms caused by a violation of the pumping function of the heart •• Diffuse moist rales of different sizes, better heard in the basal sections •• Strengthening of the second tone over the pulmonary artery •• Facies mitralis - blush on the cheeks and cyanosis of the lips •• Graham Still's murmur with relative insufficiency of the pulmonary valve •• Expansion of the borders of the heart to the right and push of the right ventricle with its hypertrophy •• Swelling of the neck veins, edema, ascites, enlarged liver, Plesch's symptom - with the development of stagnation in the systemic circulation.
• Symptoms of the underlying disease (rheumatism, congenital heart disease).
Special studies
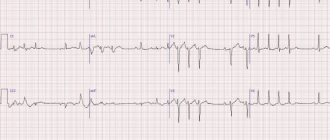
• ECG •• Signs of hypertrophy of the left atrium and right ventricle •• Supraventricular tachyarrhythmias, most often - atrial fibrillation.
• X-ray of the chest organs •• Bulging of the arch of the left atrium, pulmonary artery and right ventricle •• Smoothing of the waist of the heart (mitral configuration) •• Deviation of the contrasted esophagus along a small radius arch •• Widening of the shadows of the vena cava •• Calcification of the mitral valve •• Widening of the shadows roots of the lungs •• Strengthening the pulmonary pattern, Kerley V. lines.
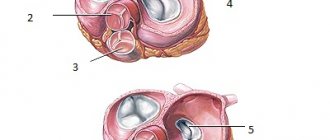
• EchoCG •• Determination of the area of the MR in Doppler mode using peak and average transmitral pressure gradients and in B-mode (to assess the severity, the smallest number is taken as a basis), deformation and calcification of the valve apparatus •• With fusion of the mitral valve leaflets when scanning along the short axis The MO has the shape of a “fish mouth”; during contraction of the left atrium, the anterolateral leaflet bulges into the cavity of the left ventricle, and in the M-mode the characteristic U-shaped movement of the anterior leaflet of the mitral valve is determined •• Enlargement of the left atrium, right ventricle •• In pulsed wave Doppler mode peak E disappears in the spectrum of transmitral blood flow •• Transesophageal echocardiography is performed in all patients to exclude thrombosis of the left atrium and vegetations, even with a normal rhythm, as well as to determine the degree of valve calcification (I degree - calcification is located along the free edges of the leaflets or in the commissures in separate nodes, II degree - calcification of the valves without transfer to the fibrous ring, III degree - transition of calcium masses to the fibrous ring and surrounding structures).
• Catheterization of all chambers of the heart •• Increased pressure in the left atrium and pulmonary artery, as well as the transmitral pressure gradient •• Increased pressure in the right parts of the heart with right ventricular failure •• Conducting functional tests with aminophylline and oxygen to determine the reversibility of pulmonary arterial hypertension and surgical prognosis treatment •• The study is carried out if the clinical picture does not correspond to the echocardiography data.
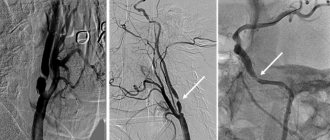
• Left atriography and ventriculography •• Increased volume of the left atrium •• Slow expulsion of contrast from the left atrium (usually in a thin stream) •• Funnel-shaped border between the left atrium and left ventricle •• The study is carried out if the clinical picture does not correspond to the echocardiography data.
• Coronary angiography. Performed in the presence of episodes of angina and positive results of stress testing, as well as in all women over 45 years of age, men over 40 years of age and all candidates for mitral valve replacement.
TREATMENT
• Drug therapy •• Prevention of infective endocarditis (see Infectious endocarditis) •• Diuretics under the control of echocardiography (possibility of reducing the transmitral gradient and reducing cardiac output) •• b-blockers, incl. in patients with sinus rhythm, by reducing heart rate, they reduce pressure in the left atrium against the background of exercise •• Indirect anticoagulants (maintain INR at 2.0–3.0) for atrial fibrillation, a history of thromboembolism and a sharp increase in the left atrium •• B in the acute period of thromboembolism, heparin is prescribed (activated PTT is maintained 1.5–2 times higher than normal), having previously performed a CT or MRI of the head to exclude intracranial hemorrhages and echocardiography to detect thrombosis of the left atrium and vegetations on the mitral valve •• In case of repeated thromboembolism, a dose of indirect anticoagulants increase until the INR is maintained at 3.0–4.5 and antiplatelet agents are added (for example, acetylsalicylic acid at a dose of 80–160 mg/day).
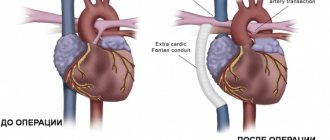
• Surgical treatment •• Indications ••• Severe and critical stenosis, regardless of the presence of clinical symptoms ••• Moderate stenosis with III-IV functional class of circulatory failure or repeated embolisms •• Contraindications ••• Severe concomitant pathology that threatens the patient’s life •• • Terminal stage of circulatory failure ••• Negative test result with aminophylline and oxygen ••• The activity of the rheumatic process is not considered a contraindication to surgical treatment •• Methods of surgical treatment ••• Percutaneous balloon valvuloplasty is performed in the absence or grade I of mitral valve calcification, preservation of the valve device, isolated stenosis or complex mitral disease with a predominance of stenosis and regurgitation no more than grade I, absence of left atrium thrombosis and concomitant ischemic heart disease ••• Closed mitral commissurotomy is rarely performed due to greater invasiveness and a large number of complications for similar indications ••• Because of due to the high frequency of relapses of the defect and the need for reoperations, open mitral commissurotomy under conditions of artificial circulation is actually performed only together with thrombectomy from the left atrium before a planned pregnancy ••• Mitral valve replacement under conditions of artificial circulation using biological prostheses is performed for children or before a planned pregnancy •• • In other cases (and in all cases of infective endocarditis), the affected valve is replaced with a mechanical prosthesis ••• During pregnancy, surgery is recommended at 14–26 weeks, or at 37–39 weeks simultaneously with a cesarean section.
Specific postoperative complications • Thromboembolism • Secondary infective endocarditis of prostheses • Atrioventricular block • Dystrophic changes in biological prostheses, restenosis and the need for re-prosthesis • Specific complications of balloon valvuloplasty: thromboembolism - 1-4%, severe mitral regurgitation requiring mitral valve replacement - 1-3 %, transient AV block - 1%, cardiac tamponade - 1%, ASD - 20% (the ratio of pulmonary minute volume to systemic blood flow is usually below 1.0, in most cases the size of the defect decreases within 3-6 months).
Prognosis • 1-year survival in the natural course of the disease - 78%, 2-year survival - 67%, 5-year - 50%, 9-year - 35% • Mortality with closed mitral commissurotomy - 0.5–1% • Over the next 10 years, 20% of patients experience restenosis • 5-year survival rate after balloon valvuloplasty - 95%, mortality - about 1% • Mortality during operations with artificial circulation - 2-8% • 5-year survival rate after valve replacement - 85 %, 9-year - 78% • 8-year survival rate after complex reconstructive operations on the mitral valve - 87%, number of complications - 6%, reoperations - 7%.
Synonyms • Mitral valve stenosis • Stenosis of the left atrioventricular orifice • Narrowing of the left atrioventricular orifice • Narrowing of the left venous orifice
Abbreviations • MS - mitral stenosis • MO - mitral orifice
ICD-10 • I05.0 Mitral stenosis