AMPP usually does not pose a threat to the baby’s life; such children develop normally, and over time this disease can go away on its own. But in cases where the child’s pathology is not limited to one aneurysm, but is combined with another heart defect, then this is, of course, a cause for concern for parents. A good ultrasound specialist in Makhachkala can detect heart abnormalities in a newborn during an ultrasound examination already in the first days of the baby’s birth.
Types and consequences of pathology
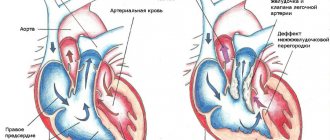
An atrial septal aneurysm is an abnormal bulging of the wall between the atria to one side. Most often, the protrusion occurs in the direction where the open oval window (OOF) was located, since in this place the heart muscle is not yet strong enough. The oval window between the atria is necessary for the fetus while it is in the womb, when pulmonary respiration is not yet functioning. It promotes the redistribution of blood flow between the left and right atria and should close after the baby is born.
However, in the practical activities of medical specialists in Makhachkala, there are cases when a newborn’s window remains open or not completely closed for quite a long time (a year or more). This leads to the fact that, under the pressure of the blood flow, the insufficiently strengthened myocardial wall begins to protrude in some direction. In medical practice, the combination of an aneurysm with an existing septal defect in children is much more common than AMPP alone without any additional heart pathologies. Types of aneurysm are classified depending on which direction the deflection of the interatrial septum is directed, such as:
- With protrusion into the right atrium.
- To the left atrium.
- S-shaped, in which different parts of the septum bulge in different directions.
If the occurrence of an aneurysm does not lead to a redistribution of blood flow from one cardiac chamber to another, then such a pathology does not pose a danger, and the prognosis can be called favorable. Otherwise, due to an increase in blood pressure in the pulmonary trunk, pulmonary hypertension may develop.
Short description
Atrial septal defect (ASD) is a congenital heart defect with communication between the atria. Statistical data: 7.8% of all congenital heart disease detected in infancy, and 30% in adults; VSD of the ostium secundum type - 70%, ostium primum - 15%, sinus venosus - 15%; Lutembashe syndrome accounts for 0.4% of all cases of ASD, the combination of ASD with mitral valve prolapse - 10–20%; the predominant gender is female (2:1–3:1).
Code according to the international classification of diseases ICD-10:
- Q21.1 Atrial septal defect
What are the external manifestations of the disease?
With a congenital aneurysm of the interatrial septum in children, when there are no additional heart defects in the baby, the disease does not affect the physical or mental development of the baby and is not expressed by any symptoms. It’s another matter if the pathology is combined with other congenital heart diseases. In such cases, the child exhibits signs such as:
- increased heart rate;
- bluish skin in the nasolabial triangle;
- the presence of shortness of breath in the baby during breastfeeding;
- tearfulness, anxiety;
- sleep disorders.
Older children may experience signs of tachycardia, pain in the chest from the heart, increased fatigue, weakness, dizziness, loss of appetite, headaches, drowsiness, etc.
Treatment of minimal brain dysfunctions in children at CORTEX MC.
Brain dysfunctions (MMD) in children are the most common form of neuropsychiatric disorders in childhood: the incidence rate among preschool and school-age children reaches 5–20%. With MMD, there is a delay in the rate of development of the functional systems of the brain that provide such complex integrative functions , such as speech, attention, memory, perception and other forms of higher mental activity. In terms of general intellectual development, children with MMD are at the normal level, but at the same time they experience significant difficulties in school learning and social adaptation. Due to focal damage, underdevelopment or dysfunction of certain parts of the cerebral cortex, MMD in children manifests itself in the form of motor and speech development, formation of writing skills (dysgraphia), reading (dyslexia), counting (dyscalculia). The term “minimal brain dysfunction” became widespread in the 1960s, when it began to be used in relation to a group of conditions of varying etiology and pathogenesis, accompanied by behavioral disorders and learning difficulties not associated with a general lag in intellectual development. Due to the diversity of clinical manifestations and the heterogeneity of factors underlying the etiology and pathogenesis of MMD, diagnostic criteria have been developed for a number of conditions previously considered within the framework of MMD.
List of nosological forms considered according to ICD 10 within the framework of the MMD.
| ICD code - 10 | Nosological form of the disease |
| Section F 8 | Psychological development disorders |
| F 80 | Speech development disorders |
| F 81 | Disorders of development of school skills: dysgraphia, dyslexia, dyscalculia |
| F 82 | Developmental disorders of motor functions - dyspraxia |
| Section F 90-F98 | Behavioral and emotional disorders, usually beginning in childhood and adolescence |
| F 90 | Attention deficit hyperactivity disorder |
| F91 | Behavioral disorders |
The reasons for the development of minimal brain dysfunction are not fully understood.
The main factors influencing the appearance of cerebral dysfunction are:
• hereditary predisposition;
• hemolytic disease occurs in the fetus, which develops in the event of a Rh conflict with the mother, which leads to the destruction of the child’s red blood cells;
• various diseases and infections that a woman suffered during pregnancy;
• maternal anemia: malnutrition, vitamin deficiency, etc.;
• severe toxicosis;
• threat of termination of pregnancy (miscarriage), for example, due to severe stress, hypertonicity or hypotonicity of the uterus, etc.;
• any harmful external influences on a woman during pregnancy: radiation, viruses, infections, bacteria, etc., this also includes poor environmental conditions;
• lack of oxygen (hypoxia), suffocation of the fetus (asphyxia) during labor, for example, the umbilical cord entwining the baby’s throat, or a long passage of the fetus through the birth canal;
• premature birth;
• weak labor activity or, conversely, rapid labor;
• damage to the spinal cord during childbirth;
• lack of nutrition in infancy and early childhood;
• development of diseases in the baby such as heart disease, bronchial asthma, infectious diseases, etc.
MMD begins to manifest itself most clearly when children are preparing for school or in the lower grades. It can be observed that the child does not assimilate new information well and has difficulty remembering it; he has problems with handwriting and writing in general. And the point is not that the child has a low intellectual level or does not want to learn, the problem is that MMD affects every sphere of life.
Clinical manifestations of minimal brain dysfunction vary depending on the age of the child:
In infants, the main symptoms of MMD are:
• increased tearfulness and moodiness;
• increased heart rate, sweating, breathing rate;
• presence of spasms and convulsions;
• disorders of the gastrointestinal tract: frequent regurgitation, diarrhea, etc.;
• difficulty sleeping and falling asleep.
The main syndromes that occur in school-age children:
Hyperactivity and attention deficit disorder: - fidgeting in a chair, inability to sit in one place); - the child leaves games and other things unfinished, cannot concentrate on one thing for a long time, begins many actions at once; - often loses things, falls, collides with objects and others; - enters into conflicts, is capricious, aggressive towards loved ones and himself; - problems arise with subjects that require high concentration of attention, long-term mental operations (mathematics, essays, memorizing poems). Sphere of attention: voluntary memorization is impaired, concentration and volume are reduced. It manifests itself mainly in the fact that the child is absent-minded and cannot do the same thing for a long time, especially if it requires mental stress. Speech sphere: the first thing you should pay attention to is the child’s articulation - unclear pronunciation of words and sounds. You can also notice that the child sometimes does not perceive other people’s speech well and does not assimilate information by ear (impaired auditory-verbal memory). This manifests itself in poor vocabulary, difficulty in retelling what was heard or read, and difficulty constructing long sentences. Memory disorders: manifest themselves mainly in difficulties in mechanical memorization, i.e. through repeated repetition. Motor sphere: in such children one can often observe violations of fine motor skills of the hands. This mainly manifests itself in general awkwardness of movements and handling of objects. The child has difficulty fastening small buttons, tying shoelaces, using scissors, and sewing; at school, difficulties arise with neat handwriting and reading speed. Spatial orientation: such children often confuse “left” and “right”, can write all letters in mirror images, etc. Emotional sphere: lability of emotional state. Children with this disorder rapidly change their mood from depressed to euphoric. Unreasonable outbursts of aggression, anger, and irritability may occur, both towards others and towards oneself. One can observe traits of infantility (capriciousness), hysterical personality, and lack of independence.
The maximum severity of MMD manifestations often coincides with critical periods of psychospeech development.
— The first period includes the age of 1–2 years, when intensive development of cortical speech zones and active formation of speech skills occur. - The second period occurs at the age of 3 years. At this stage, the child’s stock of actively used words increases, phrasal speech improves, and attention and memory actively develop. At this time, many children with MMD exhibit delayed speech development and articulation disorders. — The third critical period refers to the age of 6–7 years and coincides with the beginning of the development of written language skills (writing, reading). Children with MMD of this age are characterized by the development of school maladjustment and behavior problems. Significant psychological difficulties often cause various psychosomatic disorders and manifestations of vegetative-vascular dystonia. During adolescence, a number of children with MMD experience increased behavioral disturbances, aggressiveness, difficulties in relationships in the family and school, academic performance deteriorates, and a craving for alcohol and drug use appears.
Therefore, the efforts of specialists should be aimed at timely detection and correction of MMD.
Treatment of MMD is complex and includes several areas: - Psychological and pedagogical measures: 1. The child should be provided with sufficient physical activity: in the case of hyperactivity, it is necessary to give vent to emotions and mobility, and in cases of hypoactivity it is necessary that the loads are not unbearable, but at the same time time stimulated activity. 2. It is necessary to ensure a healthy psychological atmosphere in the family and environment. It is important to create calm and stability, because they will help correct mood swings. Overly strict discipline should not be allowed, but one should also not be overprotective or indulge in whims. 3. It is necessary to observe certain routine moments (go to bed and get up at the same time, set aside time for work and rest, etc.). 4. Contribute to the development of the child’s weaknesses: play games that require fine motor skills, memorize fairy tales and poems, but not mechanically - try to interest the child in the content, etc. An important condition for treatment will be classes with a psychologist, special teachers and speech therapist. Drug therapy occupies an important place in the treatment of MMD along with methods of psychological and pedagogical correction. Drug therapy is prescribed according to individual indications in cases where cognitive impairment and behavioral problems in a child with MMD are so pronounced that they cannot be overcome only with the help of psychological and pedagogical measures. Currently, various groups of drugs are used in the treatment of MMD, including antioxidants (Mexidol, Actovegin), nootropic drugs (Cerebrolysin, Encephabol, Semax, Cortexin). However, the above methods, while affecting individual symptoms of MMD, do not affect the causes of the disease as a whole and, as a result, do not always give a pronounced positive effect overall.
Specialists of the CORTEX MC have developed a new highly effective method of treating children suffering from various forms of mental and speech developmental delays, including MMD - BIOPHYSICAL ACTIVATION of speech centers of the brain. The main neurospecific treatment - BPA - affects the brain through the projection zones of speech, praxis, gnosis; on the articulatory apparatus, promotes their activation, stimulates the development of stable connections and improves the functioning of the first and second signaling systems of the brain, which integrate all signals from the outside world and form the child’s meaningful responses, his speech, memory, attention, and promotes his socialization. The treatment technique is based both on the activation of the speech centers themselves (Broca's area, Wernicke's area, angular gyrus, etc.), and on the restoration of lost connections not only between centers, but also interhemispheric ones. In addition, scattered interneuronal connections of speech centers with other areas of the brain involved in speech function are restored. Treatment of MMD should be comprehensive, which leads to a more pronounced and lasting positive effect. Specialists from CORTEX MC have developed a new highly effective treatment complex for children suffering from various forms of mental retardation and MMD. The components of the treatment process are: diagnosis, the main neurospecific pathogenetic treatment - BFA of the speech centers of the brain and a complex of auxiliary treatment. At the CORTEX MC, each patient must undergo a comprehensive, comprehensive examination : an initial examination by a pediatric neurologist, consultation with a pediatrician, testing of speech functions by a speech therapist-speech pathologist, psychological counseling, computer EEG and evoked potentials of the brain and spinal cord, as well as a neuroimmunological examination of blood for neurotropic viruses (cytomegalovirus, rubella, Epstein-Barr, herpes simplex and others), study of the level of antibodies to specific proteins of the central nervous system in order to determine the degree of damage and hypoxia of nervous tissue. The study allows us to identify a hidden neuroinfection that inhibits the maturation of speech, gnostic and praxis centers. All of the above diagnostic methods make it possible to predict the further course of the disease and formulate the most optimal treatment complex for each patient, as well as confirm, clarify or change the diagnosis.
Auxiliary treatment is a complex that includes the most advanced medical technologies for the symptomatic treatment of various forms of mental retardation, mental retardation and malignant retardation:
1. Neuroprotective therapy for regulating the integrative activity of the brain, lymphatic intercellular therapy and endonasal cortexin electrophoresis are techniques that allow small doses of cerebroprotectors to be delivered endolymphatically; they directly enter the brain tissue, bypassing the blood-brain barrier.
2. Transcranial and transvertebral micropolarization successfully combines non-invasiveness and selectivity of influence, allowing to improve or restore motor, mental, and speech functions. The direction of influence is achieved through the use of small areas of electrodes located on the corresponding cortical (frontal, motor, temporal, etc.) or segmental (lumbar, thoracic, cervical, etc.) projections of the brain or spinal cord.
3. Differentiated segmental massage, which helps normalize muscle tone and has relaxing and sedative effects in case of hyperexcitability of the child.
4. For the purpose of neurophysiological regulation of the stato-kinetic function of the central nervous system, the CORTEX MC uses a unique development of the Center for Aerospace Medicine - the plantar support load simulator “Corvit”. The device allows you to simulate indicators of the physical impact on the foot when walking, which helps to normalize the processes of excitation and inhibition in the central nervous system, the development and restoration of coordination of movements. The device ensures the occurrence of an impulse and its delivery to the cerebellar cortex, allowing indirect formation and improvement of speech skills and perception of the surrounding world.
5. Speech therapy correction includes diagnosis of the degree of speech disorders, daily classes aimed at improving speech function and speech therapy massage to correct various types of dysarthria and dysphagia;
6. Psychological assistance includes: individual consultations, pathopsychological tests (study of attention, memory, thinking, characteristics of the emotional and personal sphere) and neuropsychological tests (study of lateral preferences, motor and sensory asymmetry, general awareness, cognitive, speech, mnestic, intellectual functions). An experimental psychological report is drawn up and given to parents. The specialist selects an individual psychological program for correcting disorders in a particular area for a particular child and further recommendations.
7. Method of audiovocal training RUSTOMATIS according to the method of A. Tomatis. In the 50s of the 20th century, while the author was studying the method of influencing the human brain with sounds of different frequencies, it was discovered that the ear not only hears sounds of different frequencies and laterality - the vibrations are converted into electrical impulses that enter the brain. Currently, a special device for recording high-frequency and low-frequency components has been developed - the “electronic ear”. By alternating such music through tension and relaxation, the child’s middle ear apparatus – the hammer and stapes – is trained, with the help of which the range of perception of external factors expands, concentration of attention increases, new information enters the brain and, as a result, many disorders and disorders disappear. The audio correction system configures, trains and “trains” the vestibular apparatus and auditory analyzer systems to correctly process incoming information.
In the process of complex treatment, a physiological, consistent interaction of all areas of the brain associated with speech production, involved in the control of higher cognitive functions and associative systems of the brain, is formed. The child’s memory improves, attention increases, fine motor skills develop, and thinking becomes more active. During treatment, it is possible to significantly improve speech and behavior, children become calmer, better assimilate new information, and their success in school increases.
Early detection and correction of symptoms of minimal brain dysfunction is very important when the processes of morphofunctional development of the central nervous system continue, its plasticity and reserve capabilities are great. If the diagnosis was made accurately and on time, parents and teachers, doctors interact actively and were able to develop the necessary tactics of communication with the child, then with age the person will compensate for almost all the disorders, and he will be able to live a full life.
Diagnosis and treatment of AMPP
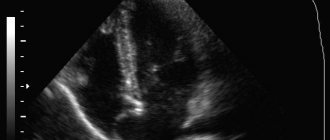
The main, effective method for detecting aneurysm of the interatrial septum in children is ultrasound examination of the heart, which is also called echocardiography. This procedure is characterized by absolute safety and the absence of any painful sensations for the child being examined. All clinics of the medical network in Makhachkala use the most modern ultrasound machines, which are staffed by highly qualified specialists, which makes it possible to reliably diagnose even the smallest patients with hidden, asymptomatic forms of pathologies.
If mild forms of aneurysm are detected in children, no special treatment is required. Such babies need to undergo a consultation with a cardiologist once a year after undergoing ultrasound diagnostics. Young patients are recommended to undergo gentle physical activity, avoid psycho-emotional stress, walks and games in the fresh air, good, long sleep and a balanced diet rich in vitamins, protein and microelements necessary for the child. Psychotherapy sessions and auto-training are very useful for children with AMPP. To improve cardiac activity, the attending physician usually also prescribes electrophoresis procedures with magnesium.
Causes
Etiology: factors that form congenital heart disease (see Tetralogy of Fallot).
Pathogenesis • The magnitude and direction of shunt depend on the size of the defect and the relative compliance of the ventricles • In adults, the right ventricle is more compliant than the left, as a result of which shunt occurs from the left atrium to the right • A small shunt leads to a moderate volume overload of the right heart, and pressure in the pulmonary artery remains normal • The severity of pulmonary hypertension may be insignificant even with a large shunt • Only in rare cases does severe pulmonary hypertension develop, leading to right ventricular failure and right-to-left shunt • Unlike VSD, with ASD the shunt is smaller and affects only the right side of the heart.
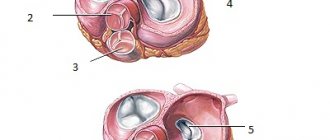
Variants of ASD • Ostium secundum (secondary defects) are localized in the area of the oval fossa, are often multiple, accompany many syndromes: Holt-Oram syndrome (ASD of the ostium secundum type in combination with digital hypoplasia), Lutembashe syndrome (combination of ASD with mitral valve stenosis), combination of ASD with mitral valve prolapse, etc. • Ostium primum (primary defects) are usually large in size, localized in the lower part of the septum, at the attachment point of the mitral and tricuspid valves, interatrial and interventricular septa. They are part of an open AV canal and are often combined with abnormal drainage of the pulmonary veins, splitting of the anterior mitral valve leaflet, mitral regurgitation and Down syndrome • Defects of the sinus venosus type are localized near the mouth of the superior vena cava and the sinus node, often combined with sick sinus syndrome, AV - nodal rhythm and abnormal drainage of the pulmonary veins.
Symptoms (signs)
Clinical picture
Complaints: shortness of breath, palpitations, fatigue during physical activity, retarded physical development, frequent infections, paradoxical embolisms.
Objectively • Pallor of the skin • Harrison's furrows - displacement of areas of the chest as a result of chronic shortness of breath • Splitting of the first tone with a pronounced component of the tricuspid valve • Pronounced fixed splitting of the second tone (pronounced - due to - due to prolongation of the time of blood ejection from the right ventricle; fixed - due to - due to the fact that the dependence of venous return on the phases of breathing is leveled by discharge from the left atrium) • An ejection click and a soft systolic murmur of relative stenosis of the pulmonary artery in the second intercostal space to the left of the sternum • Due to an increase in blood flow through the tricuspid valve, a low-frequency diastolic murmur sometimes occurs above the xiphoid process of the sternum.