Main risk factors
If a woman, especially over 35 years of age, has one or more of the following factors in her medical history, her obstetrician-gynecologist may refer her to a consultation with a cardiologist and geneticist to keep the situation under control. The defect can be recognized in the second trimester of pregnancy, and it can be provoked by:
- multiple miscarriages or abortions;
- diabetes;
- metabolic diseases;
- intoxication during pregnancy - alcohol, drugs, nicotine;
- the presence of congenital heart disease in one of the parents;
- certain infections, such as influenza, rubella, or systemic lupus erythematosus;
- drinking coffee in large quantities;
- genetic disorders in the fetus, including Down's disease.
Only an experienced geneticist can predict how likely it is to develop a defect after analyzing all the factors. You should not ignore this possibility if the attending physician insists on it.
Symptoms of congenital heart disease
They are divided into two large groups according to the color of the child’s skin: “white” and “blue”. A changed skin tone is the first reason for parents and pediatricians to be wary.
"Blue" vices
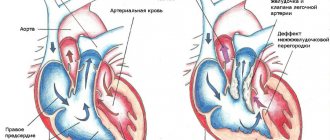
They usually appear either immediately at birth or a little later. In this case, the ears, lips and body skin are susceptible to cyanosis. Blue discoloration can occur during exertion (screaming, crying of a newborn), during breastfeeding. The “blue” appearance is usually manifested by a mirror arrangement of the great vessels, atresia of the pulmonary artery, and tetralogy of Fallot.
CHD of the “white” variety
Accompanied by pallor and coldness of the extremities. When listening with a stethoscope, noises are heard. They are not direct symptoms, but a heart examination is still required. With “white” pathologies, heart failure is often detected. Changes are detected on x-rays, ECG, ECHO-CG. This type of congenital heart disease is most often a pathology of the interatrial septum and interventricular septum.
Unfortunately, not all types of congenital heart disease occur in newborns. A child can feel well even up to 10 years of age. But sooner or later the vice will appear:
- delay in physiological development;
- pallor or cyanosis;
- shortness of breath during exercise.
What causes lead to congenital heart disease and can they be avoided?
A number of reasons lead to the occurrence of congenital heart disease: some of them, by the way, have a negative impact on the health of the mother, who may need treatment for arrhythmia, tachycardia or hypotension.
- Chromosomal factor. In 5% of cases, the disease develops due to a violation of the chromosomal apparatus. According to statistics, more than 40% of children with Down syndrome have a history of congenital heart disease.
- Gene mutation. Studies have repeatedly confirmed that it is enough to mutate just one gene for it to affect the functioning of the cardiovascular system in this way. As in the previous case, it is impossible to influence this reason.
- Infections. Various infections and viral epidemics are considered dangerous for the fetus, primarily rubella, influenza, chickenpox, serum hepatitis, mycoplasmosis, tuberculosis, and syphilis. The task of future parents is to protect themselves from potential contacts with carriers: they are quite capable of doing this.
- Intoxication. Toxic substances negatively affect the formation of the child’s organs, including the heart. Therefore, pregnant women are prohibited from working in pharmaceutical shops and chemical laboratories. Alcohol intoxication is especially dangerous, as it disrupts the normal formation of heart valves. It is very important to protect a woman from this, especially in the first trimester, and also to avoid taking teratogenic drugs.
- Heredity. Statistics say that genetic predisposition is present in 90% of cases of congenital heart disease.
- Diabetes mellitus in the mother. About 5% of congenital heart diseases develop against the background of this metabolic pathology.
- Physical influences. Radiation - X-ray, ionizing, as well as high atmospheric pressure can lead to heart disease. Forewarned is forearmed!
Parents who take the health of their unborn child seriously undergo consultations with a geneticist to eliminate risks, and also do not skip routine examinations. If the diagnosis is confirmed, experts will recommend and justify what to do - continue the pregnancy or terminate it.
Sex-linked recessive inheritance
Sex-linked developmental defects are mainly caused by recessive mutations in the female sex chromosome (this type of inheritance is also called X-chromosomal). This trait is always transmitted through the mother, a carrier of the recessive “sick” gene (i.e., the woman herself is healthy). Almost all of those affected are men (the affected gene on the X chromosome does not have a “partner” on the Y chromosome that could dominate it). A sick man never transmits the disease to his sons (after all, they receive from him a “healthy” Y-chromosome, and not a mutant X-chromosome), but all his daughters will be carriers of the “fatal” gene.
We have schematically described the types of inheritance to give the reader a general understanding of the nature of these mechanisms. In fact, everything is much more complicated - much less clear and definite.
The table below lists, by way of example, just some of the hereditary abnormalities compatible with life.
| Anomaly | Inheritance mechanism | Manifestation | Treatment and rehabilitation measures |
| Albinism | Autosomal recessive inheritance - it is possible to have an albino child from healthy parents. Population frequency 1:20,000 | Lack of normal pigmentation of the skin, hair, iris of the eye | This hereditary anomaly is not considered a disease in the full sense of the word and cannot be treated |
| Hemophilia | Sex-linked recessive inheritance. Mostly men are affected. Passed on from mother to sons | The disease is caused by a deficiency of certain blood clotting factors. Manifested by bleeding | Treatment for bleeding - blood transfusion, plasma; general hemostatic agents; antihemophilic globulin; prevention of injuries and bleeding |
| Colorblindness | Sex-linked recessive inheritance. It is observed mainly in men. Passed on from mother to sons | Partial color blindness. Most often distributed in red and green colors | Color vision disorders are detected using special tables or spectral devices. Colorblindness cannot be cured |
| Down's disease | Chromosomal abnormality: in the mother, during the maturation of the egg, under the influence of as yet unclear reasons, 3 chromosomes are formed in the 21st pair of chromosomes instead of 2. Frequency in the population - 1:700 | One of the forms of congenital dementia. The degree of mental underdevelopment varies significantly. Patients are generally affectionate, good-natured, and friendly. | Therapeutic pedagogy based on the tendency of patients to imitate. Education in auxiliary schools, occupational therapy |
| Ptosis | Autosomal dominant inheritance, transmitted to children from parents with a congenital form of the disease | Drooping of the upper eyelid due to underdevelopment of the muscle that lifts it | Surgery |
Sources
- Pereira SP., Tavares LC., Duarte AI., Baldeiras I., Cunha-Oliveira T., Martins JD., Santos MS., Maloyan A., Moreno AJ., Cox LA., Li C., Nathanielsz PW., Nijland MJ., Oliveira PJ. Sex dependent Vulnerability of Fetal Nonhuman Primate Cardiac Mitochondria to Moderate Maternal Nutrient Reduction. // Clin Sci (Lond) - 2021 - Vol - NNULL - p.; PMID:33899910
- Ben Abdelaziz A., Bchir A., Ben Salah A., Ben Salem K., Mansour N., Hsairi M., Ennigrou S., Nacef T., Dhidah L., Bellaj R., Mehdi F. Professor Mohamed Soussi Soltani : Leader, Innovator and Researcher in Public Health. // Tunis Med - 2021 - Vol99 - N1 - p.5-11; PMID:33899170
- Saavedra LPJ., Prates KV., Gonçalves GD., Piovan S., Matafome P., Mathias PCF. COVID-19 During Development: A Matter of Concern. // Front Cell Dev Biol - 2021 - Vol9 - NNULL - p.659032; PMID:33898461
- Alexanderson-Rosas E., Antonio-Villa NE., Sanchez-Favela M., Carvajal-Juarez I., Oregel-Camacho D., Gopar-Nieto R., Flores-Garcia AN., Keirns C., Hernandez-Sandoval S. ., Espinola-Zavaleta N. Assessment of Atypical Cardiovascular Risk Factors Using Single Photon Emission Computed Tomography in Mexican Women. // Arch Med Res - 2021 - Vol - NNULL - p.; PMID:33896676
- Bhasin D., Arora GK., Isser HS. Young woman with recurrent pregnancy loss. // Heart - 2021 - Vol107 - N10 - p.821-854; PMID:33893215
- Lee K., Laviolette SR., Hardy DB. Exposure to Δ9-tetrahydrocannabinol during rat pregnancy leads to impaired cardiac dysfunction in postnatal life. // Pediatr Res - 2021 - Vol - NNULL - p.; PMID:33879850
- Richards C., Sesperez K., Chhor M., Ghorbanpour S., Rennie C., Ming CLC., Evenhuis C., Nikolic V., Orlic NK., Mikovic Z., Stefanovic M., Cakic Z., McGrath K ., Gentile C., Bubb K., McClements L. Characterization of cardiac health in the reduced uterine perfusion pressure model and a 3D cardiac spheroid model, of preeclampsia. // Biol Sex Differ - 2021 - Vol12 - N1 - p.31; PMID:33879252
- Song Y., Xu J., Li H., Gao J., Wu L., He G., Liu W., Hu Y., Peng Y., Yang F., Jiang X., Wang J. Application of Copy Number Variation Detection to Fetal Diagnosis of Echogenic Intracardiac Focus During Pregnancy. // Front Genet - 2021 - Vol12 - NNULL - p.626044; PMID:33868367
- Khanna R., Chandra D., Yadav S., Sahu A., Singh N., Kumar S., Garg N., Tewari S., Kapoor A., Pradhan M., Goel PK. Maternal and fetal outcomes in pregnant females with rheumatic heart disease. // Indian Heart J - 2021 - Vol73 - N2 - p.185-189; PMID:33865516
- Kirby A., Curtis E., Hlohovsky S., Brown A., O'Donnell C. Pregnancy Outcomes and Risk Evaluation in a Contemporary Adult Congenital Heart Disease Cohort. // Heart Lung Circ - 2021 - Vol - NNULL - p.; PMID:33863666
Classification of fetal anomalies
Developmental pathologies include:
- abnormalities in the development of the neural tube - absence of the cerebral hemispheres, hydrocephalus, cerebral herniation, microcephaly;
- spinal defects - myelomeningocele, spina bifida, cystic hygroma;
- heart pathologies - abnormal position of the heart, underdevelopment of the organ, ventricular septal defect;
- anomalies of the gastrointestinal tract - atresia of the cardia, duodenum, jejunum;
- malformations of the anterior abdominal wall - omphalocele, gastroschisis, ascites in the fetus;
- congenital kidney anomalies - underdevelopment, urinary tract obstruction, polycystic disease;
- pathologies of the amount of amniotic fluid - oligohydramnios, polyhydramnios;
- intrauterine fetal death.
Neural tube malformations
- Anencephaly is a pathological condition characterized by the congenital absence of the cranial vault and cerebral hemispheres. This is the most common pathology of the central nervous system in the fetus. It is diagnosed at 11-12 weeks. As a rule, the defect is combined with hydramnios and other disorders. The level of alpha-fetoprotein in the mother's blood increases.
- Signs of hydrocephalus in the form of expansion of the anterior and posterior horns of the lateral ventricles will be visible at 18 weeks of pregnancy.
- Microcephaly - a pathological reduction of the fetal head - occurs when the biparietal size decreases by more than three standard deviations. To rule out intrauterine growth retardation, the doctor will compare the size of the head with the size of the body of the unborn child. In isolated form, the defect is rare, and in borderline cases, the diagnosis is quite difficult to make. In this regard, the woman is recommended to undergo an ultrasound again in a few weeks. The data obtained are interpreted quite carefully, especially if the fetus grows and develops normally.
- Encephalomeningocele usually appears as a rounded protrusion in the area of the calvarial bones. Inside the protrusion is fluid or brain matter. Most often, anomalies are localized at the back of the head, but sometimes anterior localization of the defect occurs. To minimize the likelihood of diagnostic error, if an encephalomeningocele is suspected, the woman will be advised to undergo a repeat ultrasound, possibly from a different doctor.
Anomalies of the spine
Most often, fetal pathologies in the form of anomalies in the development of the spine are localized in the cervical and lumbar region. Since the spine is clearly visualized from the 15th week of pregnancy, its defects are diagnosed at 18-20 weeks, during the second screening ultrasound.
- Myelomeningocele on ultrasound is visualized as a sac containing fluid and elements of the spinal cord. In rare cases, an open defect is diagnosed, in which only protrusion of soft tissue through the defect is detected. Such anomalies are particularly difficult to detect.
- Spina bifida in the fetus is diagnosed using expert-class, high-resolution ultrasound machines. Normally, the posterior ossification centers of the spine are visualized as two hyperechoic, almost parallel structures. In spina bifida they are displaced laterally.
- Cystic hygroma is a pathology of the development of the lymphatic system. In this case, an ultrasound reveals a cyst with septa located in the cervical spine. Sometimes internal partitions are visible, resembling the spokes of a wheel. The skull, brain and spinal cord, unlike other anomalies, develop normally. Sometimes cystic hygroma is combined with a generalized anomaly of the lymphatic system. In most such cases, the fetus dies.
Congenital heart defects
Diagnosis of congenital heart defects requires special equipment. The doctor should be able to perform Doppler ultrasound. If congenital heart defects are suspected, an expert opinion is required. In difficult cases, clinicians are warned about possible complications so that they are ready to provide specialized care at the birth of the child.
Anomalies of the development of the gastrointestinal tract
The most common pathology of the development of the digestive tract is duodenal atresia. In this case, on an ultrasound, the doctor sees round structures similar to cysts in the upper part of the fetal abdomen. If the cyst is located on the left, it is an enlarged stomach, on the right - the duodenum. This is the so-called “double bubble” sign. Very often the pathology is combined with polyhydramnios, anomalies of the heart, kidneys, and central nervous system.
Diagnosis of small bowel atresia is difficult. In the upper part of the fetal abdomen, the doctor sees cystic structures - overstretched loops of the small intestine. As a rule, fetal pathology is detected in the middle of pregnancy or at a later stage. With high atresia, polyhydramnios is usually diagnosed. Colonic atresia is almost impossible to diagnose using ultrasound.
Pathology of development of the anterior abdominal wall
The most commonly diagnosed defect in this group is an anterior abdominal wall defect - omphalocele. In the hernial sac, formed by the amniotic membrane and the parietal peritoneum, intestinal loops, part of the liver, stomach and spleen are found.
Other pathology is mainly localized in the right periumbilical region (gastroschisis) and is usually isolated. Only intestinal loops that are not covered by the amniotic membrane prolapse through this defect.
Ascites in the fetus
Free fluid is visualized on ultrasound as an anechoic zone surrounding the internal organs of the unborn child. If ascites is suspected, the doctor must carefully examine the fetus and evaluate its anatomy to exclude combined defects. The urinary system must be carefully examined, as ascitic fluid may be urine. If the unborn child has thickened skin or fluid is contained in at least two natural cavities, they speak of hydrops fetalis.
Its reasons are:
- Rhesus conflict;
- congenital heart defects;
- arrhythmias;
- obstruction of blood or lymphatic vessels.
To find out the exact cause of dropsy, the doctor will recommend an additional expert ultrasound to the woman.
Abnormalities of the urinary system
Some congenital defects of the urinary system are incompatible with life. If such a pathology is detected in the early stages, the doctor may advise the woman to terminate the pregnancy. If the anomaly was diagnosed late, the doctor may change the pregnancy management tactics.
Diagnosing agenesis, or absence of kidneys, is difficult due to the significant enlargement of the adrenal glands. In the last weeks of pregnancy, these glands can take on a bean-shaped shape, which makes diagnosis even more difficult. The bladder is small or absent altogether. To make an accurate diagnosis, you need to examine the fetus in several planes. Measuring the kidneys during an ultrasound helps to identify hypoplasia - underdevelopment of the organ.
Obstruction, hydronephrosis is manifested by dilation of the renal pelvis. However, it must be borne in mind that the expansion of the renal pelvis may be transient. Such dilations are most often bilateral and disappear after some time. If hydronephrosis is suspected, an ultrasound scan should be repeated after two to three weeks.
Pathological bilateral obstruction of the urinary system is usually combined with oligohydramnios and has a poor prognosis. If the obstruction is unilateral, the amount of amniotic fluid remains within normal limits.
With a multicystic kidney, ultrasound will reveal several cysts of varying diameters. They are located diffusely, less often in one part of the organ. Renal parenchyma can be detected between the cysts, although it is not clearly visualized. Autosomal recessive polycystic kidney disease is diagnosed in the third trimester of pregnancy. In such situations, there is a family history and oligohydramnios. On ultrasound, the kidneys are enlarged in size and their echogenicity is sharply increased.
Amniotic fluid
The most common causes of polyhydramnios are:
- high obstruction of the digestive tract;
- neural tube pathology;
- hydrops fetalis;
- defects of the anterior abdominal wall;
- skeletal dysplasia of the chest;
- development of several embryos simultaneously;
- diabetes mellitus in the mother.
The causes of oligohydramnios are:
- bilateral renal anomaly;
- damage to the amniotic membranes with leakage of water;
- intrauterine growth retardation;
- post-term pregnancy;
- antenatal fetal death;
- intrauterine developmental delay;
- post-term pregnancy;
- intrauterine embryonic death.
Oligohydramnios with bilateral renal anomalies is a poor prognostic sign.