If an ultrasound examination reveals markers of fetal chromosomal pathology
- Dear patients, first of all, we ask you to remember the most important thing: if markers (signs) of chromosomal pathology of the fetus were found during an ultrasound examination, this does not mean that the fetus has a chromosomal pathology, and the pregnancy must be terminated.
- All women who have been found to have ultrasound markers of chromosomal pathology of the fetus are offered invasive prenatal diagnostics - today, depending on the stage of pregnancy, we offer three types of invasive diagnostics: chorionic villus aspiration (performed at 11-14 weeks), amniocentesis (16-18 weeks), cordocentesis (19-20 weeks). More information about invasive diagnostic methods can be found at this link.
The most common ultrasound markers of chromosomal abnormalities are:
Increase in TVP.
This parameter is assessed at the first screening ultrasound (11-14 weeks)
TVP (thickness of the collar space) may be greater than normal for several reasons.
Why may the fetus exhibit an increase in TVP?
Parents are extremely excited and want to immediately get answers to all the questions they have - what is involved, what to do, and many others. Questions that cannot be answered immediately. After all, there are many reasons for the increase in TVP. This finding can occur in completely healthy fetuses; this is not a developmental defect, it is only a signal for a more in-depth examination, because such a feature can occur in fetuses with chromosomal abnormalities, heart abnormalities, or other congenital or hereditary diseases. When increasing the maximum TVP threshold, it is IMPORTANT that the doctor evaluates all other ultrasound markers (signs) and also conducts a detailed assessment of the fetal anatomy. Perhaps the reason for the increase in TVP lies in a violation of fetal development (for example, abnormalities in the structure of the heart).
What to do if an increase in TVP is detected in the fetus?
If your fetus is diagnosed with an enlarged TVP, you will definitely be referred for a consultation with a geneticist, who, after collecting an anamnesis, assessing all the risks, will give recommendations on additional research methods (invasive diagnostics). Next, an expert ultrasound of the fetus will be required at 20 weeks for a detailed assessment of the anatomy. If all these studies do not reveal any deviations, then the chances of giving birth to a healthy child are high even with a significant amount of TVP.
Hypoplasia/aplasia of the nasal bones.
Hypoplasia of the nasal bones is a reduction in the size of the nasal bone depending on the CTE of your baby.
Aplasia of the nasal bones is the lack of visualization of your baby's nasal bone.
The lack of visibility of the bony part of the nasal dorsum in the fetus or its underdevelopment (not bright enough) at the first screening is associated with delayed calcium deposition. This situation may be somewhat more common in fetuses with Down syndrome, but it is important that:
- the absence of nasal bones on ultrasound is not a developmental anomaly in itself; can occur in completely healthy fetuses (in 3% of cases);
- to assess the degree of individual risk, it is necessary to evaluate the remaining ultrasound markers (thickness of the fetal nuchal translucency, blood flow indicators on the heart valve, blood flow indicators in the ductus venosus, fetal heart rate) and biochemical analysis of maternal serum (PAPP-A, hCG);
- If the result of a combined screening (evaluation of ultrasound and blood test data in a special program) shows a LOW risk of chromosomal pathology, there is no need to worry. Be sure to undergo a follow-up ultrasound at 19-20 weeks of pregnancy, where a thorough assessment of the fetal anatomy will be carried out and certain ultrasound markers of the second trimester of pregnancy will be examined.
- What to do if the combined screening result is HIGH? – There’s no need to worry. You will definitely be referred for a consultation with a geneticist, who, having collected an anamnesis, assessed all the risks, will give recommendations on additional research methods (invasive diagnostics).
Hyperechoic intestine.
This is a term that refers to increased echogenicity (brightness) of the intestine on an ultrasound image. The finding of hyperechoic bowel NOT a malformation of the bowel, but simply reflects the nature of its ultrasound image. It must be remembered that the echogenicity of the normal intestine is higher than the echogenicity of its neighboring organs (liver, kidneys, lungs), but such intestine is not considered hyperechoic. Only intestines whose echogenicity is comparable to the echogenicity of fetal bones are called hyperechoic.
Why can the fetal intestine be hyperechoic?
Sometimes hyperechoic intestine is detected in completely normal fetuses, and this sign may disappear with dynamic ultrasound. Increased echogenicity of the intestine may be a manifestation of chromosomal diseases of the fetus, in particular Down syndrome. Therefore, when hyperechoic bowel is detected, a careful assessment of fetal anatomy is performed. However, if a hyperechoic intestine is detected, we can only talk about an increased risk of Down syndrome, since such changes can also occur in completely healthy fetuses. Sometimes hyperechoic bowel may be a sign of intrauterine fetal infection. Hyperechoic bowel is often found in fetuses with intrauterine growth restriction. However, this will necessarily reveal a lag in the size of the fetus from the gestational age, oligohydramnios, and impaired blood flow in the vessels of the fetus and uterus. If none of the above is detected, then the diagnosis of fetal growth restriction is excluded.
What to do if hyperechoic intestine is detected in the fetus?
You should contact a genetic specialist who will once again evaluate the results of biochemical screening and give the necessary recommendations for further management of pregnancy.
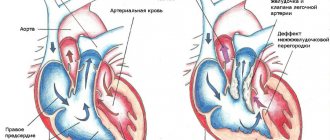
Hyperechoic focus in the ventricle of the heart.
This is a term that refers to the increased echogenicity (brightness) of a small area of the heart muscle on an ultrasound image. Identification of a hyperechoic focus in the heart NOT a cardiac malformation, but simply reflects the nature of its ultrasound image. A hyperechoic focus occurs at the site of increased deposition of calcium salts on one of the heart muscles, which does not interfere with the normal functioning of the fetal heart and does not require any treatment.
Why can a fetus have a hyperechoic focus in the heart?
Sometimes a hyperechoic focus in the heart is detected in completely normal fetuses, and this sign may disappear with dynamic ultrasound. The presence of a hyperechoic focus in the fetal heart may be a manifestation of fetal chromosomal diseases, in particular Down syndrome. In this regard, when a hyperechoic focus is detected, a careful assessment of the fetal anatomy is carried out. However, this marker refers to the “small” markers of Down syndrome, therefore, identifying only a hyperechoic focus in the heart does not increase the risk of having Down syndrome and is not an indication for other diagnostic procedures.
What to do if a hyperechoic focus is detected in the fetal heart?
If the fetus has ONLY a hyperechoic focus in the heart, then no additional examinations are required; the risk of Down's disease does not increase. At a planned ultrasound at 32-34 weeks, the fetal heart will be examined again. In most cases, the hyperechoic focus in the heart disappears by this stage of pregnancy, but even if it continues to remain in the heart, this does not in any way affect the health of the fetus and the management of pregnancy.
The only artery of the umbilical cord.
A normal umbilical cord consists of three vessels - two arteries and one vein. Sometimes, instead of two arteries, only one artery and one vein are formed in the umbilical cord, thus, only two vessels are identified in the umbilical cord. This condition is considered a malformation of the umbilical cord, but this defect does not have any effect on the postpartum condition of the child and its further development.
Why can a single umbilical cord artery be identified in a fetus?
Sometimes a single umbilical cord artery is identified in completely normal fetuses; After the birth of a child, this fact does not have any impact on its further development. Sometimes a single umbilical cord artery is combined with defects of the fetal cardiovascular system, therefore, when a single umbilical cord artery is identified, a detailed examination of the anatomy of the fetus and, in particular, the cardiovascular system is carried out. In the absence of other malformations, a single umbilical cord artery is able to provide adequate blood flow to the fetus. Somewhat more often, a single umbilical cord artery is detected in fetuses with Down syndrome and other chromosomal diseases. However, this marker is a “minor” marker of Down syndrome, so identifying only a single umbilical cord artery does not increase the risk of Down syndrome and is not an indication for other diagnostic procedures. A single umbilical cord artery sometimes leads to intrauterine growth retardation. In this regard, if a single umbilical cord artery is detected, an additional ultrasound is recommended at 26-28 weeks of pregnancy, and a planned one at 32-34 weeks. If a lag in the size of the fetus from the gestational age or disruption of blood flow in the vessels of the fetus and uterus is not detected, then the diagnosis of fetal growth retardation is excluded.
What to do if a single umbilical cord artery is identified in the fetus?
Identification of only a single umbilical cord artery does not increase the risk of Down syndrome and is not an indication for genetic counseling or other diagnostic procedures. A control ultrasound is required at 26-28 and 32 weeks of pregnancy to assess the rate of fetal growth and evaluate its functional state.
Choroid plexus cysts (CPC).
The choroid plexus is one of the first structures to appear in the fetal brain. It is a complex structure, and the presence of both choroid plexuses confirms that both halves develop in the brain. The choroid plexus produces fluid that nourishes the brain and spinal cord. Sometimes the fluid forms collections inside the choroid plexus, which appear as a “cyst” on ultrasound. Choroid plexus cysts can sometimes be found on ultrasound between 18 and 22 weeks of pregnancy. The presence of cysts does not affect the development and function of the brain. Most cysts disappear spontaneously by 24-28 weeks of pregnancy.
Are choroid plexus cysts common?
In 1-2% of all normal pregnancies, the fetuses have CSS, in 50% of cases bilateral choroid plexus cysts are found, in 90% of cases the cysts spontaneously disappear by the 26th week of pregnancy, the number, size, and shape of cysts can vary, cysts are also found in healthy children and adults. Somewhat more often, choroid plexus cysts are detected in fetuses with chromosomal diseases, in particular with Edwards syndrome (trisomy 18, extra chromosome 18). However, with this disease, the fetus will always have multiple malformations, so identifying only choroid plexus cysts does not increase the risk of having trisomy 18 and is not an indication for other diagnostic procedures. In Down syndrome, choroid plexus cysts are usually not detected. The risk of Edwards syndrome when CSS is detected does not depend on the size of the cysts and their unilateral or bilateral location. Most cysts resolve by 24-28 weeks, so a control ultrasound is performed at 28 weeks. However, if choroid plexus cysts do not disappear by 28-30 weeks, this does not affect the further development of the child.
Enlargement of the renal pelvis (pyelectasia).
The renal pelvis is the cavity where urine from the kidneys collects. From the pelvis, urine moves to the ureters, through which it enters the bladder.
Pyeelectasia is an enlargement of the renal pelvis. Pyeelectasis is 3-5 times more common in boys than in girls. Both unilateral and bilateral pyeloectasia occur. Mild forms of pyelectasis often go away on their own, while severe forms sometimes require surgical treatment.
The cause of dilation of the renal pelvis in the fetus.
If there is an obstacle in the way of the natural outflow of urine, urine will accumulate above this obstacle, which will lead to expansion of the renal pelvis. Pyeelectasis in the fetus is diagnosed by routine ultrasound examination at 18-22 weeks of pregnancy.
Is pyeelectasis dangerous?
Moderate expansion of the renal pelvis, as a rule, does not affect the health of the unborn child. In most cases, during pregnancy, spontaneous disappearance of moderate pyelectasis is observed. Severe pyelectasis (more than 10 mm) indicates a significant difficulty in the outflow of urine from the kidney. Difficulty in the outflow of urine from the kidney may increase, causing compression, atrophy of the kidney tissue and decreased kidney function.
In addition, a violation of the outflow of urine is often accompanied by the addition of pyelonephritis, an inflammation of the kidney that worsens its condition. Slightly more often, dilation of the renal pelvis is detected in fetuses with Down syndrome. However, this marker refers to the “minor” markers of Down syndrome, therefore, detecting only dilation of the renal pelvis does not increase the risk of having Down syndrome and is not an indication for other diagnostic procedures. The only thing you need to do before giving birth is to undergo a control ultrasound at 32 weeks and once again assess the size of the renal pelvis.
Is it necessary to examine the baby after birth?
In many children, moderate pyelectasis disappears spontaneously as a result of the maturation of the urinary system after the birth of the child. For moderate pyelectasis, it may be sufficient to conduct regular ultrasound examinations every three months after the birth of the child. If a urinary infection occurs, antibiotics may be necessary. As the degree of pyelectasis increases, a more detailed urological examination is necessary.
In cases of severe pyelectasis, if the dilation of the pelvis progresses and a decrease in kidney function occurs, surgical treatment is indicated. Surgery can remove the obstruction to the flow of urine. Some surgical interventions can be successfully performed using endoscopic methods - without open surgery, using miniature instruments inserted through the urethra. In any case, the issue of surgical treatment is decided after the birth of the child and its complete examination.
What to do if ultrasound markers of chromosomal pathology are detected in the fetus?
You should contact a genetic specialist who will once again evaluate the results of ultrasound and biochemical screening, calculate the risk individually for your case and give the necessary recommendations for further management of pregnancy.
GEF in the ventricles of the fetal heart: medical tactics
In most cases, if a “golf ball” is detected in the area of the child’s heart, it is necessary to continue observation: a control ultrasound examination during pregnancy should be performed by a certified diagnostician using a modern 3D device. If there is a suspicion of chromosomal abnormalities in the fetus, one must agree to invasive research methods.
After the birth of a child, it is important in the first days and during the first years of the baby’s life to be regularly examined by a pediatrician and cardiologist.
Detection of any changes in the baby’s heart is a significant reason for a careful assessment of the child’s intrauterine development.