The heart is a muscular pump that ensures continuous movement of blood through the vessels. Together, the heart and blood vessels make up the cardiovascular system. This system consists of the systemic and pulmonary circulation. From the left side of the heart, blood first moves through the aorta, then through large and small arteries, arterioles, and capillaries. In the capillaries, oxygen and other substances necessary for the body enter the organs and tissues, and from there carbon dioxide, metabolic products, are removed. After this, the blood turns from arterial to venous and again begins to move towards the heart. First along the venules, then through smaller and larger veins. Through the inferior and superior vena cava, blood again enters the heart, only this time into the right atrium. A large circle of blood circulation is formed.
Venous blood from the right side of the heart is sent through the pulmonary arteries to the lungs, where it is enriched with oxygen, and returns to the heart again - this is the pulmonary circulation.
Inside, the heart is divided by partitions into four chambers. The two atria are divided by the interatrial septum into the left and right atria. The left and right ventricles of the heart are separated by the interventricular septum. Normally, the left and right parts of the heart are completely separate. The atria and ventricles have different functions. The atria store blood that flows into the heart. When the volume of this blood is sufficient, it is pushed into the ventricles. And the ventricles push blood into the arteries, through which it moves throughout the body. The ventricles have to do more hard work, so the muscle layer in the ventricles is much thicker than in the atria. The atria and ventricles on each side of the heart are connected by the atrioventricular orifice. Blood moves through the heart in only one direction. In the systemic circle of blood circulation from the left side of the heart (left atrium and left ventricle) to the right, and in the small circle from the right to the left.
The correct direction of blood flow is ensured by the valve apparatus of the heart:
Valves:
- tricuspid
- pulmonary
- mitral
- aortic
They open at the right time and close, preventing blood flow in the opposite direction.
Aortic valve
Closes the entrance to the aorta. It also consists of three valves, which look like crescents. Opens when the left ventricle contracts. In this case, blood enters the aorta. When the left ventricle relaxes, it closes. Thus, venous blood (poor in oxygen) from the superior and inferior vena cava enters the right atrium. When the right atrium contracts, it moves through the tricuspid valve into the right ventricle. Contracting, the right ventricle ejects blood through the pulmonary valve into the pulmonary arteries (pulmonary circulation). Enriched with oxygen in the lungs, the blood turns into arterial blood and moves through the pulmonary veins to the left atrium, then to the left ventricle. When the left ventricle contracts, arterial blood enters the aorta through the aortic valve under high pressure and spreads throughout the body (systemic circulation).
The heart muscle is called the myocardium
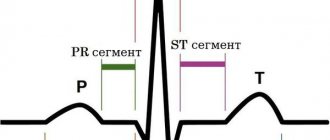
There are contractile and conductive myocardium. The contractile myocardium is the actual muscle that contracts and produces the work of the heart. In order for the heart to contract in a certain rhythm, it has a unique conduction system. The electrical impulse to contract the heart muscle occurs in the sinoatrial node, which is located in the upper part of the right atrium and spreads through the conduction system of the heart, reaching every muscle fiber
First, both atria contract, then both ventricles, thereby ensuring the flow of blood to all organs and tissues of the body. The heart muscle has two membranes (external and internal). The inner lining of the heart is called the endocardium. The outer lining of the heart is called the pericardium.
Conduction system of the heart
The heart, like any organ, has its own nervous system. The nervous system of the heart has several levels. The first and main pacemaker of the heart is the sinus node, located in the right atrium. It is subject to the atrioventricular node, which is located on the border between the atria and ventricles and quite often slows down the heart rate set by the sinus node. Then the nerve impulse goes to the ventricles of the heart along the branches of the Hiss bundle, which are divided into the smallest nerve endings - Purkinje fibers.
Ventricular extrasystole - symptoms and treatment
Once ventricular extrasystoles are detected in a patient, treatment should be selected taking into account the symptoms and the presence of dangerous types of extrasystoles.
The tactics for managing patients with ventricular extrasystole are as follows:
- observation without prescribing medications for patients with benign PVC, which is subjectively well tolerated (it is recommended to change lifestyle, eat a balanced diet, eliminate factors that provoke arrhythmia, adjust physical activity, etc.);
- in case of functional ventricular extrasystole (extrasystole caused by non-cardiac diseases) and extrasystole associated with heart pathologies, drug therapy is prescribed aimed at treating the underlying disease;
- treatment with antiarrhythmic drugs;
- the use of surgical treatment (radiofrequency ablation of the arrhythmogenic area of the myocardium, heart transplantation).
There are several main areas of treatment depending on the course, form and severity of PVCs.
1. If a person has no complaints, and the study reveals rare single monomorphic premature ventricular complexes that do not cause hemodynamic disturbances, no special therapy is required. In this case, the patient should give up caffeine-containing and alcoholic drinks, eliminate smoking, establish a daily routine, and ensure adequate sleep and rest. If there are any dysfunctions of the body associated with insufficient mobility, you need to increase physical activity in accordance with the body's capabilities. At the same time, it is necessary to exclude excessive physical activity (weight lifting, weightlifting). Your diet should include foods rich in potassium and magnesium: they have a beneficial effect on the cardiovascular system.
| Products containing potassium | Products containing magnesium |
| ⠀•⠀dried apricots; ⠀•⠀cocoa powder; ⠀•⠀wheat bran; ⠀•⠀raisins; ⠀•⠀sunflower seeds; ⠀•⠀nuts (pine nuts, almonds, peanuts, walnuts); ⠀•⠀legumes (peas, lentils, beans); ⠀•⠀jacket potatoes; ⠀•⠀avocado; ⠀•⠀ceps; ⠀•⠀bananas; ⠀•⠀citrus fruits; ⠀•⠀Brussels sprouts and kohlrabi; ⠀•⠀milk and fermented milk products; ⠀•⠀cereals (oatmeal, buckwheat, pearl barley, rice); ⠀•⠀fruits (peaches, pears, watermelon, apples, prunes, apricots, melon); ⠀•⠀chicory; ⠀•⠀vegetables (carrots, spinach, green onions, eggplant, cucumbers); ⠀•⠀chicken eggs; ⠀•⠀fish and meat; ⠀•⠀apple juice. | ⠀•⠀oil (sesame, flaxseed, peanut); ⠀•⠀cheese (Dutch, Poshekhonsky, goat, with mold); ⠀•⠀cottage cheese (low-fat and low-fat, curd cheese); ⠀•⠀bitter chocolate; ⠀•⠀almost all types of meat; ⠀•⠀fish (halibut, sturgeon, perch, haddock, cod, saury); ⠀•⠀duck eggs; ⠀•⠀cereals (rolled oats, chickpeas, peas, buckwheat, brown rice, lentils); ⠀•⠀fruits and berries (cherries, kiwi, pineapple, feijoa, raspberries, pears, peach, persimmon); ⠀•⠀many varieties of tea (for example, “Ivan-tea”) and juices; ⠀•⠀ginger; ⠀•⠀mustard; ⠀•⠀vanilla. |
2. When attacks of extrasystole are detected, which are accompanied by clinical symptoms, but do not disturb hemodynamics and have a benign course, beta-blockers (Bisoprolol, Metoprolol) are first prescribed. Sometimes, especially with functional ventricular arrhythmia against the background of vegetative-vascular dystonia and stressful conditions, drugs with sedative (Valemidin, Valerian) and anti-anxiety effects (Stresam, Adaptol), magnesium preparations (Magnerot) help in complex treatment , "Magne B6 forte"). It must be emphasized that the number of PVCs is taken into account when determining the degree of its malignancy. Frequent (up to 1000 or more per day) ventricular extrasystole in itself, even in the absence of obvious heart disease, is an indication for antiarrhythmic therapy.
Frequent PVCs and the appearance of paired, polytopic extrasystoles disrupt the movement of blood through the vessels, therefore, to reduce the risk of ventricular fibrillation and cardiac arrest, antiarrhythmic drugs are prescribed. It is preferable to use class I antiarrhythmics, and only if they are ineffective - Amiodarone or Sotalol. In parallel, drugs must be used to treat the underlying disease that caused the extrasystole[10]. To assess the results of treatment, as a rule, daily ECG monitoring is performed. A decrease in the number of PVCs by 75-80% indicates the effectiveness of therapy.
3. For PVCs of a malignant nature, it is necessary to prescribe highly effective drugs, such as Amiodarone and Sotalol. Sometimes they are combined with maintenance doses of beta-blockers. Treatment is usually carried out in a hospital setting, under ECG monitoring. In the hospital there are more opportunities to adjust hemodynamics and significantly reduce the risk of death in patients with cardiac arrhythmias.
Class I antiarrhythmics should not be taken if the patient has the following pathologies:
- severe signs of heart failure (low ejection fraction according to echocardiography);
- acute forms of coronary heart disease (acute infarction, progressive angina);
- previous myocardial infarction (especially if it was less than 6-12 months old);
- angina pectoris of functional classes III and IV (especially with proven coronary atherosclerosis);
- severe hypertrophy of the left ventricle with a thickness of more than 14 mm and/or the right ventricle (according to echocardiography);
- chronic heart failure class III-IV according to NYHA (New York Heart Association) and/or left ventricular ejection fraction less than 35%;
- pronounced dilatation (expansion of the chamber) of the left ventricle, cardiomegaly;
- active myocarditis;
- bundle branch block;
- severe bradycardia, etc.
If the patient does not have these contraindications and has moderately severe heart pathology, then the use of class I drugs can be considered [10]. It should be noted that antiarrhythmic drugs can have a proarrhythmic effect, i.e. cause a more dangerous arrhythmia, so only a doctor can prescribe them and only with appropriate indications.
Work has appeared that has shown the possibility of a beneficial effect of Omacor on ventricular arrhythmia, in particular in patients with coronary heart disease and chronic heart failure [6]. The addition of this drug to antiarrhythmics increases the effectiveness of treatment of ventricular arrhythmias. If the problem is associated with an electrolyte imbalance, then the patient is prescribed Magnesium sulfate or Potassium chloride.
The question of the duration of antiarrhythmic therapy is practically important. In patients with malignant ventricular arrhythmias, antiarrhythmic therapy should be continued indefinitely, in most cases for life. For less malignant rhythm disturbances, treatment should continue for up to several months with the possibility of gradual (due to the danger of rebound syndrome) its withdrawal. After stopping continuous therapy, the patient is advised to always carry a successfully used antiarrhythmic with him and take it in case of resumption of cardiac dysfunction.
4. For ventricular extrasystole, surgical treatment is possible. Indications for surgical intervention are:
- frequent (from several thousand to 20-30 thousand per day) ventricular extrasystole with an identified arrhythmogenic focus;
- ineffectiveness or impossibility of long-term use of antiarrhythmics in combination with poor tolerability or poor prognosis.
The high activity of the lesion makes it possible to detect it when drawing up a map of the electrical activity of the heart and perform radiofrequency ablation (RFA) of this myocardial zone[11]. The essence of the RFA technique is that a catheter is inserted into the patient through a large-caliber vessel, which is guided under the control of equipment to the very heart. First, using a special technique, the focus of pathological impulses is diagnosed, and then the site of ectopic excitation is exposed to a radiofrequency pulse, which leads to its destruction.
It is also possible to install an electrical pacemaker (ECS). The pacemaker is a device with electrodes that are attached to the ventricle and atrium during surgery. The electrodes create electronic impulses that cause the myocardium to contract. A pacemaker essentially replaces the sinus node, which is responsible for rhythm. It relieves a person from extrasystole and allows him to return to a full life.
In acute and chronic coronary heart disease, the development of ventricular arrhythmia is directly related to myocardial ischemia. In this regard, surgical myocardial revascularization (stenting, coronary artery bypass grafting) can improve electrical stability and reduce the likelihood of developing ventricular arrhythmias.
In patients with a high risk of sudden death and congestive heart failure, heart transplantation remains the main treatment option.