The medical term “vascular genesis” arose from the religious doctrine of genesis (origin, origin). The meaning is tied to the causes and mechanisms of development of diseases of the arteries and veins of the brain.
Through arterial vessels, blood comes from the carotid and vertebral arteries. And veins form a system for the outflow of waste waste from cells and intercellular space.
Any vascular disorders entail more or less severe changes in the functioning of the brain (diffuse and focal).
How should blood vessels work?
Inside the brain, blood circulation is maintained through the circles of Willis and spino-vertebral circles. The largest branches of the cerebral arteries extend to the cortex and subcortical white matter of the hemispheres:
- front,
- average,
- rear
There are anastomoses between the branches that form an auxiliary collateral supply if for some reason the main arterial trunks fail.
This organization of the vascular structure makes it possible to compensate at first for the lack of blood supply when the main arteries are damaged.
The gray matter of the brain is equipped with 4–5 times more blood vessels than the white matter (especially layers III, IV and V of the cortex). Small capillaries ensure constant intense metabolism in neurons.
The outflow begins from the venous part of the capillaries and goes to the venous sinuses, then to the jugular and superior vena cava. It is important that excess fluid from the ventricles is discharged along this path. Difficulties of venous origin can cause increased intracranial pressure and hydrocephalus.
Blood supply areas are divided by lobes and brain structures
Demyelinating disease of the central nervous system
Demyelinating diseases of the brain and spinal cord are pathological processes that lead to the destruction of the myelin sheath of neurons and disruption of the transmission of impulses between nerve cells of the brain. It is believed that the etiology of diseases is based on the interaction of the body's hereditary predisposition and certain environmental factors. Impaired impulse transmission leads to a pathological state of the central nervous system.
What diseases are these?
There are the following types of demyelinating diseases:
- Multiple sclerosis is a demyelinating disease of the central nervous system. The demyelinating disease multiple sclerosis is the most common pathology. Multiple sclerosis is characterized by a variety of symptoms. The first symptoms appear at the age of 20-30 years, women are more often affected. Multiple sclerosis is diagnosed by the first signs, which were first described by psychiatrist Charcot - involuntary oscillatory eye movements, trembling, scanned speech. Patients also experience urinary retention or very frequent urination, absence of abdominal reflexes, pallor of the temporal halves of the optic discs;
- ADEM, or acute disseminated encephalomyelitis. It begins acutely and is accompanied by severe cerebral disorders and manifestations of infection. The disease often occurs after exposure to a bacterial or viral infection and may develop spontaneously;
- diffuse disseminated sclerosis. It is characterized by damage to the spinal cord and brain and manifests itself in the form of convulsive syndrome, apraxia, and mental disorders. Death occurs within a period of 3 to 6-7 years from the moment the disease is diagnosed;
- Devic's disease, or acute neuromyelitis optica. The disease begins as an acute process, is severe, and progresses, affecting the optic nerves, which causes complete or partial loss of vision. In most cases, death occurs;
- Balo's disease, or concentric sclerosis, periaxial concentric encephalitis. The onset of the disease is acute, accompanied by fever. The pathological process occurs with paralysis, visual disturbances, and epileptic seizures. The course of the disease is rapid - death occurs within a few months;
- leukodystrophies - this group contains diseases that are characterized by damage to the white matter of the brain. Leukodystrophies are hereditary diseases; as a result of a gene defect, the formation of the myelin sheath of the nerves is disrupted;
- Progressive multifocal leukoencephalopathy is characterized by decreased intelligence, epileptic seizures, the development of dementia and other disorders. The patient's life expectancy is no more than 1 year. The disease develops as a result of decreased immunity, activation of the JC virus (human polyomavirus 2), often found in patients with HIV infection, after bone marrow transplantation, in patients with malignant blood diseases (chronic lymphocytic leukemia, Hodgkin's disease);
- diffuse periaxial leukoencephalitis. A hereditary disease that most often affects boys. Causes visual, hearing, speech, and other disorders. Progresses quickly - life expectancy is just over a year;
- Osmotic demyelination syndrome is very rare and develops as a result of electrolyte imbalance and a number of other reasons. A rapid increase in sodium levels leads to the loss of water and various substances from brain cells, causing the destruction of the myelin sheaths of nerve cells in the brain. One of the posterior parts of the brain is affected - the Varoliev bridge, which is most sensitive to myelinolysis;
- myelopathy is a general term for lesions of the spinal cord, the causes of which are varied. This group includes: tabes dorsalis, Canavan disease, and other diseases. Canavan disease is a genetic, neurodegenerative autosomal recessive disease that affects children and causes damage to nerve cells in the brain. The disease is most often diagnosed in Ashkenazi Jews living in Eastern Europe. Tabes dorsalis (locomotor ataxia) is a late form of neurosyphilis. The disease is characterized by damage to the posterior columns of the spinal cord and spinal nerve roots. The disease has three stages of development with a gradual increase in symptoms of damage to nerve cells. Coordination when walking is impaired, the patient easily loses balance, bladder function is often disrupted, pain appears in the lower limb or lower abdomen, and visual acuity decreases. The most severe third stage is characterized by loss of sensitivity of muscles and joints, areflexia of the tendons of the legs, development of astereognosis, the patient cannot move;
- Guillain-Barré syndrome - occurs at any age, refers to a rare pathological condition that is characterized by damage to the peripheral nerves of the body by its own immune system. In severe cases, complete paralysis occurs. In most cases, patients recover completely with adequate treatment;
- neural amyotrophy of Charcot-Marie-Tooth. A chronic hereditary disease, which is characterized by progression, affects the peripheral nervous system. In most cases, the myelin sheath of nerve fibers is destroyed; there are forms of the disease in which pathology of the axial cylinders in the center of the nerve fiber is detected. As a result of damage to the peripheral nerves, tendon reflexes fade and atrophy of the muscles of the lower and then upper extremities occurs. The disease belongs to progressive chronic hereditary polyneuropathies. This group includes: Refsum's disease, Roussy-Lévy syndrome, Dejerine-Sotta hypertrophic neuropathy and other rare diseases.
Genetic diseases
When damage to nerve tissue occurs, the body responds by destroying myelin. Diseases that are accompanied by the destruction of myelin are divided into two groups - myelinoclastics and myelinopathy. Myelinoclasty is the destruction of the membrane under the influence of external factors.
Myelinopathy is a genetically determined destruction of myelin associated with a biochemical defect in the structure of the neuron membrane. At the same time, this distribution into groups is considered conditional - the first manifestations of myelinoclasty may indicate a person’s predisposition to the disease, and the first manifestations of myelinopathy may be associated with damage caused by external factors.
Multiple sclerosis is considered a disease of people with a genetic predisposition to the destruction of the membrane of neurons, metabolic disorders, a deficient immune system and the presence of a slow infection. Genetic demyelinating diseases include: neural amyotrophy of Charcot-Marie-Tooth, hypertrophic neuropathy of Dejerine-Sottas, diffuse periaxial leukoencephalitis, Canavan disease and many other diseases. Genetic demyelinating diseases are less common than autoimmune demyelinating diseases.
What happens to the vessels?
The arteries are the most frequently damaged. Changes occur suddenly (acute) or develop over many years (chronic). Histological examination reveals:
- hyperplasia (growth) of the inner membrane;
- decrease in elastic properties due to loss of corresponding fibers in the wall structure;
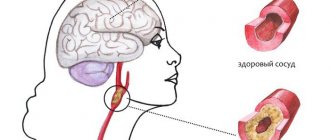
- atherosclerotic plaques at different stages of development;
- intravascular thrombi and emboli;
- aneurysmal dilatations with the formation of cysts;
- rupture of arteries and veins with the formation of hematomas;
- inflammation of the walls (vasculitis).
The study of autoallergy processes in systemic collagenoses and diathesis revealed changes in brain tissue and blood vessels of an allergic nature caused by antibody complexes.
Coronary angiography with contrast agent revealed:
- congenital or post-traumatic changes in the form of hypoplasia (underdevelopment);
- atypical location and direction;
- a decrease in the diameter of the arteries, complicating the development of anastomoses;
- dependence of blood flow on mechanical obstacles formed by tumors and compression.
Veins most often suffer from phlebitis and thrombosis. They are a consequence of head injuries. They develop due to ascending thrombus formation or compression of the jugular and superior vena cava. The inflammatory process often passes from the paranasal sinuses during sinusitis, frontal sinuses, aggravating the underlying disease.
It is important to understand that focal damage to cerebral vessels may not be caused by local damage (as in trauma), but by a general disease affecting different organs and the genesis of blood cells.
Diagnostics of NMC
- Duplex ultrasound examination of blood vessels.
- Contrast venography, angiography.
- CT, MRI.
- Transcranial Doppler.
- Laboratory tests - clinical, biochemical blood tests with determination of lipid profile, hematocrit.
- Fundus examination.
- Detection of hearing loss, smell, taste, and pathology of the vestibular apparatus.
What morphological consequences cause vascular changes?
Changes in the arterial bed are always accompanied by a narrowing of the lumen of blood vessels. This can be atherosclerotic plaques, spasm, proliferation of membranes, blood clots. As a result, the brain does not receive enough oxygen and nutrients. Impaired blood supply leads to ischemia of individual areas.
If the pathology develops acutely, then the collaterals do not have time to fully open and take over the compensation of focal needs. Ischemic damage is characterized by loss of adenosine triphosphoric acid and phosphocreatinine in tissues, which reduces the excitability of cortical cells and deprives them of energy.
In chronic pathology, the process of ischemia occurs more slowly, which makes it possible to protect neurons with medications and develop auxiliary blood circulation.
Clinically it looks like:
- transient cerebrovascular accident;
- acute ischemic stroke;
- chronic brain failure.
Rupture of a vessel due to injury or pressure surge leads to intracerebral hematoma (hemorrhagic stroke). It compresses neighboring areas of the brain and causes focal disorders.
Venous congestion contributes to increased intracranial pressure in the ventricles of the brain. This factor also leads to swelling and compression of tissue structures. Without treatment, loss of some functions of the brain nuclei is inevitable.
Development mechanisms
The nervous system consists of central and peripheral sections. The regulation mechanism between them works as follows: impulses from the receptors of the peripheral system are transmitted to the nerve centers of the spinal cord, and from there to the brain. The disruption of this complex mechanism causes demyelination.
Nerve fibers are covered with a myelin sheath. As a result of the pathological process under consideration, this membrane is destroyed and fibrous tissue is formed in its place. She, in turn, cannot conduct nerve impulses. In the absence of nerve impulses, the functioning of all organs is disrupted, since the brain cannot issue commands.
Causes of vascular problems
The genesis of vascular damage is inseparable from the mechanism of development of the underlying disease and provoking factors. The “impetus” for the onset of damage to the arteries of the brain can be:
- arterial hypertension and hypotension;
- diabetes mellitus with metabolic disorders;
- smoking and alcoholism, drugs;
- stressful situations;
- lipid and lipoprotein metabolism disorders, obesity;
- dystonia of the autonomic nervous system;
- tendency to weather dependence;
- traumatic brain injury;
- motor passivity.
Focal circulatory disorders are found in the brain when:
- systemic vasculitis;
- blood diseases;
- congenital and acquired heart diseases;
- aneurysmal vasodilation;
- cervical osteochondrosis.
Blood from a ruptured aneurysm squeezes the brain matter
Symptoms of blood supply problems
With insufficient nutrition of the brain, neurons begin to die. Since the latter are associated with neurology, the patient may experience irritability, fatigue, insomnia or interrupted sleep. Also, for this condition, depression is a common concomitant factor. If the disease progresses, the person may experience periods of severe excitability.
There is also a manifestation of egocentrism. With further development of the disease, indifference to anything and dementia occurs. Insufficient nutrition of brain cells can cause other more serious diseases. For example, a stroke. In our country, this disease occurs quite often. Not everyone can survive this disease. In addition, it can lead to various serious consequences both for the person himself and for his close circle. Epileptic seizures may also occur due to the fact that the brain does not receive enough nutrition.
How do vascular lesions of the brain manifest clinically?
Diseases of the brain of vascular origin, depending on the degree of damage to the arterial bed, can cause reversible (transient) symptoms or, using the body’s compensatory capabilities, form clinical manifestations that indicate the localization of the source of maximum destruction.
In ischemic brain disease, initial changes in nerve cells cause subtle disturbances in higher cortical functions:
- psyche;
- functioning of the sense organs;
- coordination of movements;
- vegetatives (sweating, tachycardia).
They are detected in cases of nervous overstrain, excitement, and stressful situations. Then the disorders take on a dyscirculatory character.
Headache may worsen with head movements or bending
The most common manifestations are:
- headaches - very intense and dull, localized in the back of the head, eyebrows or throughout the head;
- feeling of “noise in the head or ears”;
- dizziness;
- sensation of blood pulsating in the head;
- photophobia;
- nausea and vomiting;
- weakness in the left, right or all limbs;
- chilliness of hands and feet;
- difficulty speaking;
- visual impairment;
- memory disorder;
- insomnia.
Objective signs are:
- paresis and muscle paralysis;
- asymmetry of nasolabial folds;
- “sailing” breathing;
- pathological reflexes in the arms and legs.
In case of venous insufficiency, the patient additionally experiences:
- cyanotic tint of lips, nose, ears, cheeks;
- swollen lower eyelids;
- focal symptoms are less pronounced.
Headaches occur after night, when tilting the head (outflow worsens).
In severe cases:
- the patient is unconscious (cerebral coma);
- breathing is hoarse due to paresis of the respiratory muscles and vocal cords, arrhythmic;
- the face is purple and puffy (with a cerebral hemorrhage);
- focal symptoms depend on the location of the hematoma.
Classification
Demyelinating disease of the nervous system is classified into different types, which are based on the destruction of the myelin sheath. In this regard, the pathology under consideration is divided accordingly into multiple sclerosis, Marburg disease, Devic disease, progressive multifocal leukoencephalopathy and Guillain-Barré syndrome.
Multiple sclerosis
Multiple sclerosis is characterized as a severe chronic and immunodegenerative disease of the central nervous system, prone to progression. In most cases, the disease occurs at a young age and almost always leads to disability. This demyelinating disease of the central nervous system is assigned code G35 according to ICD-10.
Currently, the causes of the development of multiple sclerosis are not fully understood. Most scientists are inclined to the multifactorial theory of the development of this disease, when genetic predisposition and external factors are combined. The latter include:
- infectious diseases;
- state of chronic intoxication;
- taking certain medications;
- change of place of residence with a sharp change in climate;
- lack of fiber and high-calorie diet.
The progression of multiple sclerosis is characterized by the development of the following symptoms:
- sensory disturbances (goosebumps, numbness, tingling, burning, itching);
- visual impairment (impaired color rendering, decreased visual acuity, blurred picture);
- trembling of the limbs or torso;
- headache;
- speech disorders and difficulty swallowing;
- muscle spasms;
- gait changes;
- cognitive impairment;
- heat intolerance;
- dizziness;
- chronic fatigue;
- libido disturbance;
- anxiety and depression;
- stool instability;
- insomnia;
- autonomic disorders.
Treatment of multiple sclerosis is carried out using methods such as:
- plasmapheresis;
- taking cytostatics;
- prescription of immunosuppressants;
- use of immunomodulators;
- taking beta interferons;
- hormonal therapy.
- symptomatic therapy with the prescription of antioxidants, nootropic drugs and vitamins.
During the period of remission, patients are prescribed sanatorium treatment, massage, and physical therapy. In this case, all thermal procedures should be excluded. To alleviate the symptoms of the disease, medications are prescribed: those that reduce muscle tone, eliminate tremors, normalize urination, stabilize the emotional background, and anticonvulsants.
Marburg disease
Hemorrhagic fever or Marburg disease is an acute infectious pathology caused by the Marburg virus. It enters the body through damaged skin and mucous membranes of the eyes and mouth.
The symptoms of the disease depend on the stage of the pathological process. The incubation period lasts from 2 to 16 days. The disease has an acute onset and is characterized by an increase in body temperature to high levels. Along with fever, chills may appear. Signs of intoxication increase, such as weakness, headache, pain in muscles and joints, intoxication and dehydration. 2-3 days after this, gastrointestinal dysfunction and hemorrhagic syndrome appear.
All symptoms intensify by the end of the first week. Bleeding from the nose, gastrointestinal tract, and genital tract may also be observed. By the beginning of week 2, all signs of intoxication reach their maximum. In this case, convulsions and loss of consciousness are possible. According to the blood test, specific changes occur: thrombocytopenia, poikilocytosis, anisocytosis, granularity of erythrocytes.
If a person is suspected of having Marburg disease, he is urgently hospitalized in the infectious diseases department and must be kept in an isolated box. The recovery period may take up to 21-28 days.
Devic's disease
Neuromyelitis optica or Devic's disease has a chronic pattern similar to multiple sclerosis. This is an autoimmune disease, the causes of which are still unclear. One of the reasons for its development is an increase in the permeability of the barrier between the meninges and the vessel.
Some autoimmune diseases can trigger the progression of Devic's disease:
- rheumatoid arthritis;
- systemic lupus erythematosus;
- Sjögren's syndrome;
- dermatomyositis;
- thrombocytopenic purpura.
The disease has specific symptoms. Clinical manifestations are caused by disruption of conductive impulses. In addition, the optic nerve and spinal cord tissue are affected. In most cases, the disease manifests itself as visual impairment:
- a veil before the eyes;
- pain in the eye sockets;
- blurred vision.
As the disease progresses and there is no adequate treatment, the patient runs the risk of completely losing his vision. In some cases, regression of symptoms with partial restoration of eye function is possible. Sometimes it happens that myelitis precedes neuritis.
Neuromyelitis optica has two course options: a progressive increase in symptoms with simultaneous damage to the central nervous system. In rare cases, a monophasic course of the disease occurs. It is characterized by steady progress and worsening symptoms. In this case, the risk of death is increased. With the right treatment, the pathological process slows down, but complete recovery is not guaranteed.
The second option, the most common, is characterized by an alternating change of remission and exacerbation and is designated by the concept of “recurrent course.” It is also accompanied by visual disturbances and spinal cord dysfunction. During the period of remission, a person feels healthy.
To identify Devic's disease, a set of measures is carried out. In addition to standard diagnostic procedures, lumbar puncture with cerebrospinal fluid analysis, ophthalmoscopy and MRI of the spine and brain are performed.
Progressive multifocal leukoencephalopathy
People with immune deficiency may experience progressive multifocal multifocal leukoencephalopathy. This is an infectious disease caused by the penetration of the JC virus, which belongs to the Polyomavirus family, into the body. A feature of the pathology is that asymmetric and multifocal brain damage occurs. The virus affects the membranes of nerve endings, which are made of myelin. Therefore, this disease belongs to the group of demyelinating pathologies.
Almost 85% of patients with this diagnosis are AIDS or HIV infected. The risk group includes patients with malignant tumors.
Main symptoms of the disease:
- mood swings;
- visual disturbances;
- paresthesia and paralysis;
- memory impairment.
Guillain-Barre syndrome
An acute inflammatory disease characterized by “demyelinating polyradiculoneuropathy.” It is based on autoimmune processes. The disease manifests itself as sensory disturbances, muscle weakness and pain. It is characterized by hypotension and disorder of tendon reflexes. Respiratory failure may also occur.
All patients with this diagnosis should be admitted to the intensive care unit. Since there is a risk of developing respiratory failure and a ventilator may be required, the department must have intensive care.
Dependence of the clinic on the affected vessel
Ischemic signs differ according to the affected branches of the cerebral arteries.
Blockage of the anterior cerebral artery manifests itself:
- paresis of the arm and leg on the opposite side (symptoms predominate in the foot and hand);
- increased tone of the flexor muscles;
- speech disorders are possible;
- the patient is lethargic, consciousness is confused, less often - talkative and excited.
With impaired blood flow in the middle cerebral artery, symptoms are divided into lesions:
- deep branches feeding the subcortical centers;
- long arterial branches supplying the cerebral cortex.
Therefore, the signs appear differently:
- loss of movement and sensitivity of half the body;
- paresis of gaze;
- if the hearth is on the left - the inability to speak, write, the disappearance of practical skills.
A blockage in the posterior artery is different:
- severe headaches;
- loss of sensation and motor function;
- a sharp decrease in memory;
- visual disturbances.
Prevention
No drugs or methods of specific prevention of neuronal death have been developed. To maintain the activity of neuro-processes and brain vessels, we can only recommend:
- Lead a healthy lifestyle.
- Monitor your body weight.
- Maintain age-appropriate physical activity.
- Constantly monitor blood pressure, cholesterol , and blood sugar levels.
- Minimize bad habits.
- Practice a healthy balanced diet by minimizing foods containing animal fats.
- Train brain functions: solve puzzles/crosswords, learn poetry, foreign languages.
Mental changes of vascular nature
Often patients with vascular disorders of the brain present complaints of a special nature, indicating changes in the psyche. Preserved criticality is replaced by its loss, then the change in the character of the sick person can be judged by the reviews of employees at work and relatives.
The most typical:
- sleep disturbances (short-term, superficial);
- constant fatigue;
- intolerance to bright light, loud sounds, smells;
- increased irritability;
- memory loss;
- anxiety, suspiciousness.
In case of head injury, an X-ray examination of the skull is required.