Home / Neurologist / Cerebrovascular diseases
Diseases of the cerebral vessels , unfortunately, are now not at all uncommon. In Russian practice, vascular diseases of the brain are called discirculatory encephalopathy, and in foreign practice - ischemic brain disease. All these names describe the same condition.
Discirculatory encephalopathy (DE) is a condition manifested by a progressive multifocal disorder of brain function caused by cerebral circulatory insufficiency. The progression of neurological and mental disorders can be caused by persistent and long-term cerebral circulatory failure. Of no small importance in this regard is the aging process of the nervous, respiratory, and cardiovascular systems, which also leads to the development or intensification of hypoxia (oxygen starvation) of the brain. Brain hypoxia itself leads to further damage to the mechanisms regulating cerebral circulation. This fully applies to DE - a consequence of chronic vascular insufficiency of the brain, causing changes in brain tissue and disruption of its functioning.
According to statistics, up to 85% of the population are predisposed to developing various diseases related to the blood supply to the brain. This frightening number is due to the lifestyle of modern man. Many people know the word “hypertension” and “VSD” from adolescence, only if at school the diagnosis of “heart disease” was a reason not to go to physical education, then in adulthood a person receives real manifestations and evidence of the diagnosis.
About 30% of the population has a hereditary predisposition to stroke. 25% of stroke survivors die almost immediately (usually elderly people), another 25% die within six months; the risk of recurrent stroke over the next 1-2 years is 60%.
Symptoms of cerebrovascular disease
Cerebrovascular accident in the initial stages has very “harmless” manifestations, which most people attribute to fatigue, depression, weather, environmental conditions, etc. However, even mild malaise, dizziness and migraine attacks are already a reason to worry. Here are just some of the complaints that patients with impaired blood supply to the brain come with:
- Headaches, migraines.
- Dizziness, fainting.
- Hypertension or hypotension.
- Sleep disorders.
- Loss of coordination and balance.
- General weakness, malaise.
- Numbness of the limbs, loss of sensation.
- Memory impairment, especially for recent events, learning difficulties.
- Decreased intelligence, impoverished areas of interest, difficulty planning activities.
- Mood instability, emotional disturbances, possible depression, difficulty maintaining attention.
Cerebrovascular insufficiency: clinical picture, diagnosis and therapy
Stroke and chronic forms of cerebrovascular insufficiency represent one of the most pressing problems of modern neurology. According to epidemiological data, the incidence of stroke in the world is 150 cases per 100 thousand population per year. Chronic insufficiency of blood supply to the brain is also very widespread.
In the domestic literature, the term “dyscirculatory encephalopathy” (DE) is usually used to denote the clinical syndrome of brain damage resulting from insufficient blood supply to the brain. According to the classification of vascular diseases of the brain proposed by E.V. Schmidt (1985), dyscirculatory encephalopathy refers to chronic disorders of cerebral circulation.
Vascular diseases of the brain (E.V. Schmidt et al., 1985)
- Acute cerebrovascular accidents
*Stroke– Ischemic stroke (thrombotic, embolic, hemodynamic, lacunar)
– Hemorrhagic stroke (parenchymal hemorrhage, subarachnoid hemorrhage)
*Transient cerebrovascular accidents
– Transient ischemic attacks
– Hypertensive cerebral crises
- Chronic cerebrovascular accidents
*Initial manifestations of insufficient blood supply to the brain*Encephalopathy
However, as modern research shows, various cardiovascular diseases, as a rule, lead simultaneously to chronic cerebral ischemia and repeated acute cerebrovascular accidents. Therefore, it would be more correct to define discirculatory encephalopathy as a syndrome of chronic progressive brain damage, which is based on repeated strokes and/or chronic insufficiency of blood supply to the brain (N. N. Yakhno, I. V. Damulin, 2001).
Etiology and pathogenesis of DE
The most common causes of impaired blood supply to the brain are atherosclerosis of the main arteries of the head, heart disease with a high risk of thromboembolism in the brain, and hypertension. Less commonly, cerebrovascular accidents develop as a result of inflammatory changes in blood vessels (vasculitis), disorders of the blood coagulation system, abnormalities in vascular development, etc. In the vast majority of cases, cerebral vascular insufficiency develops in elderly people suffering from the above cardiovascular diseases.
As follows from the definition of DE, 2 main pathogenetic mechanisms play a role in the formation of this syndrome: stroke and chronic cerebral ischemia. Ischemic strokes of the brain develop as a result of thrombosis of cerebral arteries, thromboembolism in the brain, arteriolosclerosis, rheological and hemodynamic disorders.
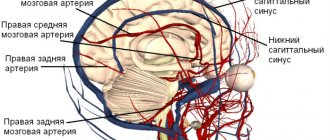
Chronic cerebral ischemia is based on structural changes in the vascular wall, which arise as a consequence of prolonged arterial hypertension or an atherosclerotic process. It has been established that lipohyalinosis of small-caliber vessels penetrating the brain substance can lead to chronic ischemia of the deep white matter. A reflection of this process are changes in the white matter (leukoaraiosis), which are defined as focal or diffuse changes in signal intensity from deep cerebral structures on T2-weighted images of magnetic resonance imaging of the brain. These abnormalities are considered to be typical neuroimaging symptoms that develop in patients with long-term uncontrolled arterial hypertension.
Clinical manifestations of DE
The clinical picture of DE is highly variable. As mentioned above, most patients with chronic vascular diseases of the brain have a history of strokes, often repeated. The localization of strokes undoubtedly largely determines the characteristics of the clinic. However, in the overwhelming majority of cases with cerebrovascular pathology, along with the consequences of strokes, there are also neurological, emotional and cognitive symptoms of dysfunction of the frontal lobes of the brain. This symptomatology develops as a result of disruption of connections between the frontal cortex and the subcortical basal ganglia (the “disconnection” phenomenon). The reason for the “disconnection” lies in diffuse changes in the white matter of the brain, which, as mentioned above, are a consequence of the pathology of small-caliber cerebral vessels.
Depending on the severity of the disorders, it is customary to distinguish 3 stages of dyscirculatory encephalopathy. The first stage is characterized mainly by subjective neurological symptoms. Patients complain of headache, dizziness, heaviness or noise in the head, sleep disorders, increased fatigue during physical and mental stress. These symptoms are based on a mild to moderate decrease in mood associated with dysfunction of the frontal lobes of the brain. Objectively, mild impairments of memory and attention, as well as possibly other cognitive functions, are detected. There may be an asymmetrical increase in tendon reflexes, uncertainty when performing coordination tests, and slight changes in gait. Instrumental research methods that make it possible to detect the pathology of cerebral vessels are important in the diagnosis of cerebral vascular insufficiency at this stage of the pathological process.
The second stage of discirculatory encephalopathy is spoken of in cases where neurological or mental disorders form a clinically defined syndrome. For example, we may be talking about mild cognitive impairment syndrome. This diagnosis is legitimate in cases where impairments in memory and other cognitive functions clearly go beyond the age norm, but do not reach the severity of dementia. At the second stage of DE, neurological disorders such as pseudobulbar syndrome, central tetraparesis, usually asymmetrical, extrapyramidal disorders in the form of hypokinesia, mild or moderate increase in muscle tone of the plastic type, ataxic syndrome, neurological disorders of urination, etc. can also develop.
At the third stage of dyscirculatory encephalopathy, a combination of several of the above neurological syndromes is noted and, as a rule, vascular dementia is present. Vascular dementia is one of the most severe complications that develops with the unfavorable course of cerebrovascular insufficiency. According to statistics, vascular etiology underlies at least 10–15% of dementia in old age.
Vascular dementia, like DE in general, is a pathogenetically heterogeneous condition. Vascular dementia is possible after a single stroke in a strategic area of the brain for cognitive activity. For example, dementia can develop acutely as a result of a heart attack or hemorrhage in the thalamus. However, much more often vascular dementia is caused by repeated strokes (so-called multi-infarct dementia). Another pathogenetic mechanism of vascular dementia is chronic cerebral ischemia, reflected by changes in the white matter of the brain. Finally, in addition to cerebral ischemia and hypoxia, secondary neurodegenerative changes play an important role in the pathogenesis of dementia in cerebrovascular insufficiency, at least in some patients with DE. Modern research has convincingly proven that insufficient blood supply to the brain is a significant risk factor for the development of degenerative diseases of the central nervous system, in particular Alzheimer's disease. The addition of secondary neurodegenerative changes undoubtedly aggravates and modifies cognitive disorders in cerebrovascular insufficiency. In such cases, the diagnosis of mixed (vascular-degenerative) dementia is legitimate.
Clinical manifestations of vascular dementia in each specific case depend on the pathogenetic mechanisms determining the disease. In post-stroke and multi-infarction dementia, clinical features depend on the location of the strokes. Changes in the white matter of the deep lobes of the brain as a result of chronic ischemia lead to cognitive impairment of the “frontal” type. These disorders are characterized by emotional disorders in the form of decreased mood, depression or apathy, and loss of interest in the environment. Emotional lability, which is a rapid, sometimes causeless change of mood, tearfulness or increased irritability, is also very characteristic. In the cognitive sphere, memory and attention impairments, slowness of thinking, decreased intellectual flexibility, and difficulties associated with switching from one type of activity to another are determined. The behavior of patients changes: the ability for self-criticism and the sense of distance are reduced, increased impulsiveness and distractibility are noted, symptoms such as disregard for socially accepted rules of behavior, asociality, foolishness, flat and inappropriate humor, etc. may be present.
The presence of secondary neurodegenerative changes in vascular dementia is manifested primarily by progressive memory impairment. At the same time, to a greater extent, the patient forgets what happened recently, while memories of distant events are retained for quite a long time. The neurodegenerative process is also characterized by disturbances in spatial orientation and speech.
Diagnosis of dyscirculatory encephalopathy
To diagnose dyscirculatory encephalopathy syndrome, it is necessary to carefully study the medical history, assess the neurological status, and use neuropsychological and instrumental research methods. It is important to emphasize that the presence of cardiovascular diseases in an elderly person does not in itself serve as evidence of the presence of cerebral vascular insufficiency. A necessary condition for correct diagnosis is to obtain convincing evidence of a cause-and-effect relationship between neurological and cognitive symptoms and cerebrovascular pathology, which is reflected in the currently accepted diagnostic criteria for DE.
Diagnostic criteria for DE (N. N. Yakhno, I. V. Damulin, 2001)
- Presence of signs (clinical, anamnestic, instrumental) of brain damage.
- Presence of signs of acute or chronic cerebral dyscirculation (clinical, anamnestic, instrumental).
- The presence of a cause-and-effect relationship between hemodynamic disorders and the development of clinical, neuropsychological, and psychiatric symptoms.
- Clinical and paraclinical signs of progression of cerebrovascular insufficiency.
Evidence of a vascular etiology for symptoms would include the presence of focal neurological symptoms, a history of stroke, characteristic neuroimaging changes such as post-ischemic cysts or marked white matter changes.
Treatment of cerebrovascular insufficiency
Cerebrovascular insufficiency is a complication of various cardiovascular diseases. Therefore, etiotropic therapy for DE should be, first of all, aimed at the underlying pathological processes of cerebrovascular insufficiency, such as arterial hypertension, atherosclerosis of the main arteries of the head, heart disease, etc.
Antihypertensive therapy is an essential factor in the secondary prevention of the increase in mental and motor symptoms of cerebrovascular insufficiency. To date, however, the question of what blood pressure levels should be achieved in the treatment of hypertension has not been resolved. Most neurologists believe that complete normalization of blood pressure in elderly patients with a long history of hypertension, while reducing the risk of acute vascular episodes, can simultaneously contribute to the aggravation of chronic cerebral ischemia and an increase in the severity of cognitive dysfunction of the “frontal” type.
The presence of hemodynamically significant atherosclerosis of the main arteries of the head requires the prescription of antiplatelet agents. Drugs with proven antiplatelet activity include acetylsalicylic acid at doses of 75-300 mg per day and clopidogrel (Plavix) at a dose of 75 mg per day. The study showed that the use of these drugs reduces the risk of ischemic events (myocardial infarction, ischemic stroke, peripheral thrombosis) by 20-25%. The possibility of simultaneous use of these drugs has now been proven. Medicines with antiplatelet properties also include dipyridamole (chimes), which is used in doses of 25 mg three times a day. Monotherapy with this drug does not provide prevention of cerebral or other ischemia, however, with combined use, dipyridamole significantly increases the preventive effect of acetylsalicylic acid. In addition to the prescription of antiplatelet agents, the presence of atherosclerotic stenosis of the main arteries of the head requires referral of the patient for consultation with a vascular surgeon to decide on the advisability of surgical intervention.
If there is a high risk of thromboembolism in the brain, for example in cases of atrial fibrillation and valvular disease, antiplatelet agents may be ineffective. The listed conditions serve as an indication for the prescription of indirect anticoagulants. The drug of choice is warfarin. Therapy with indirect anticoagulants should be carried out under strict monitoring of coagulogram parameters.
The presence of hyperlipidemia that cannot be corrected by diet requires the prescription of lipid-lowering drugs. The most promising drugs are from the statin group (Zocor, Simvor, Simgal, Rovacor, Medostatin, Mevacor, etc.). According to some data, therapy with these drugs not only normalizes lipid metabolism, but also may have a preventive effect against the development of a secondary neurodegenerative process against the background of cerebrovascular insufficiency.
An important pathogenetic event is also the impact on other known risk factors for cerebral ischemia. These include smoking, diabetes, obesity, physical inactivity, etc.
In the presence of cerebrovascular insufficiency, the prescription of drugs that act primarily on the microvasculature is pathogenetically justified. These include:
- phosphodiesterase inhibitors: aminophylline, pentoxifylline, vinpocetine, tanakan, etc. The vasodilating effect of these drugs is associated with an increase in the cAMP content in the smooth muscle cells of the vascular wall, which leads to their relaxation and an increase in the lumen of blood vessels;
- calcium channel blockers: cinnarizine, flunarizine, nimodipine. They have a vasodilating effect due to a decrease in the intracellular calcium content in the smooth muscle cells of the vascular wall. Clinical experience suggests that calcium channel blockers, such as cinnarizine and flunarizine, may be more effective for vertebrobasilar circulatory failure; this is manifested by symptoms such as dizziness and unsteadiness when walking;
- α2-adrenergic receptor blockers: nicergoline. This drug eliminates the vasoconstrictor effect of the mediators of the sympathetic nervous system: adrenaline and norepinephrine.
Vasoactive drugs are among the most commonly prescribed drugs in neurological practice. In addition to the vasodilatory effect, many of them also have positive metabolic effects, which allows these drugs to be used as symptomatic nootropic therapy. Experimental data indicate that the vasoactive drug tanakan has the ability to deactivate free radicals, thereby reducing the processes of lipid peroxidation. The antioxidant properties of this drug also allow it to be used for secondary prevention of the increase in memory impairment and other cognitive functions in cases of secondary neurodegenerative changes.
In domestic practice, vasoactive drugs are usually prescribed in courses of 2-3 months, 1-2 times a year.
Metabolic therapy is widely used for cerebrovascular insufficiency, the purpose of which is to stimulate the reparative processes of the brain associated with neuronal plasticity. In addition, metabolic drugs have a symptomatic nootropic effect.
Piracetam was the first drug specifically synthesized to affect memory and other higher brain functions. In recent years, however, it has been possible to prove that in previously taken doses this drug has a relatively small clinical effect. Therefore, the use of piracetam in dosages of at least 4–12 g/day is currently recommended. Intravenous administration of this drug in saline solution is more appropriate: 20–60 ml of piracetam per 200 ml of saline solution intravenously, 10–20 infusions per course.
The peptidergic drug Cerebrolysin is no less successfully used for cerebrovascular insufficiency, as well as vascular and degenerative dementia. As in the case of piracetam, views on the dosage regimen of this drug have changed significantly in recent years. According to modern concepts, the clinical effect occurs in the case of intravenous administration of Cerebrolysin in doses of 30–60 ml intravenously in 200 ml of saline, 10–20 infusions per course.
Peptidergic drugs that have a beneficial effect on cerebral metabolism also include Actovegin. Actovegin is used in the form of intravenous infusions (250–500 ml per infusion, 10–20 infusions per course), or in the form of intravenous or intramuscular injections of 2–5 ml 10–20 injections, or orally 200–400 mg 3 times a day within 2-3 months.
Like vasoactive drugs, metabolic therapy is carried out in courses 1-2 times a year. Pathogenetically justified and appropriate is the combined implementation of vasoactive and metabolic therapy. Currently, the doctor has several combined dosage forms at his disposal, which include active substances with vasoactive and metabolic effects. These drugs include instenon, vinpotropil, fezam and some others.
The development of vascular dementia syndrome requires more intensive nootropic therapy. Among modern nootropic drugs, acetylcholinesterase inhibitors have the most powerful clinical effect on cognitive functions. Initially, drugs in this group were used in the treatment of mild and moderate dementia due to Alzheimer's disease. Today it has been proven that acetylcholinergic deficiency plays an important pathogenetic role not only in this disease, but also in vascular and mixed dementia. Therefore, cognitive disorders of vascular and mixed etiology are increasingly appearing among the indications for the prescription of acetylcholinesterase inhibitors.
In Russia, two drugs from the group of latest generation acetylcholinesterase inhibitors are currently available: Exelon and Reminyl. Exelon is prescribed at an initial dose of 1.5 mg 2 times a day, then the single dose is increased by 1.5 mg every 2 weeks. up to 6.0 mg 2 times daily or until side effects occur. Common side effects when using Exelon are nausea and vomiting. These phenomena do not pose a threat to the life or health of the patient, but may interfere with the achievement of a therapeutic effect. Reminyl is prescribed at 4 mg 2 times a day for the first 4 weeks, and then 8 mg 2 times a day. This drug is less likely to cause adverse events.
First generation acetylcholinesterase inhibitors include neuromidin. According to some data, this drug has a positive nootropic effect in both vascular and primary degenerative and mixed dementia. It is prescribed in a dose of 20–40 mg 2 times a day.
Therapy with acetylcholinesterase inhibitors should be carried out continuously. In this case, it is necessary to monitor the level of liver enzymes in the blood once every 3–6 months.
The use of akatinol memantine is also pathogenetically justified for vascular dementia. This drug is an inhibitor of NMDA glutamate receptors. Chronic intake of akatinol memantine has a symptomatic nootropic effect, and may also slow down the rate of increase in cognitive disorders. The effect of the drug was manifested in both mild and moderate and severe dementia. It should be noted that akatinol memantine is the only drug effective at the stage of severe dementia. It is prescribed during the first week 5 mg 1 time per day, during the second week - 5 mg 2 times a day, starting from the third week and then continuously - 10 mg 2 times a day.
In conclusion, it should be emphasized that a comprehensive assessment of the state of the cardiovascular system of patients with cerebrovascular insufficiency, as well as the impact on both the cause of the disorders and the main symptoms of DE, undoubtedly contribute to improving the quality of life of patients and preventing severe complications of cerebrovascular insufficiency, such as , such as vascular dementia and movement disorders.
V.V. Zakharov, Doctor of Medical Sciences Clinic of Nervous Diseases named after. A. Ya. Kozhevnikova, Moscow
General information about cerebral ischemia
A disease in which blood circulation to the brain is reduced or completely stopped is called ischemia. The cause of the disorder is a pathological narrowing of the lumen of blood vessels, in which oxygen does not flow in the required volume. Lack of nutrition leads to malfunctions, which are expressed by general malaise and other symptoms.
Medicine has identified two forms of the disease:
- Focal
- in which tissue damage is localized in only one area. The cause is an embolism or blood clot that blocks the blood flow. - Global
- characterized by a decrease or cessation of blood circulation in several areas of the brain.
As a result of oxygen starvation of tissues, ischemia develops. With early diagnosis, complications of the disease can be avoided.
Forecast and prevention of cerebral ischemia
When the first symptoms occur, the patient should visit a neurologist. Timely treatment will help prevent complications and an undesirable prognosis for the patient. Ischemia of the blood vessels of the head against the background of high blood pressure progresses quickly, so the patient’s concern for his health should begin with an examination by a doctor.
Prevention of vascular exacerbations includes following a diet, quitting smoking, alcohol, weight control, and avoiding stress. In case of aggravating factors (diabetes, hypertension), observation by a specialist should be systematic. Doctors do not recommend long periods of physical activity or frequent sun exposure for elderly patients.
Causes and development of atherosclerosis
The main reason for the clinical manifestations of obliterating atherosclerosis is a person’s ability to live more than 40 years. Early mortality in previous centuries did not allow diagnosing arterial damage. Most diseases that lead to death or disability are in one way or another associated with atherosclerosis. Age-related atherosclerosis appears in all people sooner or later. However, a number of patients exhibit an innate tendency to atherosclerosis - hyperlipedemia (hereditary increase in cholesterol in the blood).
The main changes in atherosclerosis develop in the intima (inner lining) of the arteries. Cholesterol and fatty inclusions (lipids) begin to be deposited here, forming yellowish spots on the inner wall of the vessel. Subsequently, the formation of an atherosclerotic plaque occurs. Platelets and clots of fibrin and calcium salts settle on the plaques.
With an abundant accumulation of lipids and calcium, blood circulation in the plaques is impaired, the necrosis of which causes the appearance of atheroma cavities filled with disintegrating masses. The artery wall in the area of such a plaque is rock hard and crumbles easily. Crumb-like masses are rejected into the lumen of the vessel. Getting through the bloodstream into the underlying blood vessels, pieces of crumbled atherosclerotic plaque can cause blockage (embolism) and lead to thrombosis of the arteries of the limb with the development of gangrene (death). In addition, a large plaque leads to a significant disruption of blood flow, which reduces the delivery of oxygen to the tissues. During physical activity, muscles that do not receive sufficient nutrition refuse to work, pain occurs, which disappears only after rest. A large plaque promotes the development of a blood clot at the site of narrowing of the vessel, which can lead to acute ischemia and gangrene.
Drug therapy can be aimed at the causes of the disease (etiotropic treatment), the mechanisms of its development (pathogenetic treatment), the symptoms of the disease (symptomatic therapy) and the prevention of complications. The treatment of vascular patients should use a regimen that addresses all aspects of the disease.
Etiotropic and pathogenetic treatment.
Obliterating atherosclerosis . Treatment is aimed at preventing the development of atherosclerotic plaques. In addition to diet, drugs that reduce high cholesterol levels - statins - are used. Their list is quite extensive. In our practice, we use lovastatin, pravastatin, simvastatin, fluvastatin, atorvastatin, rosuvastatin. Statins have vascular effects. At the level of the vascular wall, by reducing the formation of cholesterol and low-density lipoproteins, they reduce the inclusion of cholesterol in the vascular subintima, help stabilize existing atherosclerotic plaques by reducing the lipid core, and therefore reduce the risk of plaque rupture and thrombus formation. Improvement in the functional state of the vascular endothelium during statin therapy is associated not only with their main effect, but also with pleiotropic effects. Taking statins should be long-term.
Diabetic macroangiopathy. In addition to statin therapy, the drug Vessel Due F, an organic glypolysaccharide, which helps restore the endothelium and reduces the risk of vascular thrombosis, is used to improve the condition of the vascular wall. To treat neuropathy in patients with diabetes, B vitamins (milgamma) and thioctacid are used.
Thromboangiitis obliterans (Buerger's disease) is an inflammatory disease of the arteries. For pathogenetic treatment, anti-inflammatory drugs are used - adrenal hormones in shock doses (pulse therapy). Most often, methylprednisolone (solu-medrol) is used for a short course. Targeted pulse therapy can improve the prognosis for patients with obliterating endarteritis.
Drugs that improve blood flow and affect collateral circulation.
Prostaglandins (vazaprostan, alprostan, ilomedine).
These drugs have a vasodilating effect on small arterioles, which increases the volume of blood flowing through the tissue. Sometimes this effect allows you to stop critical ischemia and delay the development of gangrene. However, without restoring the main blood flow, these drugs rarely help save a limb when gangrene develops. The drugs are antispasmodics. Modern data on such antispasmodics as papaverine, noshpa, nicotinic acid indicate their ineffectiveness and even harmfulness for patients with obliterating diseases. By dilating large unaffected arteries, they cause steal in small vessels and aggravate arterial insufficiency, and therefore should be excluded from the arsenal of vascular surgeons.
Pentoxifylline (trental, vasonite) is still widely used in domestic clinical practice, although many studies have shown their low effectiveness.
Cilastozol (Pletal) is a drug with a proven effect in intermittent claudication. However, it is not registered in the Russian Federation.
Actovegin and solcoseryl are drugs popular in domestic practice (deproteinized extracts from cattle plasma) contain a set of vitamins and minerals, some plasma hormones. Unfortunately, their effect does not meet expectations. In our practice, these drugs are not used.
Neovasculgen is a new genetic drug that stimulates the production of endothelial growth factor in tissues. According to the creators, it should stimulate the development of collateral circulation. Our limited experience does not confirm the effectiveness of the drug in patients with critical ischemia due to Buerger's disease. The high cost of the drug does not allow large-scale research into this issue.
Symptomatic therapy.
Implies a reduction in the symptoms of vascular diseases. Effective pathogenetic treatment helps eliminate the symptoms of chronic arterial insufficiency. In critical ischemia, pain relief is an important aspect of treatment. For these purposes, non-narcotic analgesics (ketorol, baralgin, diclofenac) are used. For neuralgic pain, Finlepsin and other sedatives are prescribed. In difficult cases, it is possible to prescribe narcotic analgesics (tramadol, promedol, morphine) or prolonged epidural anesthesia.
Prevention of complications.
The main complication associated with obliterating diseases is arterial thrombosis with the development of acute limb ischemia. Currently, the possibilities of modern therapy make it possible to significantly reduce the risk of thrombosis. The most effective drugs are clopidogrel (Plavix, Zilt, Thrombostop). Aspirin preparations (thromboass, cardiomagnyl) can be used in a dose of at least 100 mg per day, but they are weaker. In patients with a tendency to venous thrombosis and atrial fibrillation, indirect anticoagulants (warfarin), direct thrombin inhibitors (Prodaxa), low molecular weight heparins (Fraxiparine, Clexane) can be used to prevent thromboembolism.
High levels of cholesterol in the blood lead to the risk of developing atherosclerotic plaques. Due to blockage of blood vessels by atherosclerotic plaques, myocardial infarction, ischemic stroke or gangrene of the extremities develops.
Dementia
With significant severity of the above symptoms, vascular dementia develops with its characteristic slowdown and stiffness of all mental processes (torpidity and rigidity), mood variability (emotional lability), and a significant narrowing of the sphere of interests.
Patients with vascular lesions of the brain often become helpless in their mental state and cannot care for themselves. Moreover, during periods of confusion, they tend to leave home and may not find their way back. Thus, there is a danger to the patient’s life due to his mental illness. There are delusional variants of the course of dementia, which, combined with a pronounced decrease in criticism of one’s own behavior, can create a danger to the lives of others.
The treatment of mental disorders in vascular diseases of the brain is carried out by a psychiatrist. In connection with the development of new drugs, significant correction of the psychopathological picture is now possible.
All materials on the site are presented for informational purposes only, approved by certified physician Mikhail Vasiliev, diploma series 064834, in accordance with license No. LO-77-005297 dated September 17, 2012, by a certified specialist in the field of psychiatry, certificate number 0177241425770.
Classification of cerebral ischemia
The deterioration of vascular activity occurs with varying degrees of severity, therefore two types of the disease are distinguished:
- Acute
, characterized by the suddenness of the onset of symptoms and the minimum period of development of the disease (stroke, cerebral infarction). - Chronic
, occurs as a result of the slow development of brain dysfunction due to diffuse (extensive) or small focal damage to brain tissue in conditions of prolonged insufficiency of cerebral blood supply. In this condition, patients develop symptoms gradually, with further progression.
Vascular pathology occurs not only in adults, but even in newborns due to a lack of oxygen during the mother’s pregnancy.
Risk factors
Brain diseases can be caused by various reasons related to lifestyle, as well as existing health problems.
- Smoking. Nicotine and other substances contained in tobacco smoke provoke atherosclerosis and vascular aneurysm at a high rate.
- Low physical activity. Physical education improves the plasticity of the brain - its ability to create new connections and transform itself. Accordingly, if a person does not perform even minimal exercise, his brain does not create new neural connections and quickly destroys old ones.
- Male gender. According to research, men are more likely to suffer from brain diseases because they lead an unhealthy lifestyle.
- High blood pressure. As a result of surges in blood pressure, protrusion of the vessel wall in a weak spot may occur.
- Poor nutrition and obesity. If a woman’s waist exceeds 88 cm, and a man’s waist exceeds 102, it is necessary to adjust your diet. With obesity, insulin insensitivity develops (cells lose sensitivity to the hormone, and the pancreas produces more of it than normal).
- Alcohol. The alcohol contained in alcoholic drinks is absorbed into the blood, enters the brain and destroys its cortex.
- High cholesterol. It affects blood vessels, forming cholesterol plaques on their walls, interfering with normal blood flow.
- Stress. Recent studies have shown that stress impairs brain function due to the production of cortisol (the stress hormone).
- Age. Many diseases begin to appear younger and appear at an earlier age than decades ago. For example, cholesterol plaques begin to form in the blood vessels of the brain by the age of 35, which can lead to atherosclerosis.
- Genetics. If your close relatives have developed brain diseases under 50 years of age, then you are at high risk.
- Infections and inflammations. They affect the brain matter, disrupting the functioning of the immune system and brain.
Diagnosis of cerebral ischemia
To identify a dangerous disease, neurologists use an integrated approach to diagnosis. During the examination, the doctor collects anamnesis and conducts a primary examination, for example, a finger-nose test. To do this, the patient is asked to stand up, align his legs shoulder-width apart, spread his arms to the sides, bending them at an angle of 90 degrees, and close his eyes. Next, the patient should touch the tip of the nose with the index finger. With developing ischemia, contact between the two surfaces will not occur, and the missed finger will certainly point in the direction of the damaged lobe.
In addition to the finger-nose test, the doctor will examine other abilities of the patient, such as facial expressions, pupil reaction, facial symmetry, clarity of speech and coordination. Along with the examination, the necessary tests are additionally collected:
- Blood pressure is measured in a doctor's office.
- Detection of vascular lesions of the fundus is carried out by an ophthalmologist.
- Undergoing electrocardiography for correct diagnosis.
- Dopplerography of blood vessels is mandatory.
- Electroencephalography reveals inactive areas of the brain.
- CT (computed tomography), MRI (magnetic resonance imaging) perform an in-depth examination.
- A biochemical blood test evaluates cholesterol levels.
Doctors use differential diagnostic methods, since the symptoms of the pathology are similar to the manifestations of other diseases of an infectious, allergic, neurological and oncological nature.
Diagnostics
Accurate and objective diagnostic information plays an important role in choosing a treatment method, especially surgical, the place and time of its implementation. The therapeutic and diagnostic capabilities of modern neurosurgery are increasing rapidly thanks to new diagnostic equipment. At the same time, traditional diagnostic methods also remain relevant.
Diagnostic lumbar puncture is an informative method for determining subarachnoid hemorrhage, which often occurs when an intracranial aneurysm ruptures. Using echoencephalography (EchoEG), when an aneurysm ruptures with the formation of a hematoma, the side of its location is specified based on the pronounced (more than 4-6 mm) displacement of the M-echo.
Doppler ultrasound allows you to non-invasively determine the linear speed and direction of blood flow, the degree and level of circulatory disorders in the main arteries. Duplex (double) ultrasound scanning makes it possible to simultaneously determine changes in blood flow and obtain an image of the vessel itself, identify carotid artery stenosis (less than 50%), as well as the location and structure of the atherosclerotic plaque.
Changes in cerebral blood flow and cerebral vascular tone can be judged from the data of rheoencephalography, impedance rheoplethysmography and telethermography.
The study of regional cerebral blood flow using the clearance of a radioactive isotope (rXe) allows us to determine the degree of reduction in cerebral circulation. Computed tomography (CT) allows one to differentiate focal cerebral ischemia from hemorrhage. The size and location of the intracranial hematoma and the focus of cerebral infarction, as well as the state of the surrounding brain space, are clearly determined. Magnetic resonance imaging (MRI) makes it possible, even without the use of a contrast agent, to evaluate not only anatomical structures, but also the level of energy, enzymatic and metabolic processes in the brain. Non-invasive nuclear magnetic resonance angiography has even greater diagnostic capabilities, which allows you to obtain angiograms in any projection and identify not only aneurysms, but also atherosclerotic plaques in the arteries.
Recently, nuclear magnetic resonance spectroscopy has been used, which makes it possible to draw conclusions about the dynamics of focal brain lesions both in areas of irreversible changes and in the “ischemic penumbra” zone.
Treatment in each case is selected individually, depending on the cause and location of the damage.
Ischemic brain lesions
The main cause of ischemic stroke is a decrease in cerebral blood flow due to stenotic and occlusive lesions of the great vessels of the neck and arteries of the brain.
In the development of ischemic stroke (cerebral infarction), an important role is played by the blockage of cerebral vessels by microthrombi, which are formed as a result of atherosclerotic plaques breaking off and moving through the vessels.
The main etiological factors leading to damage to both extracranial and intracranial vessels include atherosclerosis, hypertension, and rheumatism. Much less often, the cause of obstruction of the patency of the carotid arteries is cicatricial traumatic and inflammatory extravascular lesions, fibromuscular dysplasia resulting from radiation therapy, as well as pathological bends of blood vessels.
The clinical picture of cerebral infarction depends on the location of the lesion, and the severity and persistence of symptoms depends on the size and condition of the collateral systems. Thrombosis of the internal carotid artery is characterized by decreased visual acuity or blindness on the affected side and hemiparesis or hemiplegia on the opposite side. With arterial stenosis, these disorders can be temporary,
CHEM diagnostics
Unfortunately, there are currently no generally accepted diagnostic criteria for chronic cerebrovascular disease. This is probably one of the main reasons for the apparent overdiagnosis of CCI in everyday clinical practice. However, due to the fact that the main clinical manifestation of CCI is cognitive impairment, diagnostic criteria for vascular cognitive impairment can be used.
To screen for vascular cognitive impairment, it is currently recommended to use the Montreal Cognitive Scale as it is the most sensitive for mild cognitive impairment of the subcortical type [30]. However, testing using this method takes 10–15 minutes, which is prohibitively long for a daily outpatient appointment. As an alternative, the Mini-Cog technique can be used, although its sensitivity in the early stages of chronic cerebrovascular disease is significantly lower [31].
To verify the vascular nature of cognitive impairment identified using scales, it is necessary to perform an MRI of the brain. Without MRI, the diagnosis is considered presumptive.