1.What is ACTH?
ACTH is a hormone that can be tested to test the condition of the pituitary and adrenal glands.
ACTH is produced by the pituitary gland.
The adrenal glands respond to ACTH levels in the blood and produce cortisol, which helps your body cope with stress. Cortisol is a vital hormone,
so its level in the blood should be monitored. When cortisol levels are elevated, ACTH levels fall and vice versa.
Cortisol and ACTH levels change throughout the day.
As a rule, the ACTH hormone is elevated in the morning (from 6 to 8 am) and decreases by 6 pm. If the doctor wants to check the ACTH level, then it is measured in the morning and evening. Cortisol levels are usually checked along with ACTH.
A must read! Help with treatment and hospitalization!
Corticotropin releasing hormone test
In rare cases, ACTH can be produced not only by the pituitary gland, but also by a malignant tumor in any organ. Tests show high levels of ACTH and cortisol. To diagnose the pathology, a test with corticotropin-releasing hormone is prescribed. After it, the ACTH level either increases (indicating Itsenko-Cushing's disease) or remains at the same level (ectopic production syndrome).
To carry out the test, venous blood is taken in the morning on an empty stomach and ACTH is measured. Then 100 mcg of corticotropin-releasing hormone is injected into a vein and blood is drawn after 30, 45 minutes and 1 hour, determining the ACTH level for each time.
3.How to prepare and how is the analysis carried out?
How to prepare for an ACTH test?
You should not eat, drink, stress, or exercise for 10 to 12 hours before your blood draw.
If the doctor wants to measure the peak level of corticotropin in the blood, then the tests will have to be taken in the morning; if the doctor wants to find out the lowest level, then in the evening.
How is ACTH analysis performed?
An ACTH test is performed after taking blood from a vein. Blood sampling from a vein is carried out according to a standard procedure.
About our clinic Chistye Prudy metro station Medintercom page!
Indications for analysis
A test for hormone levels is prescribed for the diagnosis and treatment of diseases associated with dysfunction of the adrenal cortex. Monitoring indicators is also necessary to assess the effectiveness of therapy for oncological pathologies.
In women, ACTH is performed in case of menstrual irregularities, excessive hair growth, and infertility.
What symptoms and activities may be a reason for getting tested:
- abnormal pigmentation of the epidermis;
- acne in adults;
- early puberty in adolescents;
- Cushing's disease (fat deposition on the face, neck, abdomen, purple stretch marks on the abdomen, thinning limbs, increased blood sugar, high blood pressure);
- diseases of the skeletal system (osteoporosis), as well as muscle weakness and pain;
- causeless weight loss accompanied by high blood pressure;
- regular attacks of hypertension;
- severe fatigue, weakness and lethargy for a long time;
- deviation from the norm of cortisol in the blood;
- monitoring the patient’s rehabilitation after removal of corticotropinoma (tumor in the pituitary gland);
- long-term treatment with medications (for example, glucocorticoids);
- dysfunction of the adrenal cortex;
- monitoring the effectiveness of treatment for cancer patients.
For a doctor, the reason for referring a patient to ACTH may be:
- test with corticotropin-releasing hormone;
- changes in cortisol levels;
- suspected ACTH-producing tumor.
4. Risks of analysis and what can interfere with the test?
Risks of ACTH testing
If you take a blood test for ACTH, then possible risks may only be associated with taking blood from a vein. In particular, the appearance of bruises at the site of blood sampling and inflammation of the vein (phlebitis). Warm compresses several times a day will relieve phlebitis. If you are taking blood thinning medications, you may bleed at the puncture site.
What can interfere with the test?
Reasons why you may not be able to take a corticotropin test include:
- Taking corticosteroid drugs, estrogens, spironolactone. Also, the test results can be affected by amphetamines and insulin, after taking which the level of cortisol is increased.
- Alcohol or drug intoxication.
- Pregnancy or menstruation in women.
- Physical or emotional stress.
ACTH – ectopic syndrome with hypercortisolism. Clinical case.
ACTH-ectopic syndrome is a severe multisymptomatic disease caused by the secretion of corticotropin-releasing hormone (CRH) and/or adrenocorticotropic hormone (ACTH) by an ectopic tumor (apudoma), an increase in the production of hormones by the adrenal cortex and the development of the clinical picture of hypercortisolism.
ACTH-producing tumors of various locations originate from a group of cells of the diffuse neuroendocrine system (DNES), or APUD system (from English APUD: amine precursor uptake and decarboxylation). Apudocytes are derivatives of neuroectoderm. The syndrome of ectopic hormone secretion was first defined by G. Liddle et al. In 1968, R. Gilleman was awarded the Nobel Prize for the development of the APUD theory. Varieties of ACTH-ectopic DNES tumors are carcinoids of various localizations and degrees of malignancy. Ectopic ACTH production occurs in 10% of all cases of Cushing's syndrome and in 25% of the ACTH-dependent variant of Cushing's syndrome. 60% of ACTH-ectopic tumors are tumors of the thoracic cavity, which include the following: 1) bronchopulmonary carcinoid, characterized by slow tumor growth and long life expectancy - 36-46% of all ACTH-ectopic tumors; 2) small cell lung cancer, characterized by rapid growth and early generalization of the process - 8-20%; 3) thymic carcinoid, associated in most cases with paraneoplastic syndromes - 8-10%. The prevalence of lung carcinoids is 0.7–4.8 per 100,000 population (2% of all primary lung tumors). The prevalence of a typical lung carcinoid is 7-25% of all carcinoids. The ACTH-producing variant of lung carcinoid accounts for 1-2% of all lung carcinoids. At the age of under 50 years, women predominate among patients with TC and AK of the lung; after 50 years, these carcinoids are equally common in men and women.
The clinical picture is characterized by severe hyperpigmentation of the skin and mucous membranes, progressive muscle weakness, especially pronounced in the lower extremities (it is often impossible to get up from a chair), obesity with fat deposition in the torso, face and neck, the appearance of stretch marks on the skin of a purplish-cyanotic color, increased blood pressure, clinical signs of osteoporosis appear. There is a tendency to inflammatory processes. Women develop amenorrhea, hirsutism, and hypertrichosis. In men, potency is impaired, gynecomastia develops, and the voice changes. Signs of diabetes mellitus appear.
Diagnosis of patients with ectopic ACTH syndrome consists of determining increased production of ACTH, cortisol and assessing the daily rhythm of cortisol secretion, topical diagnostics to identify the location of the tumor, differential diagnosis of hypercortisolism and additional examination methods to clarify the severity of the disease.
Plasma ACTH levels are an important indicator for diagnosing ectopic syndrome. Its level usually rises from 100 to 1000 pg/ml and above. Almost 1/3 of patients with ectopic ACTH secretion syndrome may have the same increase in the level of this hormone as in Itsenko-Cushing's disease.
In terms of diagnostics for the syndrome of ectopic ACTH production, an increase in the content of corticotropin above 200 pg/ml and the results of selective determination of the content of adrenocorticotropic hormone in various veins are important. An important role in the diagnosis of ectopic ACTH production syndrome is played by the ratio of the concentration of ACTH obtained by catheterization of the inferior temporal sinus to the simultaneously determined level of the hormone in the peripheral vein. This indicator for ectopic tumors is 1.5 and lower, while in Itsenko-Cushing's disease it ranges from 2.2 to 16.7. The authors believe that the use of the ACTH indicator obtained in the inferior temporal sinus is more reliable than in the jugular vein.
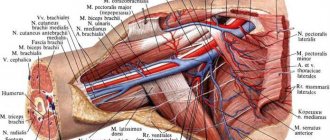
For a topical diagnosis of an ectopic tumor, retrograde catheterization of the inferior and superior vena cava and sampling of blood flowing from the right and left adrenal glands separately are used. Studies of the ACTH content in these samples make it possible to detect an ectopic tumor.
Topical diagnosis of ectopic tumors is difficult. In addition to the selective determination of ACTH, various X-ray methods and computed tomography are used for this purpose. The search should begin with examination of the chest as the most common site of ectopic tumors. To determine the main group of chest tumors (lungs and bronchi), tomographic examination of the lungs is used. Often the foci of oat cell cancer of this organ are very small, poorly diagnosed and late, often after removal of the adrenal glands, 3-4 years from the onset of the syndrome.
Treatment. The goal of treatment is to remove the tumor as a source of ACTH and normalize the function of the adrenal cortex. The choice of treatment method for ectopic ACTH production syndrome depends on the location of the tumor, the extent of the tumor process and the general condition of the patient. In cases of tumor inoperability, radiation therapy and chemotherapy are used.
All of the above shows the great significance and relevance of accumulating clinical experience in the successful treatment of each individual patient suffering from ACTH-ES.
Clinical case.
In November 2014, a 53-year-old patient was hospitalized with complaints of muscle weakness and increased blood pressure to 160/90mm. rtst, sweating, insomnia, redness of the face, ringing, tinnitus. , loss of appetite, dryness and bitterness in the mouth.
From the anamnesis: He considered himself sick for a year, when he first noticed an increase in blood pressure to 160/100, blood glucose to 6.5. He was on constant antihypertensive therapy, diet therapy with restriction of easily digestible carbohydrates. In June 2014, during examination, there was a compression fracture of the 8th thoracic vertebra. According to X-ray densitometry of the spine, a decrease in BMD to osteoporosis was noted. Osteoporosis was treated with zoledronic acid 5 mg (Aclasta 100 ml) intravenously. Since September 2014, he noted the appearance of increasing muscle weakness in the legs, an increase in blood pressure to 160/90mm. Hg Art., an increase in blood glucose to 9.0. In November 2014, he consulted an endocrinologist and, in connection with the above complaints, was hospitalized at the Federal State Budgetary Institution “Clinical Hospital No. 1” of the Department of the Russian Federation, where an examination revealed a decrease in K+ to 1.6 mmol/l. , decrease in sodium level to 130 mmol/l, hyperglycemia to 11.2 mmol/l.
On examination: The skin is clean and dry. Hyperemia of the face, neck. The tongue is pink with a white coating. Subcutaneous fat is overdeveloped, predominantly of the abdominal type, the distribution is dysplastic, with deposition in the shoulder girdle, supraclavicular spaces, and above the cervical vertebrae. The thyroid gland upon examination is not enlarged, upon palpation it is heterogeneous, predominantly on the left, dense, painless. There is no tremor. There are no striae. BP 137/100. mm. Hg st, pulse 78 beats/min. Stool 1-2 times a day, urination is normal.
Laboratory blood test data upon admission:
Potassium 1.60 (3.60-5.30) mmol/l Sodium 130 (135-152) mmol/l.
Clinical blood test: cells (WBC) 24. (12 4-9 10) e9 /l, Platelets (PLT) 142 (180-320) x10e9 /l, Hemoglobin (HGB) 157 (130-160) g/l Red blood cells ( RBC) 5. 23 4-5 10e12/l, ESR 4- 6-20 mm/hour.
Hormonal blood test:
TSH 0.05 (0.35-4.94) µIU/ml, T3-free 3.2 (2.63-5.7) pmol/l T4-thyroxine free 12.3 (9-19.5) pmol /L, AT-TPO 0 (up to 5.61) IU/ml, AT-TG 0.6 (up to 4.11) IU/ml, C-peptide 3.18 (0.78-5.19) pmol/ l. STH less than 0.2 mIU/l.
8 am: Adrenocorticotropic hormone 47.2 pmol/l (1.6 - 13.9)
8 am : Cortisol 3390 (138 - 635) nmol/l
23h: Adrenocorticotropic hormone 35.8 pmol/l
23h: Cortisol 3090 nmol/l
Analysis of 24-hour urine for cortisol: Cortisol 25113 (262.10 - 4083.30) nmol/day.
MRI of the brain: no focal pathology was detected.
CT scan of the chest: Small peripheral mass in the middle lobe of the right lung . (In S4 of the middle lobe of the right lung, an oval-shaped soft tissue formation of a homogeneous structure with clear, even contours is determined, p up to 7x9x7 mm). Signs of hemodynamic disturbances in the ICC. Bilateral small hydrothorax. Diffuse adrenal hyperplasia.
MSCT of the abdominal organs with contrast: In S4 of the right lobe of the liver, a hyperdense formation with smooth, clear contours is revealed, 16x19 mm, which does not accumulate the contrast agent. The right and left kidneys are of normal shape. In the middle segment of the left kidney there is a cyst measuring 16x21mm. There is uneven thickening of the left adrenal gland up to 25 mm, the body and medial peduncle of the right adrenal gland up to 10 mm. Minimal left-sided hydrothorax. Single focal compaction of the lung tissue of the right lung.
Preliminary diagnosis: ACTH-ectopic syndrome with severe hypercortisolism. Water and electrolyte disturbances: hypokalemia. Hyperplasia of both adrenal glands. Formation of the middle lobe of the right lung. Steroid diabetes mellitus on insulin therapy. Systemic steroid osteoporosis. Compression fracture of the 8th thoracic vertebra dated 06.14. Anxiety-depressive disorder. Stage II hypertension. , 3 degrees, risk 4. NK IIFC (HYHA). Superficial gastroduodenitis. Superficial colitis. Chronic pyelonephritis, remission. Left kidney cyst.
Treatment: 1. Ketoconazole 200 mg 4 times a day. 2. Veroshpiron 300 mg per day. 3. Potassium Normin 1 tab 3 times a day. (1200 mg per day) with positive dynamics.
Then the patient was hospitalized at the Federal State Budgetary Institution Endocrine Center for selective blood sampling from the lower petrosal sinuses in order to clarify the genesis of severe endogenous hypercortisolism with the development of steroid diabetes, steroid osteoporosis, arterial hypertension, hypokalemia, sharply increased cortisol content in daily urine 14496 nmol/day (up to 635), with high blood ACTH level 47.2/35.8nmol/l (up to 13.9). Taking into account the data of selective blood sampling, as well as MRI data of the brain, the presence of a central genesis of hypercortisolism is excluded, and the presence of a formation p 7, 0x9, 0x7, 0 mm in the IV segment of the right lung is indicated for surgical treatment of this formation.
On 18.12.14 the patient underwent a right median lobectomy with mediastinal lymph node dissection.
In the early postoperative period, there was a decrease in cortisol levels from 1573.4 nmol/l to 364 nmol/l, and the ACTH level decreased to 2.8 mg/ml. For adrenal insufficiency, Solu-Cortef was treated according to the following regimen: 300 mg IV (12/18/2014) and 100 mg 2 times a day. Thus, 8 days after surgery for ACTH-ectopic syndrome, the patient had clinical and laboratory data on the development of secondary adrenal insufficiency. Correction of hormone replacement therapy for adrenal insufficiency was carried out with an increase in the dose of Cortef to 40 mg per day, against which an improvement in the general condition was noted.
According to histological and immunohistochemical studies: within the material delivered for examination, there is a morphological picture of a highly differentiated neuroendocrine tumor of the lung (typical carcinoid).
CD 56 ( Cell Margue, clone 123C3), proliferation marker index Ki67 is 3.5%. рТ1р N0, cM0.
Clinical diagnosis: ACTH-ectopic syndrome with severe hypercortisolism, remission after median lobectomy on the right with mediastinal lymph node dissection on December 18, 2014. Secondary adrenal insufficiency. Steroid diabetes mellitus, compensation. Steroid osteoporosis. Compression fracture of the 8th thoracic vertebra dated 06.14. Anxiety-depressive disorder.
While receiving hormone replacement therapy, no clinical signs of adrenal insufficiency were observed. After 1.5 months, gradual withdrawal of hormone replacement therapy. During follow-up after 3 and 6 months, the hormones ACTH and cortisol were within normal limits. Normoglycemia and normalization of blood pressure are also noted.
Conclusion
This clinical case illustrates the potential difficulty of diagnosing ACTH-ectopic syndrome. In connection with the above, it is necessary to use a variety of laboratory tests and imaging methods, as well as persistently monitor patients every 6 months, even if the source of ectopic ACTH production remains undetected for many years.
Currently, for most patients with an unidentifiable source of ectopic hormone secretion, the optimal option is bilateral adrenalectomy followed by hormone replacement therapy. The operation should not be postponed, since the risks of the operation increase in parallel with the severity and degree of hypercortisolism.
RELEVANCE
The prevalence of endogenous hypercortisolism is about 5–6 cases per 1 million people, with 1–2 new cases per 1 million diagnosed annually [1].
The share of ACTH-dependent hypercortisolism in the overall structure is about 80%. Among this cohort of patients, in 70–75%, the cause of hypersecretion of adrenocorticotropic hormone (ACTH) is corticotropinoma, another approximately 10% are diagnosed with corticotroph hyperplasia, and in the remaining 15–20%, neuroendocrine tumors of various localizations producing ACTH and/or corticoliberin [1–4 ]. A patient with oat cell lung cancer and the clinical picture of hypercortisolism was first described in 1928 by W. Brown [5]. In 1960, peptides were isolated from a lung tumor with adrenocorticotropic activity, and in 1969 G. Liddle et al. proved the pathogenetic connection between hypercortisolism and the functional activity of certain types of tumors, which made it possible to identify a new disease called “ACTH-ectopic syndrome” [6].
According to epidemiological data, in 5–10% of cases, the source of ectopic ACTH production is tumors of extrapituitary localization: bronchial carcinoid tumors (36–46%), oat cell lung cancer (18–20%), pheochromocytoma (9–23%), medullary thyroid cancer glands (3–7%), tumors of the pancreas, thymus and parotid glands, ovaries, uterus, prostate, colon, stomach, esophagus and other organs [3, 7]. With ACTH-ectopic syndrome, the development of clinical manifestations, as a rule, occurs faster than with corticotropinoma, which determines the uniqueness of the clinical picture [4]. Difficulties in identifying the primary focus of ACTH hypersecretion may be due to its small size, the absence or nonspecificity of the clinical picture from the primary focus, and early metastasis in the case of malignant tumors. In addition, the most common manifestations of hypercortisolism (such as arterial hypertension, myopathy, carbohydrate metabolism disorders, including diabetes mellitus (DM), electrolyte disorders and increased protein catabolism, contributing to the development of myopathy and low-traumatic fractures, hypogonadism, etc. .) can sometimes be considered as independent nosological forms, which creates certain difficulties at the stages of early diagnosis and timely treatment of ACTH-ectopic syndrome. The given clinical case is proof of this.
CASE DESCRIPTION
Patient P., 36 years old, was admitted to the Federal State Budgetary Institution Endocrinology Center in November 2021 with complaints of increased blood pressure (BP) up to a maximum of 210/140 mmHg, pain in the chest and intercostal spaces during physical activity, swelling and numbness of the arms and legs, weight gain, burgundy stretch marks in the armpits, on the abdomen and thighs, “bruises” on the skin, prolonged wound healing, changes in appearance (rounding and redness of the face), muscle weakness, shortness of breath during exercise, fatigue, weakness, absent-mindedness , headache.
From the anamnesis it is known that in May 2015, at the age of 35 years, after minor physical activity, a compression fracture occurred in the thoracic spine at the Th5-Th6 level (according to MRI), pathological fractures of the ribs on both sides. In June 2015, when performing densitometry of the proximal femur, the Z-criterion was -0.3 SD, the lumbar spine, the Z-criterion was -1.3 SD. In October 2015, an examination revealed: diabetes, glycemia at the onset of 17 mmol/l without any clinical symptoms, regarded as type 1 diabetes, insulin therapy was prescribed; negative overnight suppression test (NST) with 1 mg of dexamethasone (blood cortisol 556 nmol/l) with a normal 24-hour urine test for free cortisol - 157.2 mcg/day (normal 4.3–176) and the absence of organic changes in the adrenal glands on CT scan with intravenous contrast; the level of methylated catecholamines in daily urine is normal. In March 2015, low testosterone levels were determined. However, despite the extensive clinical picture of hypercortisolism (striae, “bruises” on the skin, rounding and redness of the face, prolonged wound healing, muscle weakness, fractures of the vertebrae and ribs, diabetes, hypogonadism) and the absence of cortisol suppression against the background of NPT with 1 mg of dexamethasone, diagnostic and no therapeutic measures were carried out throughout the year (until April 2021).
In April 2021: blood cortisol – 1511.8 nmol/l (normal 260–720), ACTH – 38.4 mcg/l (normal 0–50), 25(OH)D – 12.5 ng/ml ( the norm is more than 30); MRI of the pituitary gland: no pathological changes in the pituitary gland were detected.