Follicle-stimulating hormone, designated by the English term FSH, is a gonadotropin consisting of more than two hundred amino acids. This hormone is secreted by the pituitary gland. In a woman’s body, the secretion of hormones depends on age and the phase of the menstrual cycle, so FSH norms vary.
In the female body, follicle-stimulating hormone is responsible, among other things, for stimulating the synthesis of estrogen and the production of progesterone. It is also a factor responsible for egg production and follicle maturation.
FSH: what is it for women
In women, this hormone regulates the development and maturation of follicles in the ovaries. Within normal limits, FSH is elevated before ovulation. It is its high level that leads to its onset - the release of the egg from the follicle.
If FSH production is disrupted and its level deviates from the norm, this can lead to infertility and other serious problems.
Therefore, the answer to the question about FSH: “what is it for the body” can be the definition - it is one of the main regulators of the normal function of the female and male reproductive system.
Cycle phases and FSH levels in the body
Phases of the menstrual cycle and levels of hormone production
the follicular phase begins (in some sources it is called estrogenic). During this period, this hormone is released. It stimulates the development of the follicle on the ovary.
Under the influence of another pituitary hormone, luteinizing hormone, the follicle cells begin to secrete estrogens.
Estrogens are steroid hormones that affect body chemistry and physiology, including tissue growth and sexual function.
When the level of estrogen in the body increases in the middle of the cycle, the pituitary gland secretes LH in large quantities and now in small quantities - follicle-stimulating hormone, the norm for which decreases these days.
The second phase of the cycle - ovulation - begins when the concentration of LH reaches a certain level.
The follicle bursts and an egg emerges, ready for fertilization. The egg is sent to the uterus - “to meet” the sperm, and the burst follicle becomes the corpus luteum.
the luteal phase begins . During this period, the burst follicle turns into a corpus luteum.
The corpus luteum begins to produce progesterone (a steroid hormone). High levels of steroids block the production of pituitary hormones. If fertilization does not occur during ovulation, the corpus luteum is destroyed. Accordingly, the level of steroid hormones decreases. When steroid levels in the body become low, the pituitary gland begins to secrete follicle-stimulating hormone and the follicular phase begins again and the menstrual cycle repeats.
If conception has occurred, the pituitary gland secretes the hormone choriogonin. Choriogonin is also called hCG (human chorionic gonadotropin). This is what the pregnancy test reacts to. Choriogonin begins to be released two weeks after ovulation and stimulates the development of the corpus luteum. The hormone progesterone, which is produced by the corpus luteum, prepares the uterus for pregnancy. The level of steroid hormones - estrogen and progesterone - increases significantly during pregnancy.
How and when to get tested for hormones
“Donating hormones,” more precisely, taking blood for sex hormones and their regulators (FSH, prolactin, LH) requires compliance with simple conditions that will help achieve an accurate result without errors and errors.
So the FSH norm in women is usually determined on days 6-7 of the menstrual cycle. To prevent the FSH test result from being lowered or falsely elevated, you should:
• Three days before taking hormonal tests, avoid intense sports activities and training;
• You should not smoke 1 hour before donating blood;
• 10-15 minutes before taking blood, you should rest and calm down, then the result will be without errors.
If these simple conditions are not followed, the result may be that the FSH level is increased or decreased. Moreover, both low FSH and a high level of this indicator in such conditions may turn out to be erroneous.
The FSH norm in women and men in the blood is determined in the morning and on an empty stomach (from approximately 8 to 11 o’clock).
Since FSH can be decreased or increased due to its pulsed entry into the bloodstream, it is recommended to take 3 blood samples at once, each with an interval of 30 minutes or more.
Deviation of LH concentration from the norm in women - what to think about?
Increased levels of luteinizing hormone in women can be a consequence of conditions such as:
- Primary dysfunction of the gonads;
- Polycystic ovary syndrome;
- Postmenopause;
- Pituitary adenoma;
- Hypergonadotropic hypogonadism;
- Precocious puberty syndrome.
A decrease in the concentration of luteinizing hormone in women may indicate the following diseases:
- Secondary (hypothalamic) amenorrhea;
- Hyperprolactinemia;
- Pituitary dwarfism;
- Sheehan syndrome;
- Denny–Morphan syndrome;
- Polycystic ovary syndrome (atypical form);
- Luteal phase deficiency;
- Obesity;
- Surgical interventions, stress, serious illnesses.
Tests for follicle-stimulating hormone: normal
Normally, FSH is highest in men in the summer.
Another important indicator is how the LH and FSH norms correlate in women. So, before the start of the first menstruation, the LH/FSH norm is 1. A year after the onset of menstruation, the LH/FSH norm is 1-1.5. Two years after the start of menstruation and until menopause, LH/FSH in women is 1.5-2. If LH or FSH is increased or decreased, this ratio changes markedly.
The FSH norm in women during the reproductive period averages 0.57 - 8.77 mU/ml.
In girls under 14 years of age, the norm can range from 0.19 to 7.9 mIU/ml.
The FSH norm in women varies during different periods from the beginning of the first menstruation, depending on the phase of the cycle. FSH is lowered more in the luteal phase of the cycle and is in the range of 1.09 – 9.2 mU/ml. FSH is increased more in the ovulatory phase and amounts to 6.17 -17.2. Compared to these figures, in the follicular phase FSH is reduced to 1.37-9.9 mU/ml.
The level of this hormone in postmenopausal women is 19.3 - 100.6 mU/ml, that is, during this period this indicator is significantly increased.
Compared to the indicators in women, in men over 21 years of age FSH is 0.95 – 11.95. In other age periods in men, FSH is reduced and can be less than 9.9 mIU/ml.
Follicle-stimulating hormone (FSH) is a glycoprotein hormone that is produced and accumulated in the anterior pituitary gland and affects the functioning of the gonads.
Synonyms Russian
FSH, follitropin, pituitary gonadotropin.
English synonyms
Follicle-Stimulating Hormone, Follitropin, FSH, Pituitary Gonadotropin.
Research method
Chemiluminescent immunoassay.
Units
mIU/ml (international milliunit per milliliter).
Determination range: 0.1 - 200 mIU/ml.
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 2-3 hours before the test (you can drink clean still water).
- 48 hours before the study (in consultation with the doctor), stop taking steroid and thyroid hormones.
- Avoid physical and emotional stress 24 hours before the test.
- Do not smoke for 3 hours before the test.
General information about the study
Follicle-stimulating hormone (FSH) together with luteinizing hormone (LH) is produced in the anterior pituitary gland under the influence of hypothalamic gonadotropin-liberating hormone. FSH secretion occurs in pulse mode at intervals of 1-4 hours. During a surge lasting about 15 minutes, the concentration of FSH exceeds the average by 1.5-2.5 times and is regulated by the level of sex hormones according to the principle of negative feedback. Low levels of sex hormones stimulate the release of FSH into the blood, and high levels inhibit it. The production of FSH is also suppressed by the protein inhibin B, which is synthesized in ovarian cells in women and in the cells lining the seminiferous tubules (Sertoli cells) in men.
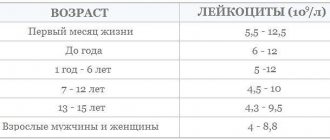
In children, FSH levels increase briefly after birth and fall very sharply at 6 months in boys and at 1-2 years in girls. Then it increases before the onset of puberty and the appearance of secondary sexual characteristics. One of the first laboratory indicators of the onset of puberty (puberty) in children is an increase in FSH concentration at night. At the same time, the response of the gonads increases and the level of sex hormones increases.
In women, FSH stimulates the maturation of ovarian follicles, prepares them for the effects of luteinizing hormone and enhances the release of estrogens. The menstrual cycle consists of follicular and luteal phases. The first phase of the cycle takes place under the influence of FSH: the follicle enlarges and produces estradiol, and at the end, a sharp increase in the levels of follicle-stimulating and luteinizing hormones provokes ovulation - the rupture of a mature follicle and the release of an egg. Then comes the luteal phase, during which FSH promotes the production of progesterone. Estradiol and progesterone regulate the synthesis of FSH by the pituitary gland via a feedback principle. During menopause, the ovaries stop functioning and decreased secretion of estradiol leads to increased concentrations of follicle-stimulating and luteinizing hormones.
In men, FSH affects the development of seminiferous tubules, increases testosterone concentrations, stimulates the formation and maturation of sperm in the testicles and promotes the production of androgen binding protein. After puberty, FSH levels in men are relatively constant. Primary testicular failure leads to an increase in its number.
Analysis for gonadotropic hormones allows you to determine the level of hormonal regulation disorders - primary (depending on the gonads themselves) or secondary (associated with the hypothalamic-pituitary axis). In patients with testicular (or ovarian) dysfunction, low FSH levels indicate dysfunction of the hypothalamus or pituitary gland. An increase in FSH indicates a primary pathology of the gonads.
Simultaneous tests for follicle-stimulating and luteinizing hormones are used to diagnose male and female infertility and determine treatment tactics.
What is the research used for?
- To identify the causes of infertility (together with a test for other sex hormones: luteinizing hormone, testosterone, estradiol, progesterone).
- To determine the phase of the menstrual cycle (menopause).
- To diagnose the causes of spermatogenesis disorders and reduced sperm count.
- To identify primary or secondary causes of sexual dysfunction (pathology of the gonads or hypothalamic-pituitary disorders).
- For the diagnosis of early or late puberty.
- To monitor the effectiveness of hormone therapy.
When is the study scheduled?
- For infertility.
- If pathology of the pituitary gland and sexual dysfunction are suspected.
- In case of menstrual irregularities (its absence or irregularity).
- When the patient has congenital diseases with chromosomal abnormalities.
- For growth and maturation disorders in children.
- When using hormonal drugs.
What do the results mean?
Reference values
| Floor | Cycle phase | Reference values |
| Male | 1.5 - 12.4 mIU/ml | |
| Female | Menstrual (1-6th day) | 3.5 - 12.5 mIU/ml |
| Folliculin (proliferative) (3-14th day) | 3.5 - 12.5 mIU/ml | |
| Ovulatory (day 13-15) | 4.7 - 21.5 mIU/ml | |
| Luteal (15th day - beginning of menstruation) | 1.7 - 7.7 mIU/ml | |
| Postmenopause | 25.8 - 134.8 mIU/ml | |
| Premenopause | 1.7 - 21.5 mIU/ml |
Menopause. Reasons for increased FSH levels
- Primary ovarian failure (premature ovarian failure syndrome, ovarian dyskinesia syndrome, ovarian tumors and cysts, Shereshevsky-Turner syndrome, Swire syndrome, insufficient production of steroid hormones by the ovaries - 17-alpha-hydroxylase deficiency).
- Primary testicular failure in men (testicular aplasia or agenesis, Klinefelter syndrome, testicular tumors).
- Hypogonadism due to exposure of the ovaries or testicles to any external factors (x-rays, chemotherapy, alcohol, infectious diseases, autoimmune diseases, trauma, castration).
- Hyperfunction or tumors of the pituitary gland.
- Endometriosis.
- Testicular feminization.
- Ectopic secretion in some hormone-secreting neoplasms (usually in lung tumors).
- Premature puberty.
- Alcoholism.
Reasons for decreased FSH levels in the blood
- Deficiency of hypothalamic gonadoliberin (Kallmann syndrome - congenital secondary hypogonadism - a disorder of impulse secretion of gonadoliberin in the hypothalamus).
- Isolated FSH deficiency.
- Pituitary insufficiency.
- Dwarfism.
- Sheehan's syndrome.
- Hyperprolactinemia.
- Neoplasms of the ovaries, testes and adrenal glands with increased secretion of estrogens and androgens.
- Polycystic ovary syndrome.
- Hemochromatosis.
- Anorexia and starvation.
What can influence the result?
- Inadequate FSH levels are possible due to the patient taking radioisotope drugs, oral hormonal drugs, pregnancy, introduction of heterophile antibodies (including monoclonal) into the body, nuclear magnetic resonance scanning of the patient performed shortly before the FSH test, smoking and alcohol consumption.
- Medicines and substances that increase the level of FSH in the blood: bicalutamide, bromocriptine, cimetidine, clomiphene, danazol, digitalis, erythropoietin, finasteride, GnRH analogs, somatoliberin, hydrocortisone, ketoconazole, leuprolide, levodopa, metformin, naloxone, nilutamide, phenytoin, pravastatin, tamoxifen.
- Medicines and substances that reduce the level of FSH in the blood: anabolic steroids, anticonvulsants, carbamazepine, conjugated estrogens, corticoliberin, danazol, diethylstilbestrol, estrogen- and progesterone-containing drugs, finasteril, goserelin, medroxyprogesterone, megestrol, octreotide, oral contraceptives, phenothiazides, pimozide, prednisolone, stanozolol, toremifene, valproic acid.
When might high FSH occur?
If a woman's FSH level is high, then her periods may stop or menorrhagia (uterine bleeding) may begin, which is in no way related to menstruation. The concentration of follicle-stimulating hormone is also higher than normal in menopausal women. If a representative of the fair sex is of reproductive age, then with an increase in the concentration of follicle-stimulating hormone in her blood, we should look for the following pathology:
- ovarian exhaustion or dysfunction;
- neoplasm of the pituitary gland;
- alcohol abuse;
- increasing testosterone levels.
With a high level of FSH, pregnancy can only occur if ovulation occurs and this fact is confirmed by ultrasound.
FSH and LH are parts of the same chain
Follicle-stimulating and luteinizing hormone work in pairs, and, as a rule, tests for the content of these hormones are prescribed simultaneously - in most cases, doctors are interested not only in the concentration of FSH and LH, but also in their ratio, with the help of which they can determine the direction of the diagnostic search for the causes of endocrine pathologies , in particular, infertility. If you are found to have deviations in FSH or LH concentrations from the norm, an imbalance in their ratio, or other problems with pregnancy, contact the IVF Center in Petrozavodsk, where you are guaranteed high-quality diagnostics and consultations with highly qualified specialists.