Atherosclerosis
Diabetes
Arthritis
Gout
11758 14 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. We remind you that independent interpretation of the results is unacceptable; the information below is for reference only.
Cholesterol: indications for use, rules for preparing for the test, interpretation of results and normal indicators.
Indications
A biochemical blood test is prescribed when visiting a doctor with complaints of pain and ailments, to monitor treatment and evaluate results, as part of routine checks (medical examination, clinical examination, intravenous blood test, perinatal screening, etc.). Blood is checked for biochemistry upon admission to hospital treatment.
Lipidogram is carried out according to personal indications:
- hypercholesterolemia (high cholesterol levels), previously identified;
- hypertonic disease;
- post-infarction post-stroke period.
Patients with chronic diseases of the cardiovascular, endocrine, and hepatobiliary systems regularly donate blood for an expanded lipid profile. Cholesterol control is recommended:
- women in the premenopausal period and during menopause;
- men aged 40+;
- people with a sedentary lifestyle and nicotine addiction.
Biochemistry is a mandatory study for children with hereditary pathologies.
How is a cholesterol test done?
First, the patient takes a cholesterol test. If the values are normal, there is no need for additional research.
If the levels are elevated, an additional analysis to determine the lipid profile is prescribed.
In some cases, a lipid profile is prescribed for possible risks of cardiovascular diseases, when taking medications to reduce lipids.
The cholesterol test is carried out in the morning (before 11.00) on an empty stomach. Blood for research is taken from a vein.
To ensure the reliability of the results, the patient is recommended to follow the following rules:
- exclude fatty foods the day before the test;
- do not eat 10 hours before the test;
- two weeks before the study, stop certain medications, in particular fibrates, statins, Niacin;
- Avoid alcohol for 24 hours.
Before the study, standard preparation rules are followed.
Total cholesterol is also checked using a special test analyzer. If you have the device, testing can be done at home. Capillary blood is taken for analysis.
The main advantage of this measurement is that a person receives results within five minutes. The test analyzer is more suitable for periodic monitoring of the indicator. For a complete diagnosis, it is necessary to undergo laboratory analysis.
Cholesterol in the blood
The fat-containing alcohol cholesterol (the chemical name for cholesterol) is localized in the elastic cell membrane, acting as a protector of cells from the external environment. It participates in the most important biochemical processes that maintain the vitality of the body:
- production of bile acids and hormones (sex and steroid);
- communication between neurons of the brain and spinal cord;
- absorption of fat-soluble vitamins A, D, E.
Endogenous cholesterol is synthesized by liver cells. It accounts for up to 80% of the total. The body gets the rest from animal products.
Cholesterol metabolism
Metabolic processes are provided by high, low and very low density lipoproteins (HDL, LDL and VLDL). Their structure includes triglycerides, higher fatty acids, proteins, cholesterol, and phospholipids. Density is determined by the quantitative correlation of proteins and lipids (fats). The smaller the protein part of lipoproteins and the larger the fat part, the lower the density.
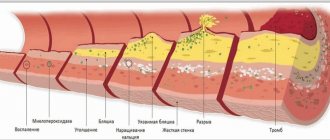
In a biochemical study, total cholesterol values are composed of lipoprotein and triglyceride values. LDL is conventionally called “bad” cholesterol, since it is low-density lipoproteins that settle on the inside of the arterial walls, forming plaques - the causes of vascular atherosclerosis. HDL (“good” cholesterol) clears blood vessels of excess free and “bad” cholesterol.
Why is analysis necessary?
Many people use the word “cholesterol” to mean a substance harmful to the body. In fact, cholesterol is present in cells and is involved in important processes. In medicine, standards for its content in the blood have been determined.
It is important to monitor the indicators and not allow them to decrease or increase. Doctors recommend checking cholesterol once every five years, and after 40 years - once every three years.
Analysis is prescribed in a number of cases:
- during a preventive examination;
- during a clinical examination;
- for diagnosing liver pathologies;
- for diabetes mellitus;
- to control cholesterol dynamics during drug treatment;
- for diagnosing thyroid diseases;
- to diagnose lipid barrier disorders;
- for the diagnosis of atherosclerosis;
- when assessing the risks of strokes and heart attacks.
The study determines total cholesterol, as well as LDL, HDL and their ratio to each other. A lipidogram is needed to provide a complete picture of the patient’s health status.
Low-density lipoproteins (LDL), also known as bad cholesterol, are dangerous. They are practically insoluble and form plaques on blood vessels. Elevated levels increase the risk of heart attack, atherosclerosis and stroke.
High-density lipoprotein (HDL), in other words, good cholesterol, plays an important role in the functioning of the body. They get rid of bad cholesterol, promote the absorption of fat-soluble vitamins, prevent the formation of plaques, and participate in the production of hormones.
Total cholesterol is the sum of the two previous indicators. A low level may indicate lipid metabolism disorders, psychophysical disorders, an increased level may indicate the risks of atherosclerosis and diabetes.
A lipid profile can provide the most accurate information about your health status. It allows you to identify the disease and identify possible risks.
The lipid profile includes cholesterol (total, bad, good), atherogenicity coefficient and triglycerides.
Atherogenic index (AI) is the proportion of total cholesterol with HDL and LDL.
The indicator assesses the state of fat metabolism and shows the possible risks of cardiovascular pathologies, atherosclerosis, and plays a role in determining liver and thyroid diseases. With the help of AI, the dynamics of changes in cholesterol during drug treatment is monitored.
Triglycerides, otherwise neutral fats, are an important source of energy that comes with food and is synthesized in tissues. These compounds can provide additional information in the diagnosis of heart attacks, atherosclerosis, vascular thrombosis, coronary heart disease and a number of other diseases.
Lipidogram and detailed biochemistry
To fully determine the lipid status (profile), lipids of various fractions are also studied in the laboratory. The purpose of the analysis is to assess fat metabolism in the body. In clinical and laboratory practice, all research parameters are designated in Latin letters.
Advanced Analysis Options
| Index | Definition, functions | Russian abbreviation | Designation in Latin |
| Total cholesterol | Set of lipid fractions | OH | Cho (Cholesterol) |
| Low and very low density lipoproteins | Transfer cholesterol molecules from the intestines and liver to cells (to ensure their functions) | LDL and VLDL | LDL and VLDL |
| High-density lipoproteins | Transport excess low-density lipoproteins and free cholesterol in the opposite direction (for catabolism in the liver and excretion from the body) | HDL | HDL |
| Trigrycerides | The body's fat reserves, consumed in the intervals between the intake and production of lipids (to replenish energy) | TG | TRIG or TG |
| Atherogenic coefficient (otherwise, index) | Shows the risk of developing vascular atherosclerosis, stroke and ischemic heart disease (coronary heart disease) | CA | I.A. |
In the forms you can find the abbreviation TC - this is how cholesterol is indicated in a blood test in some laboratories. The designations OX, TC, Cho are equivalent. The unit of measurement for total cholesterol, LDL, VLDL, HDL is mmol/l or the number of millimoles of lipid dissolved in 1 liter of blood. The atherogenicity coefficient is measured in units. It is calculated using a special formula.
Additional parameters of the lipid profile study are:
- apoproteins - proteins that are part of lipoproteins and determine which cells LDL and HDL are intended for;
- chylomicrons (CM) are a special type of lipoproteins formed in the intestines and endowed with the function of transporting exogenous fats (triglycerides and cholesterol) into the cells and tissues of the body.
Content of apoproteins, triglycerides, cholesterol and other fats in lipoproteins and chylomicrons in percent (%)
An imbalance of different density lipoproteins is called dyslipidemia. Most often, this disorder is caused by an increase in LDL concentration against the background of a decrease in HDL levels. Dyslipidemia is reflected in blood composition by hypercholesterolemia. The lipid profile indicates all parameters with specific numbers. Conventional biochemistry gives only OC results.
What to do if there are deviations from the norm
If a patient understands the indications of cholesterol levels in blood tests, they will be able to understand when treatment is needed. If deviations from normal values are small, it is enough to change your lifestyle and diet. The following measures will help normalize cholesterol levels:
- quit smoking and stop drinking alcoholic beverages;
- exclude fatty foods, sauces, fried foods, sweets, and confectionery from the diet;
- eat more vegetables and fruits;
- increase physical activity, walk, ride a bike, do gymnastics;
- Go to bed on time, avoid overtiredness.
These methods can reduce cholesterol levels by 10-15%. But if there is a serious deviation, they will not help. Therefore, it is necessary to follow the doctor’s recommendations and take prescribed medications. Statins are most often used in combination with fibrates. The doctor selects the necessary medications.
Sometimes you need to increase your cholesterol. At the same time, the amount of HDL increases, which helps prevent atherosclerosis. To do this, you also need to change your diet and lifestyle, and give up bad habits. It is recommended to consume more polyunsaturated fatty acids; they are found in vegetable oil and fatty fish. Medicines containing vitamin B3 are prescribed.
To prevent vascular disease, every adult needs to have blood tests for cholesterol every 3-5 years. In this case, it is advisable to know how it is indicated on the form. You won’t be able to fully decipher the results yourself, but you can find out whether there is a risk of cardiovascular disease. The work of many organs is associated with this substance. Therefore, any deviation from the norm indicates a serious violation of metabolic processes.
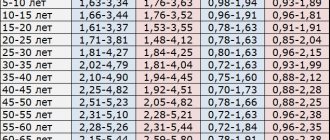
Reference values for children
Cholesterol standards are graded depending on age. The accepted values for children are lower than for adult patients, since in a child’s body:
- the reproductive and reproductive systems are not fully formed;
- the rate of metabolism of fat and sugar differs;
- the process of processing and assimilation of food is different;
- hormonal levels are unstable.
The amount of endogenous and exogenous cholesterol increases in proportion to the growth and development of the child. Accordingly, the norms of its content in the blood change.
Normal children's indicators
| Age | Up to 30 days | Up to a year | Up to 12 years | Up to 16 years old |
| mmol/l | 1,6 – 3 | 1,8 – 3,7 | 3,7 – 4,5 | 3,8 – 5,0 |
Transcript of the test
How is cholesterol indicated in tests? This question interests patients who want to independently decipher the data of a biochemical blood test. It is important to emphasize that without appropriate knowledge in the medical industry, this will be extremely difficult and sometimes impossible.
Only a specialist can give a correct assessment of the data obtained, taking into account all influencing factors such as the presence of concomitant pathologies, gender and age of the patient. Self-diagnosis can only be a temporary measure if the patient does not have the opportunity to see a doctor due to life circumstances. Personal predeterminations should not become the basis for determining the method of therapy.
Adult Cholesterol Standards
Reference TC values for men and women of fertile age are identical. The lower limit of normal is 3.2 mmol/l, the upper limit is 5.2 mmol/l. Hypercholesterolemia is considered to be results exceeding 6.7 mmol/l.
The main danger of an increased concentration of cholesterol in the blood is the development of atherosclerosis of the coronary arteries of the heart, vessels of the lower extremities, brain, and kidneys. Atherosclerotic changes in blood vessels are irreversible. If control is lost, the disease leads to heart attack, ischemic stroke, renal failure, and dry gangrene of the legs.
Cho values less than 3.0 mmol/l indicate hypocholesterolemia. With such a disorder of lipid metabolism, there is a risk of:
- destruction of cell membranes;
- vitamin D hypovitaminosis;
- dysfunctions of the reproductive and reproductive systems;
- malfunction of the autonomic nervous system.
Cholesterol deficiency provokes hemorrhagic stroke. For pregnant women, the consequences of hypocholesterolemia are miscarriage and premature birth. A slight age-related change in HDL concentration (on average, 2 mmol/l) is not a pathology. This is due to the decline of sexual activity, slowdown of metabolic processes, and general aging of the body.
Differences by gender
Lipoprotein standards are classified by gender. This is explained:
- differences in the composition, production and consumption of sex hormones;
- It is the natural nature of a woman’s body to store fat to maintain a potential pregnancy.
Female and male triglyceride and lipoprotein levels
| Options | TRIG | LDL | HDL | VLDL | ||||
| Floor | husband. | wives | husband. | wives | husband. | wives | husband. | wives |
| Norm in mmol/l | 0,41-1,8 | 2,25-4,82 | 1,92-4,51 | 0,7-1,73 | 0,86-2,28 | 0,26-1,04 | ||
Separate indicators have been adopted for the perinatal period. Cholesterol becomes the basic lipid for the formation and development of the placenta. In addition, when hormonal status changes, progesterone is synthesized in an enhanced mode - a sex hormone that protects the unborn child. Endogenous cholesterol is required for its production. The values of TC and its fractions increase from the second trimester of pregnancy.
Normal values for expectant mothers
The wave of hormonal changes during menopause also affects cholesterol concentrations. The premenopausal and menopausal periods are characterized by a gradual inhibition (followed by a stop) of the production of the sex hormone estradiol. It is replaced by estrone, synthesized from lipids, so the level of OX increases.
Indicators for women in menopause
Atherogenicity index (coefficient)
The IA symbol can only be found on the lipid profile form. The atherogenic index is not calculated as part of standard blood biochemistry. For the lipid profile the following formulas are used:
- IA= (LDL + VLDL) / HDL;
- IA= (Cho – HDL) / HDL.
The atherogenicity index reflects the degree of development (risk of development) of atherosclerotic changes in blood vessels. The obtained CA values can be deciphered as follows:
| Meaning | Analysis result | Preliminary diagnosis |
| 2-2,5 | Norm | Proper lipid metabolism |
| 3-4 | Elevated | Threat of atherosclerosis |
| >4 | High | Atherosclerosis, risk of stroke, heart attack |
An underestimated KA has no diagnostic value.
Decoding the results of a biochemical blood test
New generation laboratory analyzers are able to provide research results within two hours after blood sampling. As a rule, the patient receives the results within 2-3 days in the form of a printed or electronic table, which lists the studied indicators, their values and reference (average) normal ranges. Different laboratories offer different amounts of data, but this article will describe the most commonly tested blood parameters.
Squirrels
| Designation | Norma (women) | Norma (men) | Units | |
| Albumen | A.L.B. | < 14 years: 38–54 14–60 years: 35–50 > 60 years: 34–38 | g/l | |
| Glycated hemoglobin | HbA1c, A1c, glycosylated hemoglobin | < 5,7 | % | |
| Total protein | TP, TProt, Serum | < 1 year: 47–72 1–4 years: 61–75 5–7 years: 52–78 8–15 years: 58–76 > 15 years: 64–83 | g/l | |
| C-reactive protein | CRP, SRP | < 0,5 | g/l | |
| Iron binding capacity of serum | TIBC, IBC, OZhSS | 45,3–77,1 | µmol/l | |
| Myoglobin | Myoglobin | 12–76 | 19–92 | µg/l |
| Transferrin | Tf | 2,2–2,4 | 2–4 | g/l |
| Ferritin | Ferritin | 13–150 | 30–400 | µg/l |
Total protein characterizes the state of protein metabolism and reveals dysproteinemia (changes in the quantitative ratio of protein fractions in the blood serum). Decreased values may indicate poor nutrition, liver disease, consequences of burns, injuries and operations, while elevated values may indicate an infectious disease, non-infectious hepatitis, autoimmune diseases, dehydration, or may be caused by diarrhea and vomiting.
The protein albumin occupies up to 65% of the volume of blood plasma, is produced by the liver and performs the most important function of transporting many biologically active substances. The reasons for the decrease in albumin concentration coincide with those for total protein. The value increases quite rarely, for example, with dehydration, hemoconcentration or due to the use of anabolic steroids.
The iron-containing protein myoglobin is studied primarily for the purpose of early diagnosis of myocardial infarction. A high concentration of myoglobin may indicate myocardial infarction, heart failure, acute kidney damage, the consequences of thermal burns, and electric shock. Low myoglobin accompanies the course of rheumatoid arthritis and polio.
The value of glycated or glycosylated hemoglobin is very important for patients with diabetes mellitus and is also used for its diagnosis. Glycated hemoglobin gives an idea of the average level of glucose in the blood over a long period of time (1–2 months). If the concentration of this protein fraction does not exceed 5.7% of the total volume of hemoglobin in the blood, then we can speak of a compensated state. Values in the range of 5.7–6.4% indicate a risk of developing diabetes mellitus; values above 6.4% indicate severe decompensated diabetes.
C-reactive protein acts as an indicator of inflammation in the body. Exceeding the threshold of 0.5 g/l indicates acute inflammation or malignancy. This parameter is also important for assessing the effectiveness of antibacterial and anti-inflammatory therapy.
The studied values of transferrin , ferritin and iron-binding capacity of serum make it possible to diagnose the pathology of iron metabolism in the blood. Transferrin is the main carrier of iron; an increase in its concentration, as a rule, indicates the development of iron deficiency anemia, and a decrease indicates infections, liver cirrhosis, anemia of other etiologies, or protein starvation. In iron deficiency anemia, ferritin, on the contrary, decreases, and its increase indicates inflammatory processes, liver disease or oncopathology.
Lipids
| Designation | Norma (women) | Norma (men) | Units | |
| Triglycerides | TRIG | < 15 years: 0.40–1.48 15–30 years: 0.4–1.63 30–55 years: 0.44–2.63 > 55 years: 0.62–2.71 | < 15 years: 0.34–1.41 15–30 years: 0.45–2.81 30–55 years: 0.56–3.61 > 55 years: 0.65–3.29 | mmol/l |
| Total cholesterol | CHOL | 5,2 | mmol/l | |
| Cholesterol-HDL | HDL, HDL-C | 1,03–1,55 | mmol/l | |
| LDL cholesterol | LDL, LDL-C | 0–3,3 | mmol/l | |
Total cholesterol is used to identify primary and secondary disorders of lipid metabolism, assess the likelihood of developing atherosclerosis, and also to assess the effectiveness of treatment for atherogenic disorders of lipid metabolism. A decrease in value is caused by cachexia, starvation, malabsorption, severe acute diseases, liver failure, hyperthyroidism, and an increase is caused by primary and secondary dislipoproteinemia. The dangerous consequences of low cholesterol are psychophysiological disorders and reproductive dysfunction, while high cholesterol is diabetes and atherosclerosis. A biochemical blood test for triglycerides (products of carbohydrate metabolism in the liver) pursues the same objectives; the reasons for the increase and decrease in their concentration also coincide with total cholesterol.
and low-density lipoprotein cholesterol (HDL-C and LDL-C, respectively) are tested and interpreted in conjunction with total cholesterol and triglycerides for a more accurate diagnosis. HDL cholesterol increases in primary biliary cirrhosis, hepatitis, alcoholism, or its increase may be genetically determined. In patients with atherosclerosis, decompensated diabetes mellitus, chronic kidney disease, and cholestasis, the HDL-C value decreases. Low-density lipoproteins are involved in the processing and elimination of fats; a decrease in their concentration may indicate the development of chronic anemia, Raynaud's syndrome or myeloma, and an increase may indicate hypothyroidism, nephrotic syndrome, diabetes mellitus, porphyria, Cushing's syndrome, and the risk of developing atherosclerosis.
Carbohydrates
| Designation | Norma (women) | Norma (men) | Units | |
| Glucose | GLUC | 3,3–5,5 | mmol/l | |
| Fructosamine | FRA | 0–285 | µmol/l | |
Glucose is the main source of energy for all cells and tissues of the human body and, in particular, its only source for the brain. The glucose value in the biochemical analysis results reflects the blood sugar level. If this value is increased, then there is a possible risk of developing diabetes mellitus, damage to the central nervous system, and hormonal disorders. Glucose “falls” with the formation of tumors in the pancreas, with liver and adrenal insufficiency, hypothyroidism, malnutrition, or due to insulin intake.
fructosamine value reflects fluctuations in blood glucose levels in the 2–3 weeks preceding the test. If its concentration exceeds 280–285 µmol/l, then the doctor considers the likelihood of developing diabetes mellitus.
Inorganic substances and vitamins
| Designation | Norma (women) | Norma (men) | Units | |
| Vitamin B12 | 208–963,5 | pg/ml | ||
| Iron | Fe, IRON | < 2 years: 7–18 2–14 years: 9–22 > 14 years: 9–30 | < 2 years: 7–18 2–14 years: 9–22 > 14 years: 11–31 | µmol/l |
| Potassium | K | 3,5–5 | mmol/l | |
| Calcium | Ca | 2,25–2,5 | mmol/l | |
| Magnesium | Mg | 0,75–1,25 | mmol/l | |
| Sodium | Na | 136–145 | mmol/l | |
| Phosphorus | P | < 2 years: 1.45–2.16 2–12 years: 1.45–1.78 12–60 years: 0.87–1.45 > 60 years: 0.90–1.32 | < 2 years: 1.45–2.16 2–12 years: 1.45–1.78 12–60 years: 0.87–1.45 > 60 years: 0.74–1.2 | mmol/l |
| Chlorine | Cl | 98–107 | mmol/l | |
Vitamin B12 in the human body is involved, in particular, in the production of red blood cells. High levels of this vitamin may indicate liver disease, kidney disease, or leukemia. Diseases of parasitic etiology, inflammatory processes in the gastrointestinal tract and adherence to a vegetarian (vegan) diet, on the contrary, lead to a decrease in the level of vitamin B12 in the blood.
In one of the previous paragraphs it was mentioned that iron takes part in the process of oxygen transport. Its deficiency is usually explained by poor nutrition or metabolic disorders, and its excess is usually explained by functional intestinal disorders.
Potassium is responsible for regulating water balance and normalizing heart rate. Potassium deficiency occurs due to improper or insufficient nutrition, vomiting, renal failure, Cushing's syndrome, osmotic diuresis, chronic kidney disease, and also accompanies long-term use of steroid drugs. Potassium increases with acute dehydration, extensive injuries and burns, chronic adrenal insufficiency, diabetic coma, or due to taking potassium-sparing diuretics.
Calcium is involved in the formation of bone tissue and is extremely important for the normal functioning of muscles, nerves, heart muscle and blood vessels. Low blood calcium values indicate vitamin D deficiency, functional kidney disease, pancreatitis, impaired magnesium metabolism, or hypoparathyroidism. An increase in calcium levels accompanies hyperparathyroidism or is a symptom of cancer.
Magnesium performs the function of intracellular metabolism and transmission of impulses from nerve endings to muscles. Poor nutrition, impaired absorption, prolonged diarrhea, colitis, enterocolitis and dyspepsia reduce the concentration of magnesium in the blood. Its increase is caused by functional kidney disorders, hypothyroidism, lactic acidosis and neoplasms.
Along with magnesium, sodium , which also takes part in calcium metabolism, is responsible for transmitting impulses to muscles. The cause of sodium reduction may be hypothyroidism, Addison's disease, diabetes mellitus, kidney and gastrointestinal diseases, congestive heart failure, taking gentamicin, and less commonly, Parhon's syndrome or hypercalciuria. High sodium levels in biochemistry results indicate dehydration, oversaturation of the body with salts, diabetes insipidus or kidney disease with oliguria.
Normal functioning of the nervous and musculoskeletal systems is impossible without a sufficient amount of phosphorus in the body. The phosphorus content in the blood increases with hypoparathyroidism, excess vitamin D, rhabdomyolysis, bone diseases or poor diet, and less often with acromegaly. On the other hand, hypovitaminosis D, hyperparathyroidism, kidney transplantation, intravenous infusions of glucose, and respiratory alkalosis cause a decrease in the concentration of phosphorus in the blood.
Chlorine performs the functions of maintaining the acid-base balance of the blood and osmotic pressure. The most obvious reasons for a decrease in chlorine levels are profuse sweating, vomiting, diarrhea, incorrect treatment with diuretics; less commonly, a decrease is caused by nephrotic syndrome and hypokalemic metabolic syndrome. An excess of chlorine in the blood can be a consequence of dehydration, swelling, alkalosis and cardiac decompensation.
Example of blood biochemistry results
Low molecular weight nitrogenous substances
| Designation | Norma (women) | Norma (men) | Units | |
| Creatinine | CREA | 53–97 | 62–115 | µmol/l |
| Uric acid | U.A. | < 14 years: 120–320 > 14 years: 150–350 | < 14 years: 120–320 > 14 years: 210–420 | µmol/l |
| Urea | UREA | 2,2–6,7 | 3,8–7,3 | mmol/l |
Urea and creatinine are studied in combination; their values reflect the functional state of the patient’s kidneys, in particular, the degree of impairment of filtration and excretory functions. High values indicate kidney problems, but may be due to excessive exercise, a high-protein diet, prolonged fasting, or thyroid disease. Low urea values may be due to a low protein diet, pregnancy, and liver disease.
The level of uric acid , as an auxiliary parameter, reflects the body's ability to remove waste products from the metabolic processes of nucleic acids and purines. Of particular diagnostic interest for patients with gout. The main causes of increased uric acid are gout and alcoholism, and less commonly, kidney and liver pathologies. Low values of uric acid in the results of a biochemical blood test are much less common and, as a rule, indicate improper or insufficient nutrition.
Pigments
| Designation | Norma (women) | Norma (men) | Units | |
| Total bilirubin | BILT | 3,4–17,1 | µmol/l | |
| Direct bilirubin | BILD, D-BIL | 0–7,9 | µmol/l | |
| Bilirubin indirect | ID-BIL | BILT - BILD | µmol/l | |
The yellow pigment bilirubin begins to accumulate in the blood during diseases and hereditary pathologies of the liver and biliary tract, for example, with Gilbert's syndrome. Indirect bilirubin may also increase in some anemias and malaria.
Enzymes
| Designation | Norma (women) | Norma (men) | Units | |
| Alanine aminotransferase | ALT | < 31 | < 41 | units/l |
| Amylase | AMY | 28–100 | units/l | |
| Pancreatic amylase | AMY-P | 0–50 | units/l | |
| Aspartate aminotransferase | AST | < 32 | < 40 | units/l |
| Gamma glutamyl transferase | GGT | 6–42 | 10–71 | units/l |
| Creatine kinase | CK | 0–25 | units/l | |
| Lactate dehydrogenase | LDH | 250 | units/l | |
| Lipase | LIP | 0–190 | units/l | |
| Phosphatase alkaline | A.L.P. | 0–240 | 0–270 | units/l |
| Cholinesterase | CHE | 5860–11800 | 5800–14600 | units/l |
A liver enzyme with an unpronounceable name, alanine aminotransferase, is involved in amino acid metabolism. The indicator increases with myocardial infarction, acute hepatitis A and B, and other liver diseases.
The enzyme amylase is produced by the salivary glands and pancreas and is responsible for the digestion of carbohydrates. Exceeding the norm by 3–5 times may indicate acute appendicitis, peritonitis, gastric and duodenal ulcers, cholecystitis. In acute pancreatitis or exacerbation of its chronic form, the amylase value increases 10–30 times. An increased value of pancreatic amylase allows for timely detection of complications from operations on the abdominal organs and pancreatic diseases.
The concentration of the enzyme aspartate aminotransferase in a person’s blood increases greatly in case of damage to the liver or heart muscle; due to alcohol abuse, the levels can double the normal level.
High levels of the gamma-glutamyltransferase are observed in patients with acute hepatitis, extra- and intrahepatic cholestasis, alcoholism, pancreatic and prostate cancer, and primary liver tumors.
An increase in the concentration of creatine kinase in the blood may indicate myocardial infarction, muscle damage of various origins, and renal failure. Lactate dehydrogenase increases in diseases of the cardiovascular system, liver and kidneys, as well as in pregnant women. High lipase are observed in patients with acute pancreatitis, intestinal infarction, biliary colic, wounds, fractures, and breast cancer. The metabolism of phosphorus in the body is directly related to the content of alkaline phosphatase - its increase accompanies acute viral and alcoholic hepatitis, liver cirrhosis, mononucleosis, liver cancer or liver metastases. Cholinesterase decreases in liver cirrhosis, liver failure, hepatitis, myocardial infarction. The value of cholinesterase is also indicative for patients taking muscle relaxants.
Results
Indicators of cholesterol, lipoproteins and triglycerides in the blood are a marker of fat metabolism processes and the threat of developing serious diseases. In the analysis forms, the study parameters are indicated in Latin:
- Cho (Cholesterol) – concentration of total cholesterol;
- LDL and VLDL – low-density and very low-density lipoproteins (LDL and LDLNP);
- HDL – high-density lipoproteins (HDL);
- TRIG or TG – triglycerides.
The IA sign means the atherogenicity index, reflecting the danger of atherosclerotic vascular pathology.
Explanation of meanings
Normal cholesterol levels are in the range of 3-5.4 mmol/l. At levels of 5.5-6.5 mmol/l, moderate hypercholesterolemia is determined; more than 7.9 mmol, high hypercholesterolemia is diagnosed.
Acceptable values for HDL are from 1.2 mmol/l, for LDL – from 2.5 to 4.3 mmol/l.
In Latin it is designated: cholesterol - CHOL, bad cholesterol - LDL, good cholesterol - HDL.
The norm for the atherogenic index is from 2 to 2.9. The maximum permissible value for women is 3.2 units, for men – 3.5 units. In people with severe atherosclerosis, AI is 4-7 units.
The atherogenicity index is written in the analysis in Latin letters - CATR.
The acceptable level of triglycerides is 0.55 – 2.25 mmol/l. At levels of about 2.27 mmol/l, there is no danger of developing cardiovascular pathologies if the cholesterol complex is normal.
The Latin designation for triglycerides is TRIG.
Determination of the atherogenic index
The study of a certain atherogenicity index allows you to obtain an accurate, informative picture in determining the relationship between the concentration of good and bad substances.
When calculating the value, a simple formula is used that involves calculating the HDL value from the total cholesterol content. The resulting number must be divided by the LDL level.
Attention! The normal atherogenic index for men and women aged 30 to 560 years can range from 2 to 3.7 units. Indicators above 3 units may indicate the risk of possible development of coronary heart disease. An indicator below the acceptable level is rarely observed in patients of this age group. Absence of a value or a zero result is a good sign of vascular health, provided that LDL and HDL values fluctuate within acceptable limits.