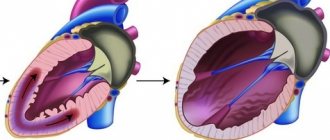
The effect of gravity when changing body position forces the circulatory system to work differently. In a split second, up to 800 ml of blood flows into the lower extremities, and venous return to the heart, cardiac output and blood filling of the cardiac cavities decrease. If the cardiovascular system is not functioning properly, a sudden change in body position can cause severe dizziness, sudden jumps in blood pressure, and fainting. In such cases, the patient may be recommended to undergo a test such as an orthostatic test .
Research methodology
Special electrodes or branches are attached to the patient's chest and limbs, transmitting electrical vibrations that occur on the surface of the skin.
A total of six branches are used, three of them are installed on the anterior chest in the projection of the heart and three on the limbs. In some cases, additional branches are used. The electrocardiograph receives information from installed electrodes, which show different amplitudes of oscillations. The data from each electrode is recorded by an electrocardiograph and displayed on paper tape with a millimeter mark in a graphical image. The paper medium moves at a certain speed. Modern devices allow you to display the received data on a monitor and record the results on digital media. In the finished electrocardiogram
information from all electrode branches is summed up.
Cardiogram
The following electrical parameters of the heart muscle are reflected:
- the location of the electrical axis of our heart;
- heartbeat rhythm;
- physiological parameters of the heart;
- arrhythmias and other pathological disorders of the heart rhythm;
- various changes associated with disruption of the electrophysiological functions of cardiac tissue, insufficient conductivity, slow metabolism, etc.;
- myocardial damage in acute or chronic form.
ECG
allows for early diagnosis of atherosclerotic lesions of the heart vessels before the development of myocardial infarction, as well as other processes accompanied by changes in the coronary vessels (vasculitis).
Indications
The study is carried out in the following cases:
- the patient has detected abnormalities in work hearts
or there is a high risk of developing pathologies;
- there is shortness of breath;
- constant pain in the sternum or in the heart area;
- presence of changes in arrhythmias;
- in the presence of dizziness, headaches;
- study of the effectiveness of the installed cardiac stimulator;
- the presence of a heart murmur ;
- for chronic diseases of the cardiovascular system, when the patient develops alarming symptoms;
- when planning surgical intervention;
- performance evaluation hearts
during pregnancy;
- undergoing medical examination after 45 years;
- passing medical examinations;
- fainting, sudden weakness;
- for various pathologies of the endocrine system, nervous system, as well as internal organs, in cases of high probability that the heart is affected by these processes;
- in the presence of cardiovascular pathology on the father's or mother's side.
ECG
It is recommended to do this if cholesterol increases and in other cases when blood counts differ from the norm. Patients over 40 years of age should have their heart function monitored annually. Elderly people, pregnant and nursing mothers, as well as young patients can undergo the study.
Contraindications
Carrying out an ECG
may be difficult in the following cases:
- the patient is overweight;
- there are injuries in the sternum area;
- Excessive hair growth in the area being examined.
Electrocardiogram
with a load is not carried out in the presence of the following pathological conditions:
- chronic cardiac dysfunction;
- acute coronary circulatory disorder (ischemia hearts
);
- myocardial infarction during the acute stage;
- viral and other infectious diseases in the acute phase;
- persistent arterial hypertension with deterioration;
- increased risk of aortic dissection or rupture.
Our advantages
"Moscow Eye Clinic" is a modern medical institution that provides a full range of professional services in the field of ophthalmology. The clinic has at its disposal the best examples of modern equipment from leading manufacturers.
The Clinic employs leading domestic specialists with extremely broad practical experience. Thus, a surgeon of the highest category Natalia Ivanovna Fomenko consults at the clinic. Thanks to the professionalism of doctors and the use of modern technologies, MGC guarantees excellent treatment results and the return of vision. By contacting the Moscow Eye Clinic, you are guaranteed a quick and accurate diagnosis and effective treatment.
Where to do the research
If you notice that you have heart
, you need to seek help from a therapist or cardiologist.
The specialist will definitely write out a referral for an ECG.
In Moscow, you can get examined at the Doctor Nearby network of clinics.
The medical center employs competent diagnosticians, and high-precision equipment is installed. research is carried out at the highest professional level. If necessary, an orthostatic test is performed with an ECG.
Comfortable conditions have been created for patients; diagnostic results with interpretation are given to them
.
Prices
At the Moscow Eye Clinic you can undergo a full diagnostic examination and receive recommendations on the most effective treatment methods. A comprehensive examination of the patient (including methods such as testing visual acuity, biomicroscopy, autorefractometry, small-pupil ophthalmoscopy, pneumotonometry) costs 3,500 rubles.
The cost of performing the Norn test to determine the stability of the tear film in the Clinic is 500 rubles.
The final cost of treatment is determined individually and depends on the specific diagnosis, stage of the disease, available tests, etc.
You can find out the cost of a particular procedure by calling 8 (800) 777-38-81 and 8 (499) 322-36-36 or online using the appropriate form on the website, you can also familiarize yourself with the “Prices” section.
Make an appointment
How the study is performed
Electrocardiogram
carried out using a stationary or portable electrocardiograph.
The patient is in a supine position. To increase the electrical activity of the skin, the area of the sternum and limbs is wiped with a damp sponge. Branch electrodes are installed in the heart
, on the ankles, and on the wrists. Then the diagnostician turns on the device and begins reading information about electrical potentials.
Graphs of cardiac muscle activity are displayed on the screen in the form of an oscillation graph and recorded on a special tape. The standard duration of ECG recording does not exceed 15 minutes. The results obtained are assessed by general practitioners, cardiologists, and general practitioners. The description (decoding) of the electrocardiogram is performed by cardiologists and functional diagnostics doctors.
Running the test
The person is asked to pull back the lower eyelid with a finger and look down; at 12 o’clock the limbus area is irrigated with a drop of a 0.2% solution of a contrast agent (sodium fluorescein). The patient is then asked to step behind the slit lamp, blink calmly, and then keep the eyes open without blinking. A cobalt filter is introduced into the slit lamp lighting system, it is turned on, and the cornea is scanned in the horizontal direction through the eyepieces. The doctor’s task is to record the time of formation of the first rupture in the fluorescein-stained tear film. As a rule, it forms in the lower outer quadrant of the patient's cornea.
Preparing for the study
No special preparation is required. If there is thick hair in the chest area, it is recommended to remove hair. The day before, you can stick to your usual drinking and eating regimen. To obtain reliable results, it is not recommended to undergo diagnostics immediately after eating food, coffee, energy drinks, alcohol, or after intense physical activity. ECG accuracy
may be affected by the time of the study, extraneous electromagnetic background, location of the branch electrodes, elevated temperature in the patient, stress and other factors.
Research results
The resulting cardiogram
transferred to a cardiologist for functional diagnostics to
decipher
the information. The results are sent to the attending physician, who recommends additional research or selects effective treatment tactics.
ECG parameters are considered normal:
:
- Heart rate (number of contractions within 1 minute) - 60–80 beats/min.
- Type of heart rhythm (where the nerve impulse that causes the contraction occurs) hearts
) - sinus. In case of disturbances, the rhythm can be ventricular, atrial, or atrioventricular.
- The electrical axis of the heart (the direction characterizing the propagation of impulses) is 30–70 degrees. During pregnancy, EOS up to 90 degrees is considered normal.
Questions and answers
What is an orthostatic test with an ECG?
The Doctor Nearby clinic network uses modern methods for diagnosing cardiac activity. The difference between this type of cardiography is that during the study the patient is in an upright position. The oblique test can be passive or active. The test is carried out after a regular cardiogram
, which allows one to assess the autonomic reactivity of the cardiovascular system and monitor rhythm and conduction disturbances.
How is a drug test performed during an ECG?
The Doctor Nearby network of clinics performs electrocardiography using pharmacological drugs. ECG
is recorded against the background of administering medications to the patient that directly affect the functioning of the heart and coronary circulation.
The method is a modification of the usual procedure. During this diagnosis, blood pressure is monitored and the patient's condition is monitored. Blood pressure readings are monitored before the drug is administered, after the drug is administered, and after the drug is stopped. The method of recording an electrocardiogram
is classic.
This diagnostic method is used to detect coronary artery disease and rare heart diseases.
LONG-TERM PASSIVE ORTHOSTATIC TEST (TILT TEST) TO DETERMINE THE CAUSE OF SYNCOPAL CONDITIONS
The long-term passive orthostatic test (Tilt-test) has been performed in the Department of New Diagnostic Methods since 1991.
A long-term passive orthostatic test (LPOT) is performed on patients suffering from repeated bouts of loss of consciousness (fainting). Syncope (fainting) can be caused by diseases of the cardiovascular or nervous system, but can also be observed in the absence of any pathological manifestations in these systems. Among the many types of syncope, one can distinguish the so-called neurocardiogenic syncope . This term characterizes a group of clinical syndromes manifested by attacks of loss of consciousness and associated with the pathological reflex effect of the autonomic nervous system on the regulation of vascular tone and heart rate. This group also includes vasovagal fainting, which is a fairly common variant of short-term loss of consciousness and, according to various authors and in various categories of patients, accounts for from 28 to 93% of the total number of syncope.
Indications for performing a long-term passive orthostatic test are:
- clarification of the genesis of recurrent syncope and presyncope attacks of unknown cause;
- monitoring the effectiveness of therapy or an implanted artificial pacemaker (pacemaker) in patients with previously observed syncope.
If an examination carried out within the walls of the Institute of Cardiology, which included: a clinical examination, ECG, echocardiography, transesophageal and/or intracardiac electrophysiological study (to exclude the arrhythmic nature of fainting), a test with massage of the areas of the sinocarotid zones (to exclude carotid sinus syndrome), electroencephalography with provocative tests, examination by a neurologist, the cause of syncope has not been determined, the patient undergoes DPOP with continuous non-invasive (bloodless) monitoring of blood circulation parameters in mandatory combination with electroencephalography (EEG).
Contraindications for this study are:
- unstable angina;
- circulatory failure, starting from class II according to NYHA classification;
- severe arterial hypertension;
- condition after acute cerebrovascular accident (less than 6 months);
- severe respiratory failure;
- acute thrombophlebitis;
- acute infectious diseases;
- endocrine diseases;
- mental disorders;
The test is carried out in the morning (from 10 to 12 o'clock), on an empty stomach and against the background of withdrawal of all cardioactive and psychotropic drugs, for at least 5 half-lives.
The patient is introduced in advance to the research methodology in order to exclude pronounced manifestations of anxiety, an explanatory interview is conducted, following which the patient is asked to read and sign the “protocol of informed consent of the patient for a long-term passive orthostatic test”, developed in the Department of Clinical Electrophysiology of the Research Institute of Cardiology named after. A.L. Myasnikov RKNPK and accepted by the ethics committee of the Institute in 2000.
DPOP is performed on a special rotating (orthostatic) table, which allows the patient to be transferred from a horizontal to a vertical position and back with an adjustable angle of inclination. The table is equipped with a foot rest, a footrest to facilitate climbing onto the table and seat belts.
During the test, the following biosignals are recorded:
- ECG in standard lead II;
- Tetrapolar thoracic rheography according to Kubizek and its first derivative (differential rheogram), necessary for documenting changes in blood flow and blood supply, as indicators of “disturbing” effects on the patient’s circulatory system;
- Rheovasography of the left leg, for an objective assessment of vascular tone and blood deposition in the lower extremities;
- The signal from the chest breathing sensor to assess the frequency and depth of breathing in order to take into account the factor of hyperventilation at the time of development of presyncope and syncope;
- EEG in four bipolar leads allows you to document possible epileptiform manifestations.
For operational monitoring of blood circulation parameters during a long-term passive orthostatic test, either a computerized rheograph-polyanalyzer RGPA-6/12 with REAN-POLY software of domestic production (MEDIKOM-MTD, Taganrog) or a similar Task Force Monitor complex is used , (manufactured by CNSystem, Austria).
After applying the necessary electrodes and sensors, the patient is placed on an orthostatic table and secured with seat belts.
Initially, for at least 20 minutes, with the patient in a horizontal position, measurements and registration of background (initial) values of circulatory system indicators are carried out for operational monitoring. Then the patient is transferred to a vertical position (+ 60°) with the legs resting on the stand of the orthostatic table. In this position of the patient, the main indicators of the state of the cardiovascular system (Heart Rate, Stroke Volume, Minute Volume of Blood Circulation, Total Peripheral Vascular Resistance, Blood Pressure) were continuously monitored in real time in automatic mode for 40 minutes, or before the development of syncope.
The criteria for stopping the test (turning it into a horizontal position) are:
- development of syncope or presyncope, in which case the test result is considered positive;
- achieving the specified duration of the study.
If during DPOP it is not possible to induce a syncope (presyncope) state, the test result is considered negative.
After transferring the patient to a horizontal position, recording and monitoring of hemodynamic parameters continues for 5–10 minutes until they are completely restored.
After completion of the DPOP, the patient is given a conclusion and study protocols
LONG-TERM PASSIVE ORTHOSTATIC TEST (TILT-TEST) WITH ASSESSMENT OF FLUID REDISTRIBUTION IN DIFFERENT REGIONS OF THE BODY
In the Department of New Diagnostic Methods of the A.L. Myasnikov Research Institute of Cardiology, RKNPK, a version of a long-term passive orthostatic test (LPOT) has been developed and used to diagnose possible regions of blood deposition in patients with syncope. This test is performed to select tactics for further treatment of patients using therapeutic knitwear. The test is carried out according to a protocol developed at the Institute of Cardiology. Monitoring of the redistribution of blood volumes is carried out using the device “Analyzer for assessing the balance of water sectors of the body ABC-01 MEDASS” with ABC-501 software for assessing the redistribution of venous blood in orthostatic, pharmacological and other stress tests, developed and produced by JSC STC “MEDASS” ( Moscow city). If the DPOP result is positive (the development of syncope or presyncope during the test), the region of the patient’s body in which the maximum deposition occurred is determined.
Literature. 1. Gekht B.M., Petrenko B.E. Mechanisms of vasovagal syncope in patients with different characteristics of transient processes of the cardiovascular system. Cytolysins. In the book. “Neurology of fainting and hypoxic states of the brain” (proceedings of the 2nd Moscow Medical Institute). Ed. Erokhina L.G. – M, -1977, vol. 76, issue 6, pp. 47-58. 2. Gukov A.O., Zhdanov A.M. Carotid sinus syndrome and vasovagal syncope. II scientific and practical conference “Clinical and physiological aspects of orthostatic disorders”. Moscow, March 22, 2000, pp. 46 – 62. (www.medass.ru) 3. Erokhina L.G. Clinic and treatment of syncope in some forms of cerebral and somatic pathology. Guidelines. M. RGMU 1993. 4. Pevzner A.V., Kuchinskaya E.A., Vershuta E.V., Albitskaya K.V., Kheimets G.I., Tripoten M.I., Moiseeva N.M., Rogoza A.N., Golitsyn S.P. Possibilities of long-term orthostatic and bicycle ergometer tests in the differential diagnosis of syncope of unknown origin. Therapeutic archive No. 11, 2004, pp. 23 -27
5. Rogoza A.N., Kheimets G.I., Pevzner A.V., Pantaeva N.M., Ponomarev Yu.A., Tsegelnikova A.L., Skomorokhov A.A., Kalinichenko N.N., Noskin L.A., Chashchin A.V., Pivovarov V.V. The key factors of instability of the circulatory system during orthostatic tests are the possibilities of objective analysis. II Scientific and Practical Conference “Clinical and physiological aspects of orthostatic disorders”, Moscow, March 22, 2000, pp. 102 – 122. (www.medass.ru)
6. Rogoza A.N., Pevzner A.V., Tripoten M.I., Kheimets G.I., Skomorokhov A.A., Vershuta E.V., Kuchinskaya E.A., Atkov O.Yu. Long-term passive orthotest for neurocardiogenic syncope. IV Scientific and Practical Conference “Diagnostics and Treatment of Cardiovascular System Regulation Disorders”, Moscow, March 20, 2002, pp. 262 – 281. (www.medass.ru).