Capillaries are the smallest blood vessels that penetrate all tissues and organs of the human body. Capillaries carry blood to every cell in the body and deliver oxygen and nutrients necessary for life. Waste products pass from the cells into the blood, which are subsequently transferred to other organs or removed from the body. The exchange of substances between blood and body cells can only occur through the wall of capillaries, so they can be called the main elements of the circulatory system. When blood flow through the capillaries is disrupted and their walls change, the body cells will experience hunger, which will gradually lead to disruption of their activity and even death.
Arterioles and venules
Capillaries are the most numerous and thinnest vessels, their diameter is on average 7–8 microns. The capillaries are widely connected (anastomose) with each other, forming networks inside the organs (between the arteries delivering blood to the organs and the veins carrying blood out). The thin arteries through which blood enters the capillary networks are arterioles, and the small veins carrying blood are venules. Arterioles, especially those from which capillaries directly branch (precapillary arterioles), regulate the flow of blood into the capillary networks. By narrowing or expanding, they block or, conversely, resume the flow of blood through the capillaries. That is why precapillary arterioles are called the valves of the cardiovascular system. Venules, together with larger veins, perform a capacitive function - they retain the blood present in the organ.
Heart and blood vessels interesting facts
The length of all blood vessels in an adult is approximately 100,000 km. All blood vessels, together with the heart, form the anatomical basis for the circulatory system and thus the transport of oxygen and nutrients throughout the body.
There are different types of blood vessels:
- Aorta
- Arteries
- Arterioles
- Capillaries
- Vienna
- Venules
- Vena cava
Aorta (main arterial vessel of the systemic circulation)
The aorta comes directly from the heart and therefore bears the name of the main artery. It transports blood from the left chamber of the heart to the arterial vessels of the circulatory system.
Arteries (blood vessels that carry blood from the heart to the organs)
Arteries refer to all the blood vessels that transport blood from the heart to the body. With the exception of the pulmonary artery, which moves oxygen-depleted blood from the right side of the heart to the lungs, the remaining arteries transport oxygen-rich blood. Arteries are also called “beating veins” (literally from German “Schlagader”) or “pulsating veins” (literally from German “Pulsader”) (they are called so because the pulse can be felt in large arteries).
Arterioles (small arteries)
In the vascular system, arterioles are a transitional form between arteries and capillaries. They precede capillaries and are located behind the arteries. Arterioles can dilate and contract, and thus regulate blood flow and blood supply to organs.
Capillaries (vessels “thinner than a hair”)
Blood capillaries (hemocapillaries) connect the venous and arterial vascular systems. They are the finest branches of blood vessels and form the finest network in which the exchange of substances between blood vessels and body tissues occurs. In the lymphatic vascular system, lymphatic capillaries are the initial link of the lymphatic system where lymphatic fluid collects.
Veins (blood vessels)
Veins carry blood circulating in the body back to the heart. They are divided into deep and superficial veins, with more than 90% of all blood flowing through the deep veins. In an adult, this corresponds to approximately 8,000 liters of transferred blood daily. With the exception of the pulmonary veins, all other veins carry venous (oxygen-depleted) blood. Together with capillaries and venules, they belong to the low pressure system of the circulatory system.
Venules (small veins)
Venules are the smallest veins and can still be seen with the naked eye. For example, they are in the form of a very fine vascular pattern on the sclera of the eyes (the white membrane of the eye).
Vena cava
The vena cavae are represented in the vascular system by two large veins that collect venous (oxygen-depleted) blood from the veins of the body and carry it to the right atrium. There is the superior vena cava, which collects blood from the head, neck, chest and upper extremities. The inferior vena cava collects blood from the abdomen, pelvis and legs.
Microcirculation
Capillaries, arterioles and venules belong to microvessels, i.e. vessels with a diameter of less than 200 microns. The movement of blood through them is called microcirculation, and the microvessels themselves are called microvasculature. Microcirculation is given great importance in creating optimal modes of working organs, and in case of its violation, in the development of the pathological process. Every day, 8000–9000 liters of blood flow through the blood vessels. Thanks to constant blood circulation, the required concentration of substances in tissues is maintained, which is necessary for the normal course of metabolic processes and maintaining a constant internal environment of the body (homeostasis).
Capillary structure
The capillary wall consists of a single layer of endothelial cells, outside of which lies the basement membrane. The capillary wall is a natural biological filter through which nutrients, water and oxygen pass from the blood into the tissues and the reverse - from the tissues into the blood - the flow of metabolic products. Modern research methods, in particular electron microscopy, indicate that the capillary wall is not a passive partition and that there are special pathways for the active transport of substances through it. The transfer of substances involves the junctions between endothelial cells, special pores that penetrate the thinnest parts of the wall of the capillaries of the intestine, kidneys, endocrine glands, and vesicles for the transfer of fluids present inside the endothelial cells in the wall of the capillaries of most organs.
Blood vessels and their types
The heart and blood vessels form a closed system. The blood enclosed in the blood vessels does not come into direct contact with the cells of the organ tissues. Substances enter and exit this closed system only through the walls of blood vessels. The closed circulatory system ensures high and constant blood pressure and its rapid return to the heart.
Blood vessels are a system of closed tubes of various diameters. They perform a transport function, regulate the blood supply to organs, and carry out the exchange of substances between the blood and surrounding tissues.
Blood vessels are named based on the organ they supply (eg, the renal artery), or the bone to which they are adjacent (eg, the ulnar artery), etc.
Types of Blood Vessels
Arteries are vessels that carry blood from the heart to organs and tissues.
The largest artery in the human body is the aorta. In arteries, blood moves under high pressure.
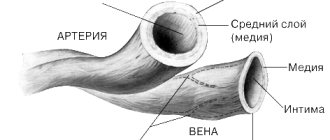
Their wall consists of three layers:
- external – connective tissue;
- medium - muscular, well developed, consisting of smooth muscle and elastic fibers;
- internal - endothelial membrane.
Such walls are strong, thick and elastic.
Usually the arteries are located deep under the muscles.
Large arteries (up to 2.5 cm in diameter) branch into smaller ones - arterioles, and then into capillaries.
Veins are vessels that carry blood from organs and tissues to the heart. Their wall, like that of arteries, consists of three layers, but it is much thinner and weaker, since it contains less smooth muscle and elastic fibers. In the lumen of the veins there are semilunar valves , which prevent the reverse flow of blood. The walls of the veins are easily compressed by the surrounding muscles, which promotes the movement of blood towards the heart, since the blood in the veins flows under low pressure.
Capillaries are microscopic vessels whose walls consist of a single layer of endothelial cells. The average diameter of the capillaries is about 7 µm, the wall thickness is 1 µm, and the length is 0.2–0.7 mm.
The total cross-sectional area of all capillaries of the body is 6300 m2.
It is in the capillaries that blood performs its main functions: it gives oxygen O2 and nutrients to tissues and carries away carbon dioxide CO2 and other dissimilation products. This is facilitated, along with a very thin wall, by the low speed of blood movement in the capillaries. Capillaries form networks connecting small arteries and veins.
The structure of the walls of blood vessels
The walls of all arteries, as well as veins, consist of three membranes: inner, middle and outer. The thickness of the walls and their tissue composition are not the same in different types of vessels.
The inner lining, the intima, consists of flat endothelial cells (endothelial cells) located on the basement membrane. In the walls of most arteries there are many elastic fibers that form an internal elastic membrane and give the arteries elasticity and firmness. In small and medium-sized (in thickness) veins, the inner membrane forms semilunar folds - valves that prevent the reverse flow of blood.
The tunica media (muscular) consists of smooth muscle cells. Arteries, compared to veins, have a well-developed muscular layer. It also contains elastic fibers that form the outer elastic membrane in some arteries.
The outer lining of blood vessels consists of loose fibrous connective tissue. It contains nerves and blood vessels that supply the walls of blood vessels.
1 – arteries 2 – capillaries 3 – veins
History of the study of the capillary network
Although blood capillaries were discovered by M. Malpighi back in 1661, their serious study began only in the twentieth century and led to the emergence of the doctrine of blood microcirculation. The idea of the exceptional importance of capillaries in meeting the needs of tissues for blood flow was expressed by A. Krog, who was awarded the Nobel Prize for his research in 1920.
Actually, the term “microcirculation” began to be used only in 1954, when the first scientific conference of scientists working on capillary blood flow was held in the USA. In Russia, academicians A. M. Chernukh, V. V. Kupriyanov and the scientific schools they created made a huge contribution to the study of microcirculation. Thanks to modern technical advances associated with the introduction of computer and laser technologies, it has become possible to study microcirculation in vivo and widely use the results in clinical practice to diagnose disorders and monitor the success of treatment.
Features of the structure of the microvasculature
Difficulties in studying microvessels for decades have been associated with their extremely small sizes and highly branched capillary networks. The narrowest capillaries are found in skeletal muscles and nerves - their diameter is 4.5–6.5 microns. Metabolism in these organs is very intense. The skin and mucous membranes have wider capillaries - 7–11 microns. The widest capillaries (sinusoids) are located in the bones, liver and glands, where their diameter reaches 20–30 microns.
The length of capillaries varies in different organs from 100 to 400 microns. However, if all the capillaries present in the human body are extended in one line, then their length will be about 10,000 km. Such a colossal length of the capillaries creates an extremely large exchange surface of their walls - about 2500–3000 square meters. m, which is approximately 1500 times the surface of the body. The number of capillaries in different organs is not the same. The density of their location is associated with the intensity of the organ’s work. For example, in the heart muscle per 1 sq. mm of cross-section there are up to 5500 capillaries, in skeletal muscles there are about 1400, and in the skin there are only 40 capillaries.
It has now been precisely established that different organs have characteristic features of the structure of the microvasculature (number, diameter, density and relative arrangement of microvessels, the nature of their branching, etc.), due to the specifics of the organ’s work. In most cases, the microvasculature consists of repeating modules, each of which serves its own section of the organ. This allows you to quickly adapt the blood supply to the organ to changes in its functioning. The complexity of the structure of the microvasculature of organs occurs gradually, along with the growth and development of the human body. The increase in the number of microvessels is timed to coincide with the intensive increase in the mass of the organ, and the structural maturation (formation of modules) of the microvasculature is completed by the time of final puberty (by 15–17 years).
Competition "bio/mol/text"-2013
This article was submitted to the competition of popular science works “bio/mol/text”-2013 in the category “Own work”.
The competition is sponsored by the visionary Thermo Fisher Scientific. The sponsor of the People's Choice Award is Helicon.
The artificial creation of living tissues, organs and even entire organisms throughout human history has been the subject of myths, legends and fantastic stories, and has haunted the human imagination. The idea of creating organs and organisms from one small piece of living tissue has its roots in ancient times. The cultural history of mankind reflects, as in a mirror, the development of views on the cultivation of organs [1]. Examples of the earliest appearance of these ideas include the ancient Greek myths about Prometheus, as well as the creation of Eve from Adam's rib in biblical stories (Fig. 1).
Figure 1. Creation of Eve. Fresco by Michelangelo Buonarroti (1508–1512).
As people's understanding of nature expanded, new scientific approaches emerged. This is evidenced by the belief of scientists of that time that a living being can be created using alchemy, reflected in the works of Paracelsus. Vivid examples in art and literature demonstrate a person’s desire to independently create life, using the opportunities that were inherent in a particular era; among them are “The Treatment of Justinian” by Fra Angelico (1439), “Faust” by Johann Goethe (1774–1831), “Frankenstein” by Mary Shelley (1818) and many others. In parallel with the development of these ideas, scientific and practical work on the creation and restoration of parts of the human body was actively going on in culture. The prerequisites for the emergence of tissue engineering as a science were the use of various materials for the mechanical replacement of a lost organ: various ivory and metal dental implants, wooden prosthetic legs, etc. But it was only the breakthrough discovery of Ross Harrison (1870–1959), namely cell culturing (that is, growing them in laboratory conditions), that became the basis of what can be considered classical tissue engineering [2].
What is considered mysticism in one century becomes scientific knowledge in another. Paracelsus
Currently, tissue engineering is working to translate the ideas of creating organs and their use in clinical medicine. Tissue engineering not only brings into reality the long-standing dreams and fantasies of mankind, but also solves the complex problems associated with replacing damaged organs in patients [3]. It is well known that a large number of patients around the world need urgent organ transplants: heart, lungs, liver, kidneys, etc., and do not always wait their turn. In addition, after transplantation of a donor organ, problems associated with graft rejection remain. In turn, tissue engineering makes it possible to create the necessary organs from the patient’s own cells, thereby preventing the body’s negative reaction to a foreign organ. A bladder grown from a patient's own cells was the first tissue-engineered organ to be transplanted into a human. This work was carried out by leading tissue engineer Anthony Atala and his colleagues in 2006 [4]. Today, using tissue engineering, scientists create skin, bones, cartilage, pancreas, elements of the cardiovascular system, etc. Also of great interest is the development of tissue-engineered blood vessels, since they are extremely necessary for performing operations for diseases as a result of which the patient has impaired blood vessel patency, and it is impossible to use synthetic prostheses [5].
You can read more about the principles and successes of tissue engineering in the article “Tissue engineering - a window into modern medicine” [6]. - Ed.
Just like creating all other organs, making a tissue-engineered blood vessel requires three main components. The first and most important component is stem cells, which are the main building material for the formation of the desired organ. The cells are taken from the patient's bone marrow, blood or other tissues and then cultured in special laboratory conditions to increase their number. The tissue from which the cellular material for cultivation is obtained is selected depending on what cells are needed to grow a given organ. A blood vessel requires at least two types of cells: smooth muscle cells, which form the wall, and endothelial cells, which line the inside of the blood vessel and protect it from clotting. In culture, cells are arranged in one layer, but in our body they are in three-dimensional space, so they need to be somehow organized and given the desired orientation. To achieve this, there are two more components in tissue engineering: a matrix and a bioreactor.
The so-called tissue-engineering matrix is the framework of a future organ and has a porous structure. Pores are necessary so that cells can be located in them, like in niches. The shape of the matrix corresponds to the shape of the organ that needs to be grown. In the case of a blood vessel, the matrix has the shape of a tube with porous walls. To create a tissue engineering matrix, it is necessary to use an absolutely safe material that does not cause any allergic or immune reactions. Also, the creation of some organs, and especially blood vessels, requires matrices that have great strength and elasticity to withstand the pressure created by the blood flow. Various polymers are most often used as materials. These include natural materials such as collagen, chitosan, hyaluronic acid, as well as synthetic polymers. Matrices made from such materials are gradually destroyed in the body (biodegradable) and replaced by new tissues of the body.
To plant existing cell cultures on a matrix and help them form new three-dimensional tissue, engineers have designed different types of bioreactors. Blood vessels are grown in a pulsating bioreactor, which creates a flow of culture fluid, thereby simulating blood flow in the bloodstream (Fig. 2). In this case, the mechanical influences to which the cells are exposed have a beneficial effect on tissue growth. Thus, a living blood vessel grows in the bioreactor, which is then implanted into the patient [7].
Figure 2. Bioreactor for growing vessels
[7]
However, it takes considerable time to grow an organ. While working on the problem of creating a blood vessel prosthesis, we were faced with the question: what to do if a patient needs urgent surgery, such as coronary artery bypass surgery, and cannot wait for his blood vessel to grow? To answer this question and find a solution to this problem, we turned to one of the tissue engineering approaches, namely growing organs in the patient’s body. How is this possible? To do this, the matrix is placed in the organ, part of which needs to be restored. Thus, the human body itself plays the role of a bioreactor, and the organ grows on a matrix in an environment favorable to it. This approach also involves the use of matrices made of biodegradable, that is, destructible material. This is necessary so that by the time the organ is finally formed, the matrix material is completely removed from the body. The formation of an organ is thus possible due to the fact that the body’s stem cells are able to migrate to areas of damage, where they actively divide and carry out tissue repair.
And the Lord God created man from the dust of the ground... Old Testament, Book of Genesis
Based on this approach, we have developed a vascular tissue-engineered graft, which is implanted in the area of the bloodstream that requires restoration. In our work we used a synthetic polymer - polycaprolactone. Since it is known that synthetic polymers are more durable compared to natural ones, they are more often used for the manufacture of tissue-engineered matrices. Polycaprolactone is known for its high strength and elasticity, as well as the fact that its destruction in the body occurs over a long period of time (more than one year) [8]. It is believed that this time should be enough for a new full-fledged blood vessel to form.
We fabricated blood vessel matrices from polycaprolactone with a diameter of 2 mm (see title figure) using the electrospinning method. Electrospinning has nothing in common with electric fishing rods and fishing, but is a method of creating very thin fibers from a polymer solution under the influence of electrostatic forces. The materials obtained by this method consist of fibers that have micro- and nanosizes [9].
The manufactured matrices consist of fibers with a diameter of about 3 microns, which intertwine with each other and thereby form a huge number of pores (Fig. 3). This structure of the material is very popular with stem cells, which are able to penetrate the wall of the porous matrix and settle in the pores as niches. Penetrating into the matrix structure, cells actively divide, grow and produce an extracellular substance consisting of collagen and other fibers, which subsequently replaces the polymer material [10].
Figure 3. Scanning electron microscopy of a polycaprolactone matrix fabricated by electrospinning.
By evaluating the mechanical properties of our vascular scaffolds, we were able to verify that they are not inferior in strength and elasticity to existing synthetic and biological prostheses that are currently used in cardiovascular surgery. This means that after implantation into the bloodstream they will be able to withstand the load created by the blood flow and will perform their function perfectly.
Since vascular matrices interact directly with blood, it is very important that the material from which they are made does not provoke the formation of blood clots. Otherwise, the resulting blood clots will obstruct blood flow, which can lead to tragic consequences. In experiments using donor blood, we determined that the matrix being developed for the restoration of a blood vessel does not cause the formation of blood clots, and therefore can be implanted into the bloodstream of a living organism.
However, for a more complete assessment of the properties of vascular matrices, they were implanted into the bloodstream of rats, namely into the abdominal aorta (Fig. 4). Over the course of a year, we observed using ultrasound analysis that the implanted matrix was permeable to blood. After that, the matrices were removed from the animals, and, evaluating them under a light microscope, they found that the entire porous wall was completely permeated with cells, between which there was intercellular substance. In addition, the entire internal surface of the matrix is covered with endothelial cells. These cells form the inner lining of all blood vessels. All this indicates the formation of a new blood vessel based on the polymer matrix.
Figure 4. Wistar rat after implantation of the vascular matrix
Our studies show that in the rat body such vascular matrices function perfectly and remain passable for a long time (Fig. 5). However, the human body is too different from the rat body, and therefore further research is needed to improve and test matrices for regenerating blood vessels. You must be completely sure that the matrices are absolutely safe for human health. Our approach to growing blood vessels is aimed at eliminating the lengthy and complex steps associated with obtaining cells from a patient, increasing their number, and culturing them on a matrix in a bioreactor. This will make it possible to quickly provide assistance to the patient and significantly reduce the cost of growing an organ. The cost of tissue-engineered organs is one of the challenges of tissue engineering because the complete creation of an organ in a bioreactor is a very expensive procedure. Therefore, in order for tissue engineering products to be available for use in medical practice, their price must be adequate.
Figure 5. Computed tomography of a vascular matrix implanted in the aorta of a rat, one year after implantation.
Currently, the world is actively working on growing almost all tissues and organs of the human body. Some of them are already in clinical use, others are still in testing and development. It is possible that rapid progress in the field of creating and restoring damaged organs will soon lead to widespread use of this technology in clinical practice and will help prolong the lives of many patients. And for some patients, tissue-engineered organs may be the last hope.
The study was conducted in collaboration with the Laboratory of Cell Technologies of the Federal State Budgetary Institution "Research Institute of Complex Problems of Cardiovascular Diseases" of the Siberian Branch of the Russian Academy of Medical Sciences, Kemerovo, Russia (under the leadership of Aleksey Sergeevich Golovkin, PhD) and the Cleveland VA Medical Center, Ohio, Cleveland, USA ( under the leadership of Doctor of Medical Sciences Yakov Lvovich Elgudin).
Functional characteristics of the capillary network
The total capacity of the capillary bed is 25–30 liters, while the volume of blood in the human body is 5 liters. Therefore, most of the capillaries are periodically switched off from the bloodstream. In humans, under resting conditions, only 20–35% of capillaries are open at a time. In a muscle at rest, no more than 40% of the capillaries are filled with blood. During physical activity, almost all capillaries of the working muscle are included in the bloodstream. Capillaries themselves are not able to change their lumen. As already mentioned, blood flow in them is regulated by narrowing or dilating blood-bearing arterioles and the use of arteriolovenular anastomoses. Observations indicate that organs are constantly replacing some functioning capillaries with others. High variability of blood flow in the capillaries is a necessary condition for the adaptation of the microcirculatory system to the needs of organs and tissues for the delivery of nutrients.
Features of blood flow in capillaries
Since the capacity of the capillary bed is very large, this leads to a significant slowdown in blood flow in the capillaries. The speed of blood movement through capillaries ranges from 0.3 to 1 mm/s, while in large arteries it reaches 80–130 mm/s. Slow blood flow ensures the most complete exchange of substances between blood and tissues. When blood moves, its cells (erythrocytes) line up in the capillary in one row, since their radius is approximately equal to the radius of the capillary. The significance of such a device becomes clear if we remember that oxygen is carried by red blood cells and its transfer to organ cells will occur most efficiently if the red blood cells are in best contact with the capillary wall. When moving through capillaries, red blood cells are easily deformed, so even the narrowest capillaries are not an obstacle for them. Unlike red blood cells, other blood cells (lymphocytes) have difficulty crossing narrow sections of the capillary bed and can clog the lumen of the capillary for some time.
With a significant decrease in the speed of capillary blood flow, red blood cells can stick together and form aggregates like coin columns of 25–50 red blood cells. Large aggregates can completely clog the capillary and cause blood to stop in it. Increased erythrocyte aggregation occurs in various diseases.
Abstract on biology on the topic “Vessels of the circulatory system: arteries, veins, capillaries” (8th grade).
The topic of the lesson is
“Vessels of the circulatory system: arteries, veins, capillaries.”
In the human body, blood continuously moves through a closed system of blood vessels in a strictly defined direction. This continuous movement of blood is called circulation
. It depends on the work of the heart, which serves as the main engine of blood. The heart pumps blood into the vessels, ensures its movement and return to the heart itself.
Circulatory system
= heart + blood vessels: arteries + veins + capillaries, which penetrate all human organs and tissues.
In humans
, like all representatives of the chordate type,
a closed circulatory system
, i.e. blood moves in our body only through blood vessels and does not spill into organ cavities and body walls.
Structure and functions of blood vessels
.
There are 3 types of blood vessels: arteries, veins and capillaries.
1. Arteries
- These are the vessels through which
blood flows from the heart to the organs.
" arterial walls
contain a lot of muscle cells, they are
very thick, multi-layered and elastic
, which allows them to withstand the pressure of blood pushed out of the heart;
« the inner layer of the walls consists of a single layer of flat epithelial cells;
« the middle layer is formed by smooth muscle tissue. He's fat
and its contraction promotes the movement of blood through the vessels;
« the outer layer of the images is dense connective tissue;
« the diameter of the vessel decreases in the direction from the heart to the organs;
“The speed of blood flow is approximately 0.5 m per second;
“blood pressure 120 mm. Hg Art.;
« blood amount: 17%.
Figure 1 – Features of the structure of arteries
2. Vienna
- These are vessels through which
blood flows from organs to the heart.
“The walls of the veins
are three-layered, less thick and elastic
than the walls of the arteries, but
more extensible;
“ The inner layer of the walls consists of a single layer of flat epithelial cells;
“ The middle layer is formed by smooth muscle tissue.
It is thin and has pocket-like valves
that prevent blood from flowing in the opposite direction;
« the diameter of the vessel increases in the direction from the organs to the heart;
“The speed of blood flow is approximately 0.2 m per second;
“blood pressure 10 mm. Hg Art.;
« blood amount: 67%.
Figure 2 – Features of the structure of veins
3. Capillaries
- these are the smallest vessels,
the walls of which are thin, single-layer, microscopic and formed only by epithelial tissue.
“ The diameter of the vessel is smaller than a hair;
“The speed of blood flow is approximately 0.05 mm per second;
“blood pressure 30 mm. Hg Art.;
« blood amount: 16%;
“they exchange fluids, nutrients and gases between blood and tissues (metabolism);
“The membranes of these cells have numerous holes that facilitate the passage of substances involved in metabolism through the capillary wall.
Figure 3 – Features of the structure of capillaries
Comparative characteristics of blood vessels
| Sign | Arteries | Vienna | Capillaries |
| Vessel function | carry blood from the heart to the organs | carry blood from organs to the heart | exchange of substances, gases between blood and tissues |
| Features of the structure of the walls | thick, multi-layered, elastic | three-layer, less thick and elastic than arteries, more extensible | thin, single-layer, microscopic |
| Availability of valves (no / yes) | No | There is | No |
| Outer layer | layer of dense connective tissue | No | |
| Middle layer of smooth muscle | thick | thin | No |
| Inner layer | consists of a single layer of squamous epithelial cells | ||
| Vessel diameter | decreases away from the heart | increases towards the heart | thinner than a hair |
| Blood flow speed, m, mm/s | 0.5 m per second | 0.2 m per second | 0.05 mm per second |
| Blood pressure, in mm. Hg Art. | 120 mm. Hg Art. | 10 mm. Hg Art. | 30 mm. Hg Art. |
| Amount of blood, in% | 17% | 67% | 16% |
Additional Information:
1. Large arteries are divided into smaller ones - arterioles
, which in turn branch into
microscopic capillaries that
intertwine all tissues.
The capillaries connect into thin venous vessels - venules
, which merge together to form
veins
.
Figure 4 – Blood vessels
2. Since the venous walls, unlike arteries, are not elastic, there is an auxiliary mechanism that promotes the movement of blood from the organs to the heart. Skeletal muscles located next to the veins stimulate blood circulation. When muscles contract, the venous vessels are compressed and push blood through. Blood cannot move in the opposite direction, since the veins have valves that open only in the desired direction. the muscle or venous pump works
Figure 5 – Venous pump
3. At the junction of the smallest arteries into capillaries there are accumulations of muscle cells. Contractions of these cells change the lumen of the vessels, open or stop the flow of blood into the capillaries. Typically, in a person at rest, only 20-30% of the capillaries are open to blood flow. During intense work, additional capillaries open and enter the bloodstream. This mechanism is especially well developed in athletes.
Figure 6 – Muscular regulators of capillary lumen
4. The largest artery of the body is the aorta. Its diameter in an adult is approximately 3-4 cm.
Regulation of blood microcirculation
How does microcirculation regulation occur? Firstly, microvessels react to stretching: when blood pressure increases, arterioles narrow and limit blood flow into the capillaries, and when pressure decreases, they expand. Secondly, sympathetic nerves approach the largest of the microvessels (but not the capillaries), and when irritated, large arterioles and venules narrow. Thirdly, microvessels are very sensitive to vasoactive substances dissolved in the blood and react even to their concentration, which is 10–100 times less than that required for the narrowing or dilation of large vessels. Thus, skin vessels show high sensitivity to adrenaline (complete closure of the lumen of arterioles occurs when its concentration in the blood is insignificant - the skin turns pale), while the microvessels of internal organs are much less sensitive, and the microvessels of skeletal muscles and the heart can expand under the action of adrenaline. Potassium, calcium, sodium ions, as well as substances that accumulate in tissues during intense activity, lead to the expansion of microvessels. Precapillary arterioles have the greatest sensitivity to the action of vasoactive substances, and large arterioles and venules have the least sensitivity.
Test work on the topic “Structure of the heart and blood vessels”
12*.
Read the text and complete the task.
BLOOD VESSELS
Arteries and veins are large blood vessels. Their inner layer is formed by flat cells tightly adjacent to each other. The middle layer consists of elastic fibers and smooth muscles. Their contraction and relaxation affects the volume of blood flowing in the vessel. This ensures the body's adaptation to physical and mental stress. The outer layer is formed by connective tissue.
Arteries are vessels through which blood moves away from the heart. The largest artery is the aorta; the blood speed in it is approximately 0.5 m/s. The walls of the arteries are formed by a large number of elastic fibers and a thick muscle layer. They are dense and elastic to the touch, do not fall off, and can withstand high blood pressure, which in a calm state is about 120 mm Hg. Art. Arteries branch into smaller vessels - arterioles, smoothly turning into the thinnest vessels - capillaries. The walls of the capillaries consist of a single layer of cells, and through them the exchange of substances and gases between blood and tissue fluid easily occurs.
From the capillaries, blood is collected first into small, then into large veins - vessels through which blood flows to the heart. The walls of the veins are thin and distensible, contain few smooth muscle cells, so a significant part of the blood accumulates in them. The speed of blood in the veins increases and amounts to 6–25 cm/s, and the pressure drops. The walls of large veins have special folds called valves. They prevent backflow of blood.
Using the content of the text “Blood Vessels”, answer the question and solve the problem.
1) What properties are characteristic of arteries?
2) Knowing the speed of blood flow in the aorta, approximately calculate the speed of blood flow in the capillaries, if it is known that the total lumen of the capillaries is 1000 times larger than the lumen of the aorta.
3) What biological significance does this blood flow rate have for respiration?
Test work on the topic: “Structure of the heart and blood vessels”
Option 2.
1.
In which organ(s) of the human circulatory system is more than 60% of all his blood simultaneously concentrated?
1)
veins
2)
arteries
3)
aorta
4)
heart
2.
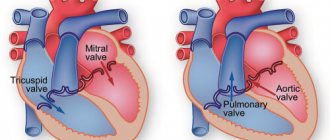
The figure shows a diagram of the structure of the human heart. What letter on it indicates the right atrium?
1)
A
2)
B
3)
C
4)
D
3.
The walls of arteries are different from veins
1)
number of layers
2)
sequence of layers
3)
structure of the inner layer
4)
more powerful outer and middle layers
4.
Through which vessel does oxygenated blood flow?
1)
pulmonary artery
2)
subclavian artery
3)
superior vena cava
4)
renal vein
5.
Which vessel does NOT contain arterial blood?
1)
pulmonary artery
2)
carotid artery
3)
femoral artery
4)
renal artery
6.
The number of heart beats per minute can be determined by measuring
1)
pulse
2)
blood pressure
3)
speed of blood movement
4)
content of red blood cells in the blood
7.
The reverse movement of blood from the ventricles to the atria of the heart is prevented
1)
pericardial sac
2)
leaflet valves
3)
septum of the heart muscle
4)
semilunar valves
8.
One of the functions of blood vessels is
1)
nutrient transport
2)
nervous regulation of internal organs
3)
skeletal muscle contraction
4)
nutrient storage
9.
Which part of the heart has the thickest wall?
1)
left ventricle
2)
right ventricle
3)
left atrium
4)
right atrium
10.
What number in the figure indicates the pulmonary trunk (pulmonary artery)?
1)
1
2)
2
3)
3
4)
4
11*.
Establish a correspondence between a blood vessel and the direction of blood movement in it: for each element of the first column, select the corresponding element from the second column.
Diagnosis of blood microcirculation disorders
Relevant for modern clinical practice, assessment of the state of microcirculation and diagnosis of its disorders in a wide variety of diseases can be done using methods such as capillaroscopy of the skin and mucous membranes, biomicroscopy of conjunctival vessels, laser Doppler flowmetry. The state of microcirculation in any part of the body makes it possible to judge its state in the body as a whole with a high degree of accuracy.
Early signs of capillary blood flow disorders are narrowing of arterioles, congestion in venules, leading to their expansion and significant tortuosity, as well as a decrease in the intensity of blood flow in the capillaries. At later stages, widespread intravascular aggregation of erythrocytes is detected, which inevitably entails a stop of blood flow in the capillaries. The final outcome of microcirculatory disorders is stasis, i.e. complete blockage of blood flow and a sharp disruption of the barrier function of microvessels, which is often accompanied by hemorrhages - the release of red blood cells through the wall of the capillaries, which are the most vulnerable. Arteriovenular anastomoses are more resistant to microcirculatory disorders and tend to maintain blood flow even in conditions of stasis spreading to a significant part of the microcirculatory bed.
Microcirculation disorders underlie a large number of diseases, so their treatment requires restoration of microvascular functions with the help of various medications.
Author: Olga Gurova, Candidate of Biological Sciences, Senior Researcher, Associate Professor of the Department of Human Anatomy of the RUDN University