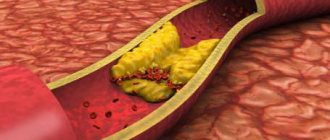
Narrowing of the carotid arteries is observed with atherosclerosis, a systemic process affecting all arteries. The main manifestation of atherosclerosis is the appearance of atherosclerotic plaques on the inner wall of the artery. These plaques are composed of cholesterol, calcium and fibrous tissue. Gradually increasing in volume, plaques narrow the lumen of the arteries and disrupt normal blood flow. When plaques form in the lumen of the carotid arteries, cerebral circulation is disrupted.
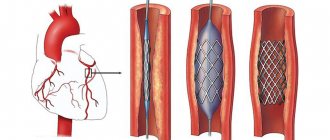
Carotid artery stenting is a procedure that involves installing a thin wire structure in the form of a cylinder into the lumen of a narrowed vessel, which plays the role of a frame - a stent. A stent is usually placed in a previously dilated artery.
The carotid arteries begin from the aortic arch. Around the middle of the neck they are divided into external and internal. The external carotid arteries supply blood to all the soft tissues of the head. The internal carotid arteries supply blood to the brain.
The appearance of plaques on the walls of the internal carotid arteries is fraught with dire consequences. Plaques are sites where blood clots form. This leads to complete blockage of the lumen of the arteries. A so-called ischemic stroke occurs. In addition, thromboembolism may develop. This condition occurs when a small blood clot breaks off from an atherosclerotic plaque, blocking the arteries of the brain. When blockage of small-caliber arteries occurs, a transient ischemic attack develops.
There are several types of surgical treatment for carotid artery disease. And one of them is carotid stenting .
Briefly about the treatment method
Endovascular surgery for narrowing of the vertebral artery, which allows you to restore the patency of the vessel and prevent the development of stroke in the vertebrobasilar region.
The carotid and vertebral arteries pass through the neck, supplying blood to the brain. Vertebral (vertebral) arteries are located in the neck and are mainly contained in the bony canals of the cervical spine. The vertebral artery stenting procedure is a minimally invasive method that provides an alternative to surgery. With stenting, a self-expanding mesh tube is placed into the artery at the site of the narrowing. When placed in a vessel, the external force of the stent reduces or completely eliminates the narrowing in the vessel. This method can be applied to vessel narrowing both in the neck and inside the skull. A stent is a tubular metal mesh whose task is to maintain vascular patency. They have been actively used since the 90s. Depending on what the stents are made of, they come in two types: balloon-expandable and self-expanding. The spreadable ones are a mesh, made of stainless steel or other metal alloys (cobalt and chromium) that resist rust. Modern meshes have a complex design and can adapt to the shape of a blood vessel and are distributed evenly and accurately inside it. Self-expanding stents are made from thin wires made of steel or nitinol (an alloy of nickel and titanium) and are characterized by their shape memory. They are less often used for stenting the vertebral artery, since during implantation they are shortened by up to 20% and cannot be held firmly in a certain position. Carotid and vertebral stents remain in place and are not detected by metal detectors. Carotid and vertebral artery stenting is much less invasive than surgery. Patients usually have a shorter recovery time. For the vertebral and subclavian arteries, treatment with angioplasty alone or angioplasty with stenting may be appropriate first-line therapy.
Discussion
CEA has proven itself as a method of surgical treatment of ICA stenoses [29, 30]. CAS is an alternative method of correction with equal effectiveness and the absence of complications such as damage to cranial nerves, laryngeal paresis, Horner's syndrome, acute hematomas at the surgical site requiring revision of the paraarterial space, which was also noted in our study [2, 10, 13 , 29, 30].
However, for each of the above methods of correction of the brachiocephalic bed there are specific indications and contraindications, thanks to which CAS, if CEA is not possible, can replace it with less likelihood of dangerous complications [10, 11, 14, 16]. Thus, in our study, clear criteria for choosing CAS were identified in most cases due to the risk of complications associated with a severe comorbid background, which is confirmed in the literature [15, 16, 22, 23, 29, 30].
Perioperative mortality in our study was 2.7% (n=2) compared with 0.7% and 0.6% in the CREST and SAPPHIRE clinical trials, respectively [15–18, 32]. Both cases are associated with a severe comorbid background of patients who had a history of repeated strokes, diabetes mellitus requiring insulin therapy, and post-infarction cardiosclerosis.
Initially, residual symptoms of stroke/TIA occurred in almost half of the patients, which was accompanied by the presence of cysts in the brain. The phenomenon of “luxurious perfusion” after hemodynamic correction aggravates this condition [20, 21, 24, 25, 27]. In addition to the listed reasons, it is necessary to note pronounced atherosclerotic changes in the aorta in the study cohort of patients, which, according to the literature, is a source of atherothrombosis during catheterization of the brachiocephalic arteries during stenting [15–18].
Myocardial infarction, according to foreign authors, is one of the main cardiovascular complications of CAS and CEA in patients with concomitant lesions of the coronary arteries, which is reflected in the presented study [1—10, 15, 17, 24, 32]. This pattern is explained by the presence of multivascular lesions of the coronary bed with high SYNTAX values and occurs due to hemodynamic changes associated with the development of bradycardia during irritation of the carotid glomus and vagus nerve, restoration of normal blood flow after correction of ICA stenosis, as well as artificial hypertension to compensate for cerebral circulation during manipulations with affected carotid artery [1, 5, 10, 29, 30]. Therefore, the cardiac status of each patient must be determined before choosing a carotid revascularization strategy.
Indications and contraindications for the treatment method
The goal of endovascular stenting surgery is to improve or restore blood flow and oxygen. Some reasons why a doctor may suggest stenting:
- The patient has high risks with open surgery.
- The patient cannot undergo general anesthesia.
- The patient has a new narrowing in the artery from previous surgery (“restenosis”).
Indications for stenting: Arteries can become narrowed (stenotic) or completely blocked due to atherosclerosis. Atherosclerosis is a disease in which fatty deposits called plaques collect inside blood vessels. As atherosclerosis develops, there is a gradual narrowing of the vessel and a decrease in blood flow to the brain. This can lead to stroke or temporary ischemic attacks. By restoring or increasing blood flow through narrowed arteries, the risk of a potentially life-threatening stroke can be reduced or prevented. Pseudoaneurysm: forms a secondary injury to the vessel wall, leading to periarterial hematoma. Arteriovenous fistulas associated with the vertebral arteries are a rare occurrence. Like pseudoaneurysms, these lesions most often occur secondary to blunt or penetrating neck trauma. Iatrogenic lesions are caused by arterial puncture with concomitant damage to the adjacent vein. Symptoms of vertebrobasilar insufficiency. Pathological tortuosity of the artery.
Contraindications Although stenting may be a better option than surgery for many patients, it is not suitable for everyone. The procedure is not performed if the diameter of the artery is less than 3 mm; the patient has severe renal and respiratory failure; the patient has vascular disease that does not allow endovascular intervention; with severe tortuosity of the artery; recent stroke or intracranial hemorrhage.
Description of a clinical case
Patient A., 54 years old, was admitted to the department of acute cerebrovascular accident (ACVA) of the Volyn hospital on October 9, 2007 with the diagnosis: “Transient ischemic attack (TIA) in the basin of the left middle cerebral artery on October 9, 2007 against the background of cerebral atherosclerosis. Hypertension stage 2, degree 3, risk 4.”
Upon admission, the patient presented acute complaints of speech impairment, weakness in the right arm and a feeling of heaviness in the head. For 15 years, he noted episodes of elevated blood pressure (up to 180/100 mmHg), took antihypertensive drugs irregularly, and smoked 1 pack of cigarettes per day for a long time.
On examination: the general condition is relatively satisfactory, the skin is clean and of normal color. There is no swelling. Heart sounds are clear, the rhythm is correct. Blood pressure 160/90 mmHg. Pulse 70 per minute. The abdomen is soft and painless on palpation. The neurological status is without features, with the exception of a slight deviation of the tongue to the left.
Taking into account the clinical picture of acute cerebrovascular accident, the patient was given appropriate drug therapy, against the background of which focal neurological symptoms regressed within 5-6 hours from the moment of onset, and the patient’s condition improved significantly. Subsequently, the patient underwent routine examination and treatment.
According to duplex scanning of the brachiocephalic arteries, stenosis was visualized at the mouth of the left internal carotid artery (ICA) with a transition to its proximal third, narrowing the lumen to 85%; velocity parameters at the mouth of the left ICA are significantly enhanced; in the distal part of the left ICA, a significantly reduced collateral type of blood flow is determined; hemodynamically insignificant narrowings are detected in the right ICA.
When performing echocardiography, hypertrophy of the left ventricular myocardium, impaired diastolic function of the left ventricle type 1 and mitral regurgitation of degree 2 were noted. The ejection fraction was 62%, and no contractility disorders were detected.
The ECG revealed changes in the myocardium of the anterolateral wall of the left ventricle and its basal section, as well as scar changes along the posterior wall of the left ventricle.
When performing an endoscopy (10/17/07), gastric erosions in the antrum were visualized, for which antiulcer therapy (omez, venter) was prescribed; on a repeat endoscopy on October 26, 2007, complete epithelization of the erosions was observed.
Taking into account the clinical picture, as well as data from additional research methods, at the consultation it was decided to perform stenting of the left ICA; in addition, taking into account the ECG data, coronary angiography was recommended.
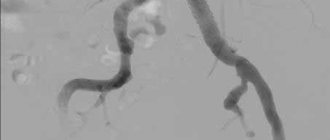
Angiography of the brachiocephalic arteries (October 29, 2007) reveals a pronounced (up to 95%) narrowing at the mouth of the left ICA (Fig. 1a), the remaining arteries are without significant changes. Coronary angiography revealed occlusion of the right coronary artery (RCA) with retrograde filling along the collaterals, 75% anterior interventricular branch (LAD) stenosis, 90% narrowing of the diagonal branch (DV) ostium, and 95% obtuse branch stenosis (OBS).
Operation description. The Angioguard (Cordis) cerebral embolism protection system was inserted into the distal third of the left ICA. Considering the presence of a critical narrowing at the orifice of the left ICA and the impossibility of safely inserting a stent, predilatation of the affected segment was performed with a 3.0x12 mm balloon catheter. The next step was stenting of the left ICA with transition to the left common carotid artery. A self-expanding stent “Precise” (“Cordis”) measuring 8.0x40 mm was implanted. Then postdilatation of the stented segment was performed with a 5.0x20 mm balloon catheter. A good angiographic result was obtained (Fig. 1b).
After the patient was transferred to the acute stroke department in the afternoon, severe hypotension was noted, which was corrected within 24 hours with dopamine infusion. The postoperative period proceeded smoothly, the patient was discharged on November 1, 2007. It is recommended to perform planned stenting of the coronary arteries after 2 months.
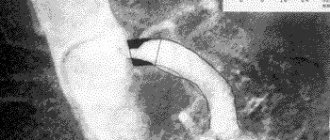
Following the recommendations, on December 10, 2007, the patient was admitted to the emergency cardiology department of the Volyn Hospital. On December 11, 2007, stenting of the VTK was performed (1 “Cypher” (“Cordis” stent was implanted) and LAD (1 “Cypher” (“Cordis”) stent was installed, followed by simultaneous balloon dilatation of the stented segment of the LAD and the ventral orifice using the “kissing balloons” technique The stages of the operation are presented in Fig. 2-3.
No complications were observed after the intervention. When performing a treadmill test (December 14, 2007), the test was negative, high tolerance to physical activity was noted, and there was no pain. At the time of discharge, she was not bothered by angina attacks.
After 17 months, the patient was admitted again for a routine examination. The patient had no complaints, no attacks of angina were noted, and there were no neurological symptoms. On control coronary angiography and angiography of the brachiocephalic arteries (03/24/2009), all stented segments were passable, and no progression of atherosclerosis was observed in other arteries (see Fig. 4).
How the treatment method works
The patient is connected to equipment with which his vital parameters will be monitored. A drug that reduces blood clotting is injected intravenously. If installed, a balloon-expandable stent is inserted through an introducer (an accessory device, a plastic tube with a sleeve). The introduction takes place under angiographic control. When the stent reaches the desired location, it is inflated with a balloon. When installing a self-expanding stent, a catheter is inserted through the introducer and the stent is delivered to the desired location. The catheter is then removed and the stent is deployed. After some time, the stent takes the required shape. The operation lasts on average 1-2 hours.
Postoperative period after carotid artery stenting
Immediately after surgery, the doctor applies pressure to the catheter insertion site for 15-30 minutes to prevent bleeding. After surgery, it is recommended to stay in bed for several hours so that the doctor can monitor the occurrence of complications. It is recommended to limit heavy lifting for a while. After surgery, it is not recommended to take baths (you can shower). The doctor will also advise you to drink plenty of fluids to quickly remove the contrast agent from your body. After carotid stenting surgery, it is recommended to take blood thinners (aspirin). In addition, it is periodically necessary to monitor the condition of the carotid arteries using duplex ultrasound scanning.
Possible complications during treatment
Immediate complications occur in 9% of patients. Embolic complications with a closed stent placement are caused by dissection or rupture and embolization of the atherosclerotic plaque; embolic strokes and postoperative transient ischemic attacks rarely occur. The stent may be thrombosed. Complications also include: Acute asymptomatic thrombosis after stent deployment. Recurrent bleeding after initial hemostasis. Subacute thrombosis and intimal hyperplasia leading to stent stenosis or vascular occlusion. The graft material may delay endothelialization, leading to thrombotic closure of the stented vessel. In addition, injured vessels are hypercoagulable.
Stenting of the vertebral arteries in Germany: progress of the operation
The procedure is performed under local anesthesia.
The stent is a special folding frame, which, when folded, is delivered to the site of narrowing and then straightened. Modern stents have a special design that allows it to be correctly positioned in the vessel and, when extended, to take the shape of the vessel.
The stent is inserted through the skin into the arterial system using a catheter and advanced into the vertebral artery. When the stent reaches the site of narrowing, it expands itself (if it is a self-expanding stent), or with the help of a special balloon. Thus, a frame is created from inside the vessel that supports the walls of the artery.
The operation is carried out under constant visual control, which is achieved using special equipment.
Recovery after surgery
After stenting of the vertebral arteries has been performed in Germany, the patient usually goes home the very next day.
At first, it is forbidden to take a hot bath or lift weights. Then the person can lead a normal life.
After three months, a follow-up examination is usually scheduled, which must be repeated several more times throughout the year.
Stenting of the vertebral artery provides long-term positive results. However, after the operation it is necessary to make lifestyle adjustments and adhere to a diet. Otherwise, atherosclerosis of the vertebral artery may reoccur over time.