Stenting of the lower extremities is a treatment method based on strengthening the vascular wall with a special metal structure - a stent. Critical ischemia and gangrene of the lower extremities have long been treated only with open bypass surgery. Despite all the positive qualities, bypass surgery has one drawback - it is a large open operation with incisions to access the vessels. This creates risks of complications associated with major interventions in patients with gangrene. Endovascular methods have made it possible to effectively treat critical ischemia in patients with concomitant lesions of the coronary, renal and carotid arteries of the brain.
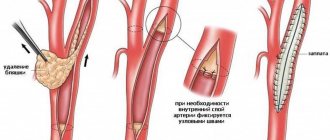
The development of medical technologies has made it possible to minimize surgical trauma using endovascular interventions through skin puncture and without incisions. The main endovascular operations are angioplasty of the lower extremities and installation of stents in the vessel. The purpose of vascular angioplasty is to inflate a narrowed or blocked segment using a special balloon passed through a thin guide. After angioplasty, a special metal mesh, a stent, can be installed into the lumen of the restored vessel to support the wall. Historically, laser angioplasty was used to destroy plaque in blood vessels, but this has given way to new, advanced endovascular instruments.
What is angioplasty
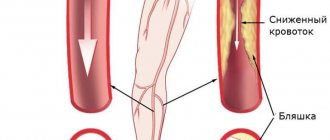
With atherosclerosis, dense plaques of cholesterol form on the walls of the arteries of the lower extremities. They block and narrow the lumen, disrupt the blood supply to the legs, leading to complications: oxygen starvation of tissues, brain, heart muscle, necrosis, trophic ulcers.
The main signs of the disease at stages 3–4 (“critical ischemia”):
- aching or sharp pain in the leg when walking and physical activity;
- numbness, tingling in the calves;
- pale skin;
- reduction of the fat layer, muscle fiber atrophy;
- excessive hair loss;
- change in the shape of nails, keratinization on the heels and toes;
- the appearance of non-healing ulcers.
Surgical angioplasty is a minimally invasive operation that restores the lumen of a damaged vessel. The method is endovascular and does not require long-term hospitalization of the patient in a hospital. Cardiac surgeons have developed several methods to normalize blood flow without painful incisions.
City Hospital reports!
Obliterating atherosclerosis, causes
Obliterating atherosclerosis is the appearance of cholesterol plaques in the thickness of the walls of the arteries, leading to narrowing and blockage (obliteration) of the artery and disruption of the blood supply to the organ or tissue that the altered artery supplies.
Atherosclerotic plaques can occur in any arteries of the human body, including those found in the arteries of the lower extremities. This leads to the development of a disease - obliterating atherosclerosis of the lower extremities.
The occurrence of atherosclerotic plaques occurs due to many reasons. The role of metabolic disorders in this process, in particular disorders of fat metabolism in the body, is important. Genetic predisposition to this disease also plays a role, as well as such important factors as smoking, diabetes, poor diet, sedentary lifestyle, obesity, high blood cholesterol, and arterial hypertension. Among patients with obliterating atherosclerosis of the lower extremities, men significantly predominate.
According to the Ministry of Health of the Russian Federation, 5-15% of the population suffers from chronic obliterating diseases of the lower extremities.
The main age of patients with obliterating atherosclerosis of the lower extremities is 60-69 years in men, 70-79 years in women, but atherosclerosis has recently become rapidly “younger”.
Symptoms of obliterating atherosclerosis of the arteries of the lower extremities
The most common symptom of atherosclerotic lesions of the arteries of the lower extremities is intermittent claudication. Patients note pain, cramps, numbness that occurs when walking and goes away at rest, in the muscles of the thigh, gluteal region (high intermittent claudication), and lower leg (low intermittent claudication). This is a sign that at rest the muscles of the lower limb are sufficiently supplied with blood, and during physical activity the narrowed artery cannot deliver enough blood, and oxygen starvation occurs.
With further narrowing of the artery, up to its complete blockage (occlusion), pain begins to appear even with less load (a clear criterion is the distance traveled after which pain appears), then they continue to bother you even at complete rest. In this case, a lower position of the leg helps relieve pain. Pain at rest indicates a complete blockage of the artery; in this case, the blood supply is provided by collaterals - small arteries running in parallel, bypassing the blocked (occluded) artery.
With further aggravation of the condition, non-healing ulcers begin to appear on the skin, they gradually increase in size and deepen until they die completely - gangrene. Gangrene usually begins with the toes; in the absence of adequate treatment, the height of the spread of gangrene is determined by the level and degree of changes in the arteries.
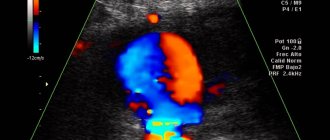
One of the simplest and most objective studies of the extent of arterial damage is ultrasound duplex scanning of the arteries. Using an ultrasound sensor, you can see both the narrowed areas and the degree of their narrowing. When, due to the deterioration of the patient’s condition, it becomes clear that surgery is no longer possible, angiography is performed - an X-ray examination of the vessels through a puncture, using a catheter and a contrast agent.
Treatment of obliterating atherosclerosis of the lower extremities
Treatment tactics for each patient are developed individually and depend on the level, extent and extent of arterial damage, and the presence of concomitant diseases. However, there are general patterns that correspond to the severity of symptoms:
Intermittent claudication suggests the presence of a narrowed section of the artery. In most situations, endovascular treatment is effective: dilatation or stenting of a narrowed arterial vessel.
For pain at rest, it is assumed that there is a completely blocked section of the artery with blood supply to the leg through collaterals. In this case, endovascular treatment is used if it is possible to pass a catheter through the blocked area - which is often only possible with small blockages (occlusions). For long occlusions, surgical treatment methods are more applicable: open removal of atherosclerotic plaques (endarterectomy), or replacement of the affected area with a vein or tissue prosthesis (bypass surgery). In case of multiple lesions, combined operations are often used - bypassing the occluded section of the artery and dilatation (or stenting) of the narrowed one.
The presence of ulcers or gangrene is a sign of extensive arterial occlusions, multi-level lesions of arteries with weak collateral blood flow. Surgical treatment options in this case are reduced. Endovascular treatment can be used in combination with open surgery. If it is impossible to perform arterial reconstruction, or if it is ineffective, amputation of the affected limb is performed.
Important! The smaller the atherosclerotic damage to the artery, the simpler, more successful and cheaper the treatment. Therefore, the most favorable stage for treatment of obliterating atherosclerosis of the lower extremities is the stage of intermittent claudication.
If the described symptoms occur, urgent consultation with a vascular or endovascular surgeon is necessary. By postponing the start of treatment “until better times,” you contribute to the progression of the disease and increase the likelihood of amputation in the near future.
Endovascular treatment of obliterating atherosclerosis of the arteries of the lower extremities
In the cath lab, under completely sterile conditions, the endovascular surgeon punctures the femoral or other artery and inserts a catheter into the artery. The catheter is brought to the affected arterial area, a contrast study is performed - angiography, which makes it possible to clarify the extent and degree of narrowing (occlusion). A conductor is passed through the affected area - a metal string with a soft tip. A catheter balloon is installed along the guide into the affected area - a catheter with a plastic balloon inflated under high pressure to a strictly defined diameter. Then the balloon is inflated (dilated) at the site of narrowing. In this case, atherosclerotic plaques are pressed into the artery wall and smoothed out evenly, the lumen of the vessel increases. Control angiography is performed. If restoration of arterial patency is satisfactory, the procedure is completed. If a narrowed or closed area remains (elastic narrowing, external compression, bending), a stent is installed at the site of the lesion - a mesh metal structure, expanded by a balloon and reinforcing the lumen of the artery from the inside, preventing it from collapsing. After the patency of the artery is restored, the endovascular instruments are removed from the artery, the puncture site is pressed with a hand for 5-10 minutes (until bleeding from the puncture site stops), then a pressure bandage is applied and bed rest is prescribed until the next morning. Anticoagulants (heparin, fraxiparin, clexane) can be prescribed for several days, after which the patient continues to take the long-term antiplatelet agent prescribed for this disease (thrombo-ASA, aspirin-cardio, cardiomagnyl, cardio-ASA).
results
Immediately after restoration of arterial patency, the volumetric velocity of blood flow in the arteries of the limb increases, and the pulse is restored in the underlying arterial segments. If a limb has been left for a long time under conditions of insufficient blood supply, restoration of blood flow can lead to the so-called hyperperfusion/reperfusion syndrome. Unusually high blood flow causes redness of the limb, swelling, and sometimes pain. This condition goes away after a few days, after the limb “gets used” to the new conditions of blood supply.
Side effects, complications, relapses
In the presence of arterial lesions of both lower extremities, restoration of blood flow in one of them can lead to depletion of blood flow in the other. As a result, after surgery, intermittent claudication may appear on a limb that was previously considered healthy (which is a manifestation of the presence of previously undiagnosed obliterating atherosclerosis in it). Therefore, it is important to initially examine both limbs, even if painful symptoms are present on only one side.
The most common complication during endovascular interventions is puncture site hematoma. This complication does not require additional hospitalization; in the vast majority of cases it is treated conservatively.
Complications at the site of arterial damage (arterial thrombosis, partial or complete rupture of the artery) are relatively rare, their frequency depends on the experience of the surgeon, the quality of equipment, instruments and the severity of arterial damage. For example, the presence of calcification (long-existing arterial plaques accumulate calcium) increases the likelihood of rupture of the arterial wall when it dilates. In most cases, such complications can be eliminated endovascularly, or, if necessary, with open surgery.
Re-emergence or worsening of symptoms of arterial insufficiency can be caused by repeated narrowing of the dilated arterial segment or growth of the intima (inner lining of the artery) at the site of the stent. In this case, repeated endovascular interventions are performed, and if they are ineffective, surgical treatment is performed. However, most often, repeated narrowing of the arteries of the lower extremities is associated with the progression of atherosclerosis.
Continued growth of atherosclerotic plaques may create the need for repeated endovascular or surgical interventions. Therefore, it is especially important for patients with obliterating atherosclerosis to correct risk factors for the progression of atherosclerosis: strive to normalize blood pressure and blood cholesterol levels, quit smoking, follow a certain diet, change the mode of physical activity - that is, completely, sometimes radically change their lifestyle. All this is necessary in order to stabilize and slow down the further development of atherosclerosis. Only in this case, the results of any treatment for arterial insufficiency of the lower extremities will be long-term.
Clinical cases
Clinical case No. 1
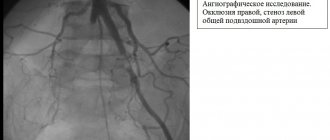
A patient complained of intermittent claudication and pain in both legs occurred at a walking distance of 50 m.
The angiogram shows pronounced stenoses of the common iliac arteries on both sides (Fig. 1).
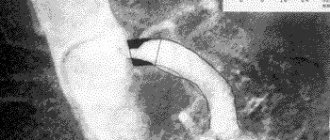
Balloon-expandable stents were installed into the areas of stenosis under local anesthesia through radial access (puncture on the forearm) (Fig. 2 and 3).
rice. 1 pic. 2 fig. 3
Stenoses were completely eliminated (Fig. 4).
Pain in the legs with minimal exertion no longer bothers the patient.
The pain-free walking distance has increased significantly.
rice. 4
Clinical case No. 2
A patient with diabetes mellitus complained of a non-healing trophic ulcer on the foot, in the bed of the removed 3rd toe (the toe was removed at the place of residence due to its gangrene), incipient gangrene of the 1st and 2nd toes of the right foot.
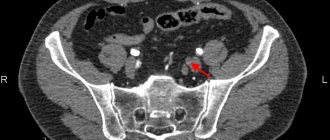
The angiogram shows occlusion of one of the tibial arteries at the level of the right ankle joint, its subocclusion in the lower third of the leg; the blood supply to the foot is provided by a single artery (Fig. 5).
rice. 5 (before intervention) Fig. 6 fig. 7
rice. 8 fig. 9
Balloon angioplasty of the arteries on the leg and foot was performed (Fig. 6, 7, 8, 9).
The main blood supply to the foot has been completely restored (Fig. 10 - angiogram of the right foot and lower third of the leg). Good conditions have been created for the healing of fingers and trophic ulcers. See photos of the foot before, one month, 3 months after angioplasty (the initially long-term non-healing bed after removal of the gangrenous toe quickly healed after angioplasty; the incipient gangrene of the 1st and 2nd toes was stopped - the toes were completely healed).
rice. 10
Photo of the foot before angioplasty Photo of the foot 1 month after angioplasty
Photo of the foot 3 months after angioplasty
Clinical case No. 3
The patient was admitted with critical ischemia of the only left lower limb due to acute thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marbled in color). In 2010 he had already been admitted with a similar condition of the right lower limb, when, despite the full scope of treatment, including a thrombectomy (removal of blood clots) performed by a vascular surgeon called from the republican hospital, gangrene of the limb eventually began to develop, and it had to be amputated.
In the present situation, clinical thrombosis of the arteries of the limb occurred 2 weeks ago, but the patient presented only 2 weeks later as a result of progressive deterioration of the limb.
The angiogram shows thrombotic occlusion of the arteries of the limb below the level of the inguinal fold (Fig. - top row). The patient underwent selective thrombolysis (administration of a drug that dissolves blood clots) through a catheter inserted under local anesthesia through radial access (wrist puncture) and lowered into the left lower limb to the level of thrombosis. The thrombolytic drug was administered for 1 day. Despite the 2-week period of thrombosis, the blood clots were completely dissolved, and the main blood supply to the limb was completely restored (Fig. - bottom row). The patient's complaints completely resolved. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 4
Similar example. The patient was admitted with critical ischemia of the left lower limb due to thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marble-colored).
Clinically, thrombosis of the arteries of the limb also occurred 2 weeks ago, but the patient came only 2 weeks later as a result of a progressive deterioration in the condition of the limb.
The angiogram shows occlusion of the arteries of the limb below the level of the knee joint ( Fig. - top row ). Over the course of 1 day, the patient underwent selective thrombolysis (administration of a drug that dissolves blood clots) through a catheter inserted under local anesthesia through an access on the wrist and lowered into the left lower limb to the level of thrombosis. This method of treatment made it possible to completely dissolve blood clots, despite the 2-week period of thrombosis, the main blood supply to the limb was completely restored ( Fig. - bottom row ). As a result, the patient's complaints resolved completely. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 5
The patient was admitted with critical ischemia of the right lower limb due to thrombosis of the main arteries of the limb (incessant pain in the leg at rest, the leg below the inguinal fold is cold, marbled in color).
In the present situation, clinical thrombosis of the arteries of the limb occurred 3 days ago, but the patient came only 3 days later as a result of a progressive deterioration in the condition of the limb.
The angiogram shows a short occlusion of the femoral artery above the level of the knee joint, occlusion of all arteries of the limb below the level of the knee joint ( Fig. - top row of photos ). The patient underwent selective thrombolysis through a catheter inserted under local anesthesia through radial access and reduced to the level of thrombosis in the right lower limb. The thrombolytic drug was administered for 1 day. Despite the 3-day period of thrombosis, the blood clots were dissolved, the main blood supply to the limb was restored, with the exception of the local area below the knee ( Fig. - second row of photos ). Balloon angioplasty of this area was performed, after which the main blood supply to the limb was completely restored (Fig. - third row of photos) . The patient’s complaints completely resolved. Thus, it was possible to save the limb from amputation, and the patient was discharged in satisfactory condition. Photo below: top row - before the intervention, bottom row - the result of treatment.
Clinical case No. 6
A patient complains of intermittent claudication, pain when walking, mainly in the muscles of the right leg below the knee at a walking distance of 100 m. The angiogram shows a short occlusion of the right femoral artery at the level above the knee joint. Balloon angioplasty of the occlusion area was performed with good angiographic and clinical results. The pain-free walking distance increased significantly. Photo below: the progress of the surgical intervention (before angioplasty - the moment of balloon inflation - the result of balloon angioplasty).
Clinical case No. 7
A patient complains of intermittent claudication, pain when walking, mainly in the muscles of the right leg below the knee, and a progressive decrease in the pain-free walking distance. In the past, the patient underwent femoral-popliteal bypass surgery using his own vein. The angiogram shows critical stenosis of the shunt at the level above the knee joint. Balloon angioplasty of the area of critical stenosis was performed with a good angiographic and clinical result. The pain-free walking distance increased significantly. Photo below: the progress of the surgical intervention (before angioplasty - the moment of balloon inflation - the result of balloon angioplasty). Angioplasty in this situation extended the life of the venous shunt and made it possible to avoid repeated open vascular surgery.
Clinical case No. 8
A patient complains of pain in the muscles of the right leg below the knee. The angiogram shows chronic occlusion (blockage) of the popliteal artery. Recanalization and balloon angioplasty of the occlusion area were performed. However, the result of angioplasty was regarded as insufficient and the intervention was supplemented with stenting with good angiographic and clinical results. The rest pain disappeared. Also, after the intervention there was no intermittent claudication. Photo below: the progress of the surgical intervention (the first row of photos is the area of occlusion before and after angioplasty, the flexion test shows the absence of compression of the stent when bending the knee joint; the following photos show blood flow below the knee joint before and after intervention).
Endovascular treatment of obliterating atherosclerosis. conclusions
Steady progress in manufacturing technologies for endovascular instruments, the emergence of new devices, improvement of catheterization techniques and the emergence of new treatment methods in recent years have led to a significant expansion of indications for endovascular reconstructive operations on the arteries of the lower extremities, improved treatment results and reduced the number of complications and relapses.
The experience accumulated by specialists allows us to recommend endovascular methods for the treatment of obliterating atherosclerosis to everyone who is faced with the problem of choosing a method of treating this disease.
You can ask questions related to angiographic and X-ray endovascular interventions at Medservice LLC:
Tel.
Email mail
Ivanov Andrey Gennadievich (head of the department of x-ray surgical methods of diagnosis and treatment, doctor of the highest category in the specialty “endovascular diagnostics and treatment”)
Indications for angioplasty
Atherosclerosis of the lower extremities often develops in old age due to diabetes, obesity, smoking or poor nutrition. At stages 3 and 4, diabetic foot and dry gangrene often develop due to reduced blood flow. The situation requires urgent care, surgery or even amputation.
Main indications for endovascular surgery:
- narrowing of the vascular bed (stenosis);
- severe swelling;
- anemic condition;
- atherosclerotic lesion of the iliac artery;
- leg cramps;
- trophic ulcers.
Indication for stent installation is a narrowing of the lumen by 75%, a high risk of amputation of the foot due to gangrene. After this procedure, in 95% of cases, the healing of trophic ulcers is accelerated, the blood supply to the muscles is normalized, and tension pain disappears.
Possible complications
Complications after balloon angioplasty of the vessels of the lower extremities usually develop during the intervention and should be immediately eliminated. Methods for eliminating these complications are available to vascular surgeons. The most commonly observed complications are:
- Bleeding from the access site (hematoma or pseudoaneurysm) most often occurs when the patient violates bed rest. Sometimes requires open access to eliminate the source of bleeding.
- Puncture site infection is a very rare complication. It can develop with severe purulent-destructive processes on the lower limb. It is necessary to treat with antibiotics. If necessary, open the purulent focus.
- Contrast kidney injury is a rare complication from contrast media.
- Dissection (dissection) of the artery - sometimes observed with complex lesions and attempts at subintimal passage. Most often it can be eliminated by installing a stent.
- Blockage of the arterial bed with pieces of plaque can be determined during control angiography.
- Fracture of the stent in the places where it bends is a late complication associated with mechanical stress on the metal.
- Repeated narrowing at the site of stent installation (restenosis) is the process of overgrowth of the lumen of the stented segment.
- Arterial rupture is a complication that develops due to excessive balloon inflation in a severely calcified vessel. Detected during control angiography. It is often possible to stabilize the situation with prolonged exposure of the balloon; installation of a stent graft or open surgery may be required.
- Arterial spasm is a reaction to inflating a vessel with a balloon. Occurs in 10% of procedures. To eliminate spasms, medications (papaverine, nitroglycerin) can be administered.
The frequency of all complications is no more than 5% of all procedures performed and they are usually eliminated in a timely manner during the intervention.
Method of operation
The official name of the method is percutaneous transluminal balloon angioplasty, or stenting. During the operation, a special device with a miniature balloon is inserted into a vessel affected by atherosclerosis through a thin catheter. Under pressure, air enters it, the stent expands, increasing the lumen.
After inflating the balloon, the surgeon carefully removes the catheter, leaving the stent securely in place in the artery. The procedure does not remove atherosclerotic plaques in the vessels, but reduces the risk of new deposits in the operated areas. The speed and volume of blood flow increases, nutrition of soft tissues, bones, and leg joints is restored.
Stenting of the lower extremities is carried out in a minimally invasive way: the surgeon makes punctures on the skin no more than 1 cm in diameter in the groin area. The catheter easily passes through the iliac artery through the thigh to the lower leg. At the same time, using diagnostic equipment, the patient’s condition and the location of the stent are monitored.
The operation is performed under local anesthesia, which is important for older people. The patient does not experience pain or discomfort and recovers quickly after the end of stenting.
Main types of angioplasty
Depending on the symptoms and degree of damage to the large arteries, an effective and safe surgical method for humans is selected:
- Transluminal angioplasty - a special balloon is used that is inflated, preventing stenosis. It compresses the plaques on the walls, but after removal there remains a risk of relapse.
- Stenting – a metal structure in the form of a spring creates a strong frame and prevents the artery from decreasing in diameter. After removing the balloon, the stent remains fixed and blocks the accumulation of atherosclerotic plaques. The shape and size of the device are selected individually.
- Laser angioplasty is the newest method in which a quartz thread is inserted into the vessel. Laser beams act on the skin through the skin and increase the temperature, melting cholesterol deposits.
For atherosclerosis of the lower extremities, stenting is most effective. During physical activity, the device supports blood vessels from the inside, controls stretching, blood pressure, and removes swelling in the ankles and cramps in the legs.
Types of angioplastic stenting of the lower extremities:
- Reconstruction of an artery in case of complete blockage by atherosclerotic plaques, installation of an artificial vessel. It starts the blood flow bypassing the affected area.
- An operation to strengthen the stretched artery wall. The stent forms a mesh that restores firmness and elasticity, prevents stenosis, spasms, and thrombosis.
- Standard balloon angioplasty of the iliac artery.
- Administration of drugs simultaneously with the stent for the treatment of atherosclerosis, inflammation, systemic lupus.
When choosing a method, the patient’s age, the presence of contraindications, and general health are taken into account.
Cause of illness
The cause of the disease is the formation of atherosclerotic plaques on the inner wall of the arteries and the gradual layering of salts, cholesterol, fibrin and small blood clots on them. This leads first to a narrowing of the vascular lumen, and then to complete blockage of the artery. The development of the disease can lead to:
- smoking;
- errors in nutrition;
- passion for alcohol;
- overweight, obesity;
- some endocrine disorders - diabetes mellitus, hypothyroidism;
- hereditary predisposition to hyperlipidemia (increased levels of low-density lipoproteins);
- hypertonic disease;
- constant stress and psycho-emotional overload;
- middle and old age;
- insufficient physical activity.
Obliterating atherosclerosis is a serious pathology that needs to be treated, as it can significantly reduce the quality of life. Men suffer from it more often, however, timely consultation with a doctor and correct diagnosis will help maintain health and avoid severe consequences of the disease, such as amputation or death.
Main advantages and disadvantages of stenting
Surgery has many indications and is recommended for patients with allergies to anesthesia.
Unlike a standard operation, the advantages of a closed procedure are:
- average duration – from 40 minutes to 3 hours;
- rapid restoration of blood flow in the first minutes after installation of the structure;
- prevention of thrombosis, myocardial infarction, cerebral or pulmonary stroke;
- blood loss is excluded, there are no incisions, scars, scars;
- short rehabilitation period (after 4 days the patient is sent for home treatment);
- postoperative complications develop only in 4−7% of cases;
- possibility of treating patients up to 75 years of age with minimal risk.
Stenting is a gentle method that allows you to avoid surgery under general anesthesia, amputation and distal prosthetics for diabetic feet.
Among the contraindications to angioplasty:
- acute pulmonary failure;
- endocarditis;
- exacerbation of chronic joint diseases;
- liver failure;
- hemocoagulation disorder;
- hypertensive crisis;
- severe infections of the genitourinary tract and respiratory organs.
The procedure is not recommended if you are intolerant to the components of the contrast agent, which is administered to monitor the movement of the catheter. During stent installation, computed tomography is used, so the operation is not performed during pregnancy at any stage.
Cost of surgeon's services
The prices indicated in the price list may differ from the actual prices. Please check the current cost by calling +7 495 104 8605 (24 hours a day) or at the GMS Hospital clinic at the address: Moscow, st. Kalanchevskaya, 45.
| Name | Price |
| Brief consultation with a leading surgeon/traumatologist/orthopedist | RUB 4,641 |
| Brief consultation with a surgeon/traumatologist/orthopedist | RUB 3,248 |
| Initial consultation with a leading surgeon/traumatologist/orthopedist | RUB 9,566 |
| Initial appointment with a surgeon/traumatologist/orthopedist | RUR 6,696 |
| Repeated consultation with leading surgeon/traumatologist/orthopedist | RUB 8,131 |
| Repeated appointment with a surgeon/traumatologist/orthopedist | RUB 5,691 |
| Extended consultation with a leading surgeon/traumatologist/orthopedist | RUB 17,224 |
Dear Clients! Each case is individual and the final cost of your treatment can only be found out after an in-person visit to a GMS Hospital doctor. Prices for the most popular services are indicated with a 30% discount, which is valid when paying in cash or by credit card. You can be served under a VHI policy, pay separately for each visit, sign an agreement for an annual medical program, or make a deposit and receive services at a discount. On weekends and holidays, the clinic reserves the right to charge additional payments according to the current price list. Services are provided on the basis of a concluded contract.
Plastic cards MasterCard, VISA, Maestro, MIR are accepted for payment. Contactless payment with Apple Pay, Google Pay and Android Pay cards is also available.
Fast healing and short rehabilitation period
The highest level of personnel qualifications
100% sterile
Modern medical equipment and advanced diagnostic and treatment methods
Make an appointment We will be happy to answer any questions Coordinator Oksana
Preparing for surgery
Before stenting the lower extremities, the doctor must properly prepare the patient.
The following diagnostic procedures are preliminarily prescribed:
- determination of blood clotting using a coagulogram;
- clinical blood test;
- X-ray scanning of the vessels of the legs with the introduction of a contrast agent;
- electrocardiogram;
- Ultrasound of blood vessels, liver;
- duplex ultrasound scanning to assess the condition of the arteries.
For chronic diseases, it is recommended to additionally visit your doctor and adjust the dose of daily medications. If you are prone to allergies, the anesthesiologist may prescribe a contrast test.
How is the operation performed?
Patients are rarely hospitalized first: diagnosis can be done on an outpatient basis. Before the procedure, local anesthesia is administered, the patient is positioned on the operating table, and changes into a disposable gown. At the same time, the X-ray equipment is set up.
The contrast agent is administered intravenously in small doses during surgery. An incision is made with a scalpel on the inner thigh or groin to provide access to the iliac vein. A small-diameter catheter with a metal stent is slowly passed through the vessel to the blocked area.
When operating on the arteries of the lower extremities, a coronary stent system from is often used. The cobalt alloy design features an innovative RESOLUTE INTEGRITY zotarolimus coating made from a biocompatible polymer.
Its advantages:
- high degree of flexibility;
- the polymer is released within 6 months, protects the vessel from inflammation and infection;
- tight fit to the walls;
- safety in diabetes.
There is a miniature balloon inside the stent. After insertion and inflation for several minutes, the doctor monitors blood pressure readings to ensure improved blood flow.
After removing the catheters, the puncture is gently clamped for 15-20 minutes, which accelerates blood clotting. The patient is transferred to a regular ward under the supervision of a doctor.
A few words about stents
When performing coronary angioplasty, the following are used:
- Simple metal (without drug coating) stents;
- Drug-eluting stents are stents coated with a special polymer on the stent wall in contact with the vessel and releasing a dosed drug that prevents the development of restenosis;
- Bioabsorbable (self-absorbable) stents - when installed, they expand the lumen of the artery, and within three months they release a drug that prevents the process of restenosis. And after two years, bioabsorbable stents dissolve.
Each type of stent is selected individually, according to indications, taking into account the wishes of the patient and in accordance with all the features of the course of the disease.
Recovery after angioplasty
If there are no contraindications, the patient is recommended to get up the next day, perform simple exercises, and take a few steps around the room. He is given vasodilators and painkillers that dissolve atherosclerotic plaques in the vessels.
Rehabilitation at home helps reduce the risk of relapse:
- daily performance of a complex of physical therapy;
- method of dosed walking “health path” for training the blood vessels of the legs;
- taking medications to control blood pressure, blood sugar and cholesterol levels.
Proper and nutritious nutrition plays an important role. During recovery, it is recommended to completely avoid salty and fried foods and animal fats. The basis of the menu should be products enriched with microelements, potassium, magnesium, vitamins A and E for the elasticity of blood vessels.
Results after angioplasty
Restoring the iliac artery without anesthesia is guaranteed to relieve leg cramps and pain for 5-10 years. The patency of the blood vessel is maintained at 80−85%, which allows you to lead an active lifestyle and reduces the risk of dangerous complications for the body.
To prevent relapse, you need to visit a vascular surgeon annually, having previously undergone the following procedures:
- ultrasound examination of the arteries and veins of the lower extremities;
- tomography using a contrast agent.
Angioplasty of the lower limb artery is the only way to preserve blood circulation in the foot, prevent gangrene and the development of trophic ulcers. Installing a stent using a gentle method in combination with diet and physical activity gives a long-lasting effect and returns the ability to move without pain and restrictions.