Celiac trunk compression syndrome (CTCS) is a rare disease that is one of the causes of chronic abdominal ischemia [1]. Compression of the celiac trunk by the median arcuate ligament of the diaphragm occurs during ontogenesis. In 1965, the American physician J. Dunbar first described this syndrome, which later became known after him [2]. Diagnosis and treatment of SCS are a difficult task for the surgeon, since the presence of extravasal compression detected by instrumental examination methods often does not correspond to the clinical picture and patient complaints. The reasons why in some patients the blood circulation in the celiac trunk is completely compensated by collateral blood flow, while in others ischemia develops, are not fully understood [3]. The clinical definition of SCS can be formulated as follows: extravasal compression of the celiac trunk, confirmed by instrumental research methods, accompanied by clinical symptoms of abdominal ischemia, which cannot be associated with any other disease. The symptoms of this disease are varied: chronic abdominal pain, which occurs or intensifies after eating, can be accompanied by dyspeptic symptoms, neurovegetative disorders, and depressive asthenic-hypochondriacal syndrome.
For many years, the method of choice for SCS was dissection of the median arcuate ligament of the diaphragm using superomedian laparotomy or even thoracophrenolumbotomy, which was accompanied by a severe postoperative period with a large number of complications associated with access trauma [4]. With the beginning of the era of endoscopic surgery, the first reports of laparoscopic decompression of the celiac trunk began to appear [5].
However, since the introduction of this method into surgical practice, questions remain open to this day about indications and contraindications for this operation, surgical technique, intraoperative assessment of the effectiveness of decompression, as well as assessment of treatment results in the early and late postoperative periods.
The purpose of our study is to improve the surgical technique and evaluate the value of intraoperative laparoscopic ultrasound (US), as well as to evaluate and search for ways to improve the immediate and long-term results of laparoscopic decompression of the celiac trunk based on our own experience.
Briefly about the treatment method
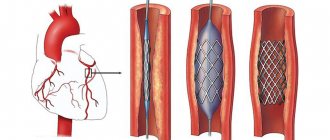
Angioplasty and stenting of the celiac trunk and mesenteric arteries is used to treat the syndrome of chronic intestinal circulatory disorder (angina abdomenalis) or for emergency surgery for acute intestinal circulatory disorder (mesenteric thrombosis).
Intestinal circulatory disorders are rarely diagnosed without a specific focus on certain complaints and are often diagnosed by an experienced clinician only after excluding other causes of abdominal pain.
Previously, when identifying narrowing of the celiac trunk or mesenteric arteries, surgeons adhered to a conservative wait-and-see approach, since open operations on these arteries are very complex and difficult for patients to tolerate. Now, thanks to the development of endovascular technologies, it has become possible to eliminate problems with visceral arteries in a low-traumatic manner.
Why do stenting of the celiac trunk and mesenteric artery?
Inside the abdominal cavity there are organs that are responsible for digestive processes.
They are abundantly supplied with blood by large vessels - the celiac trunk, the superior and inferior mesenteric and renal arteries. Impaired blood flow in these arteries complicates the work of internal organs and impairs their functionality. This disorder can occur suddenly, for example, when a vessel is blocked by a blood clot, or develop in a chronic form, when the flow of blood to the organ is maintained, but noticeably decreases. Acute circulatory disorders require immediate surgical intervention, as they can be fatal. Chronic forms worsen a person’s quality of life, cause other diseases of internal organs, and also require surgery.
Advantages of treatment at the ISC
In case of pathology of the celiac trunk and superior mesenteric artery, our x-ray surgeons can perform angioplasty and stenting of narrowings of these significant arteries. The most commonly used approach is the brachial or radial artery.
In the presence of thrombosis of the mesenteric artery or celiac trunk, our clinic performs thrombectomy operations using a special Rotarex probe or selective thrombolysis. Once blood flow is restored, we perform angioplasty and stenting.
results
The average duration of the operation was 102±20 minutes. Intraoperative blood loss in each case did not exceed 50 ml. Technical feasibility was achieved in all cases, regardless of the option of access to the celiac trunk. There were no conversions, intraoperative complications, or complications in the early postoperative period in any of the 21 cases. The duration of hospital stay was 5.8±0.6 days.
Long-term results from 1 year to 12 years after surgery were monitored in 17 out of 21 patients. According to duplex ultrasound scanning, the average degree of narrowing of the celiac trunk before surgery was 72.5%, in the early postoperative period it decreased to 42.5%, and in the long-term period it decreased further to 33% (Fig. 5).
Rice. 5. The degree of narrowing of the celiac trunk according to ultrasound data before surgery and in the postoperative period.
The change in hemodynamic parameters of blood flow velocity in the celiac trunk after surgery also seems significant. Thus, before the operation, the average peak systolic blood flow velocity in the celiac trunk (Vs) was 312 cm/s, and the acceleration of the peak systolic blood flow velocity in the deep exhalation phase compared to the deep inspiration phase (Vs exhalation - Vs inhalation) was 144.5 cm/s. With. In the early postoperative period, these indicators decreased to 193.3 cm/s and 54 cm/s, respectively. In the long-term postoperative period, the peak systolic blood flow velocity in the celiac trunk (Vs) was 172 cm/s, and the acceleration of the peak systolic blood flow velocity (Vs ext - Vs inhalation) decreased further to 43.5 cm/s (Fig. 6).
Rice. 6. Hemodynamic parameters of blood flow before and after surgery.
In our study, intraoperative laparoscopic ultrasound was performed in all cases of celiac trunk decompression, which allowed, in addition to determining the anatomy of the celiac trunk, to objectively assess the adequacy of decompression and, accordingly, obtain good clinical results (Fig. 7).
Rice. 7. Intraoperative ultrasound scanning allows assessing the effectiveness of decompression.
However, 2 out of 21 patients required repeat surgery. In the first case, repeated surgery was required due to incomplete restoration of blood flow along the celiac trunk after laparoscopic decompression. The operation was performed through an open approach a year after laparoscopic decompression, with a positive effect. This case was the first experience of performing laparoscopic decompression of the celiac trunk at the Institute of Surgery named after. A.V. Vishnevsky. Thus, the need for reoperation may be associated with inadequate decompression during the development of the technique.
In the second observation, laparoscopic decompression of the celiac trunk was performed with a pronounced positive effect, which was confirmed by ultrasound data in the early and late postoperative periods. Due to the persistence of the patient's complaints and the presence of instrumentally confirmed hemodynamically significant compression of the celiac trunk, a decision was made to repeat laparoscopic decompression. Repeated laparoscopic decompression was performed successfully, blood flow was completely restored: according to ultrasound examination in the early postoperative period, blood flow in the celiac trunk was laminar in nature, the linear speed of blood flow was 180 cm/s. However, the patient continued to complain of abdominal pain. In this case, we are probably talking about a psychosomatic disorder.
We consider the main criteria for the effectiveness of surgical intervention to be postoperative improvement in hemodynamic parameters of blood flow in the celiac trunk (these parameters go out of the range of hemodynamic significance) in combination with relief of symptoms and improvement in the patient’s quality of life.
The effectiveness of the performed intervention in the long-term postoperative period was assessed clinically, according to postoperative instrumental examination, as well as using a questionnaire using the SF-36 quality of life assessment system. According to the SF-36 questionnaire, 17 out of 21 patients were surveyed twice: in the preoperative period and one year after the intervention. Before the operation, the average value of the physical component of health was 38 points, psychological - 31 points, pain intensity was 28.7 points. In the postoperative period, the studied criteria were assessed with a large number of points, which indicated an increase in the quality of life and a decrease in pain intensity: the physical component of health was 41.5 points, the psychological component was 35.8 points, the pain intensity criterion was 40.2 points (Fig. 8 ).
Rice. 8. Assessment of quality of life according to the SF-36 questionnaire.
Indications and contraindications for the treatment method
Indications:
Celiac stenosis more than 60% with chronic abdominal ischemia syndrome
Stenosis of the superior mesenteric artery more than 60% (symptoms of intestinal vascular insufficiency are not a mandatory indication, the fact of stenosis is sufficient)
Stage of endovascular treatment of acute mesenteric obstruction (mesenteric thrombosis)
Contraindications:
- Allergy to iodine
- Thoracoabdominal aortic aneurysm (without aneurysm surgery)
- Stage of intestinal necrosis with mesenteric thrombosis
Diagnostics
Mesenteric thrombosis: causes, symptoms, treatment
Diagnosis should be based on physical and instrumental examination methods. During the examination, it is necessary to measure the pulse. Cardiac stenosis will be characterized by its slow speed and low value.
https://youtube.com/watch?v=BbfNG4gqp_s
https://youtube.com/watch?v=BbfNG4gqp_s
Physical methods include auscultation and palpation. An auscultatory sign of this disease is listening to a systolic murmur; you need to listen above the aortic arch and mitral valve; there is a decrease in two tones. Palpation is an important clinical technique. There is a change in the localization of the apical impulse and its systolic tremor. Percussion shows a displacement of the left cardiac artery to the left and down.
Patients with this pathology have a pale skin color, often a bluish color of the limbs of the body. Often the abdomen will be swollen, as will the lower extremities.
Instrumental examination methods include:
- echocardiography (EchoCG);
- electrocardiogram (ECG);
- ultrasound examination (ultrasound);
- X-ray examination;
- cardiac catheterization.
An electrocardiogram reveals the degree of left ventricular hypertrophy and a shift of the heart axis to the left. An X-ray examination shows expansion of the heart. A diagnosis of arterial pulmonary hypertension is made. Echocardiography examines a fibrous valve-subvalvular formation, which is thickened, a hypertrophied cardiac septum.
Preparing for treatment
Standard examination before surgery:
- Clinical blood and urine tests, biochemical blood test.
- Coagulogram, platelet aggregation
- Gastroscopy (examination of the stomach)
- X-ray of the lungs
- ECG
- ECHO cardiography
- Ultrasound of the abdominal organs, aorta and arteries of the extremities
- Multislice computed tomography with contrast of the aorta and its branches
Before surgery, you must abstain from eating for 8 hours and liquids for 2 hours. No other preparation activities are required.
How the treatment method works
The operation is performed under local anesthesia in the access area. Perhaps access will be on the thigh or in the elbow area. The surgical field is treated with an antiseptic and covered with sterile sheets.
The surgeon performs local anesthesia at the puncture site, after which the artery is punctured with a special needle and a short tube is installed - an introducer.
All further work with the vessels is carried out through the introducer. A special guide is inserted into the abdominal aorta, then a catheter is passed through it, through which a contrast study of the celiac trunk and mesenteric artery is performed. This stage is called selective angiography. It is the definitive diagnostic method. If narrowing of the arteries is confirmed, then the guidewire is inserted below the narrowing site. A balloon with a stent is passed through the guidewire. By expanding this balloon, the narrowing of the artery is eliminated, and the stent strengthens the arterial wall.
After stent implantation, control angiography is required to exclude possible complications. The catheter and introducer are removed from the access site, and bleeding is stopped by pressing or using a special Angiosil suturing device.
| To main |
(Radiation diagnostic news 2000 1: 8-11)
Chronic disorders of visceral circulation.
Filippovich N. S.
Belarusian Institute for Advanced Medical Studies.
Chronic disorders of visceral circulation are a disease characterized by ischemic circulatory disorders of the abdominal organs, caused by impaired patency of the visceral arteries due to extra- or intravasal causes (A. V. Pokrovsky, 1979). Since the disease manifests itself as an attack of abdominal pain at the moment of greatest functional activity of the digestive organs, some authors use the term “angina abdominalis” to refer to this disease. The mechanism of origin of pain is identical to angina pectoris and is associated with a lack of oxygenated blood flow to an actively functioning organ due to impaired blood flow through the arteries.
The history of studying the pathology of visceral arteries began in 1843, when Tiedeman at autopsy revealed asymptomatic occlusion of the superior mesenteric artery. The frequency of the disease has not yet been determined. According to pathological studies, damage to the celiac arteries is observed in 20-45% of cases, the superior mesenteric artery in an average of 30% (Dewgan C., et. al).
There are acute and chronic forms of ischemic intestinal disease. Acute IBD is a special chapter of emergency surgery. The number of patients with CIBC is progressively increasing as the disease is studied, and the true number of people with this pathology is much greater than is detected in clinical practice. This is explained by the variety of clinical manifestations, the complexity of diagnosis, and ignorance of some features. Considering that people of working age suffer from this disease, the need to study the issues of diagnosis and treatment of abdominal clinical syndrome and the enormous social significance of the problem becomes clear.
In the general hemocirculation system, mesenteric blood flow plays a significant role. The amount of blood in the intestines of an adult is from 30 to 40% of all circulating blood; blood circulation in the intestines is provided by the vessels of the superior and inferior mesenteric arteries and veins, and the celiac artery.
The main causes of chronic disorders of visceral circulation are intravascular stenosis and occlusion and extravascular compression of the visceral arteries. In first place among intravascular factors is atherosclerotic damage to the visceral arteries, in second place is aortoarteritis.
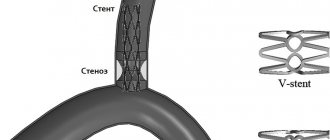
Extravasal factors causing compression of the mesenteric arteries: the falciform ligament of the diaphragm, its medial leg, solar plexus ganglia, tumors, etc. In this case, the celiac trunk is most often subjected to extravasal compression.
Sometimes compression occurs with a high origin of the celiac trunk from the aorta, in other cases with a low attachment of the diaphragm with a normal level of origin of the artery. In addition, kinking of the celiac artery can occur as a result of its low origin from the aorta.
Pathological anatomy.
The main visceral arteries form a wide network of collateral vessels. The following collateral connections are of most clinical importance. Between the celiac and superior mesenteric arteries there are anastomoses formed by the supraduodenal and retroduodenal arteries from the celiac artery collector and the anterior and posterior branches of the inferior pancreatoduodenal artery - branches of the superior mesenteric artery. In the area of the head of the pancreas, these branches form the so-called anterior and posterior pancreaticoduodenal arcades - or minor arch. The superior and inferior mesenteric arteries are connected to each other by a wide arterial bridge - a large arch - the arch of Riolan, formed by the middle colic and left colic arteries. The inferior colic artery in turn is connected to the internal pudendal artery ( Fig. 1
)
In addition to the listed anastomoses, there is a wide network of small collaterals. Vascular anastomoses become extremely important when the patency of the main visceral arterial trunks is impaired. They provide functionally complete collateral blood flow, which can protect part of an organ or the entire organ from ischemic damage. These usually small-caliber arterial anastomoses, in conditions of obstruction of the main arteries, turn into powerful collateral pathways. In case of stenosis or occlusion of the celiac artery, the most important collateral blood flow occurs through the pancreaticoduodenal arcades. The blood flow begins from the pancreaticoduodenal arteries emerging from the superior mesenteric artery, which connect through the posterior or anterior pancreaticoduodenal arcade to the gastroduodenal artery, and then through the common hepatic artery to the celiac artery.
With partial or complete occlusion of the superior mesenteric artery, the same collateral circle functions, only in the opposite direction, and at the same time the Riolan arch is activated.
However, often the collateral blood flow does not develop sufficiently and many factors - age, the nature of the pathological process, anatomical variations, etc. can influence the adaptive capabilities in conditions of ischemia, therefore, a pronounced clinical picture is often observed even with an isolated lesion of one of the visceral branches.
When analyzing the causes of disturbances in visceral blood flow, the following pattern is observed: the cause of isolated damage to the celiac artery is most often extravasal compression, the superior mesenteric artery is somewhat more often affected in nonspecific aortoarteritis. The inferior mesenteric usually suffers from atherosclerosis.
Pathogenesis
The disease is characterized by a variety of functional and morphological disorders, complex hemodynamic and neuro-reflex relationships.
In the initial stages of the disease, the restriction of blood flow to the organs of the digestive tract is compensated with the help of systemic collaterals. Subsequently, under the influence of chronic ischemia, dystrophic changes in the glandular apparatus, degenerative processes in the functional elements of the digestive organs and their replacement with less differentiated connective tissue occur. Absorption disorders in the intestine of ischemic origin are characterized by insufficient digestion of all components of food products, especially fat. Long-term chronic ischemia of the muscular layer of the intestinal wall leads to impaired peristalsis. Arterial insufficiency and hypoxia of the intestinal wall leads to weakened peristalsis, which is clinically expressed by flatulence and constipation. The disease is defined by a triad of symptoms: 1) paroxysmal abdominal pain that develops after eating at the height of digestion; 2) intestinal dysfunction; 3) progressive weight loss. In 78% of patients with celiac trunk stenosis, a systolic murmur is heard in the epigastric region; in cases of damage to the superior mesenteric artery, it is heard in 50%. For these symptoms to occur, two of the three main visceral arteries must be more than 50% stenotic.
If all of the above symptom complex is present, as well as if there is a systolic murmur and negative results of studies of the cardiovascular system and gastrointestinal tract, and there is no effect of treatment, the patient must undergo an X-ray contrast study of the visceral vessels.
Diagnostic measures
include general clinical and special. From general clinical findings, attention should be paid to a thorough collection of anamnesis, complaints, indication of the patient for unsuccessful conservative treatment, identification of the characteristic systolic murmur heard above the mouths of narrowed visceral arteries. Using laboratory research methods, it is possible to identify dysfunction of the digestive system (scatological examination reveals undigested muscle fibers, neutral fat, and a large amount of fiber).
The presence of leading signs of CIBD is a direct indication for X-ray contrast angiography of the abdominal aorta and its visceral branches. The following methods are used: 1. Abdominal aortography in the sagittal and frontal planes, 2. Selective angiography of the visceral arteries.
X-ray (angiographic) signs are divided into two groups: direct and indirect. Straight lines are deformation, stenosis and occlusion visible directly on the artogram: ( Fig. 2, 3
) shadows of the initial part of the arterial trunk in the form of an hourglass, excessive approach (pressure) of the celiac artery to the superior mesenteric artery and the presence of an acute angle between the celiac artery and the aorta. These signs also include the break or absence of contrasted arteries on the aortogram with their complete occlusion. Direct signs are better identified in the lateral or one of the oblique projections, and can also be clearly identified with selective angiography. Direct angiographic signs allow one to directly determine the location, extent and extent of the lesion, as well as its most likely cause. Thus, atherosclerosis is characterized by localization of the process at the mouths of the visceral arteries, extensive distribution, blurred contours of the affected artery, and simultaneous involvement of the abdominal aorta in the process. With nonspecific aortoarteritis, the aorta and celiac artery are most often affected, then the superior mesenteric artery. In the affected area, the contours of the vessel are clear and circularly narrowed. Extravascular compression of the celiac trunk is characterized by the approach of the celiac trunk to the superior mesenteric artery, the formation of an acute angle between the celiac trunk and the aorta, and the presence of hourglass-shaped deformations of the arteries.
| Rice. 1. Scheme of collateral pathways in abdominal tonsillitis syndrome. | |
| Rice. 2. Stenosis of the celiac trunk. Atherosclerotic lesion. Lateral angiogram. |
Indirect signs include: 1. The presence of clearly defined and expanded collaterals between the celiac trunk and the superior mesenteric artery. 2. Symptom of retrograde contrast of the arterial trunk. ( Fig. 4
) 3. Poststenotic dilatation of the arterial trunk. 4. Absence of retrograde reflux of contrast agent into the aorta during selective catheterization of a stenotic visceral artery.
| Rice. 3. Selective celiacography. Stenosis of the celiac trunk, splenic artery. Poststenotic dilatation of the common hepatic artery. Atherosclerotic lesion. | |
| Rice. 4. Selective upper mesentericography. Retrograde contrasting of the celiac trunk, hepatic arteries through the “lesser arch”. |
The possibility of using duplex Doppler ultrasound (DDG) and color Doppler ultrasound (CDG) for these conditions is currently being studied. Sometimes there are limitations due to gas obstructing the bowel and difficulty in obtaining images of the inferior mesenteric artery; conventional studies rarely make a diagnosis of mesenteric vascular ischemia. Doppler sonography to study local disturbances in the blood flow of the celiac trunk and the SMA is performed on an empty stomach (12 hours without food intake). The disturbances recorded in this case may be the following: changes in the waveform, speed or direction of blood flow, increased turbulence, indicating stenosis. The largest stenoses occur in the proximal segments of the vessels. The normal waveform in the proximal celiac axis is a highly resistant structure with low diastolic flow. More distally, the waveform becomes low-resistance with continuous diastolic flow. The VMA normally has turbulent flow. On an empty stomach, a highly resistant structure with minimal diastolic flow is revealed. Postprandially, a low-resistance pattern is observed with broad systolic peaks, increased systolic and diastolic velocities, and continuous diastolic flow. In the presence of significant stenoses in fasting patients, an increase in the maximum systolic flow velocity through the narrowing zone with significant spectral expansion, post-stenotic turbulence and relatively pronounced diastolic flow is detected. With CDG, a high-velocity flow is visible ( Fig. 5, 6
). Most specialists prefer to repeat the study 45 minutes after patients eat a standard breakfast, since most patients have a normal fasting flow, and provocative tests are necessary to detect pathology. With significant stenosis in patients after eating, changes in the SMA are detected. The flow characteristics in the celiac axis do not change noticeably even in healthy patients.
.
| Rice. 5. Ultrasound image of an atherosclerotic plaque at the mouth of the celiac trunk. TC-celiac trunk, AO-aorta. | |
| Rice. 6. Spectrogram of blood flow recorded in the area of celiac trunk stenosis (turbulent blood flow). |
Recently, CT and MRI have been successfully used to identify changes in the visceral arteries. ( Fig. 7
).
A routine X-ray examination of the gastrointestinal tract may reveal some nonspecific changes, in particular the slow passage of barium in the stomach and intestines, and increased gas content in the intestines. In addition, symptoms of chronic intestinal ischemia are observed in the form of varying sizes of filling defects due to swelling of the mucous membrane, which disappear upon repeated examination; slit-like areas of clearing due to segmental spasms of the ischemic intestine and segmental intestinal stenosis. Haustra disappear in the colon, and emptying slows down.
Differential diagnosis
carried out with a tumor of the stomach, liver, pancreas (with extravasal compression of blood vessels), chronic pancreatitis, peptic ulcer, abdominal aortic aneurysm.
| Rice. 7. CT scan. Atherosclerosis of the abdominal aorta. Calcified plaque at the mouth of the celiac trunk. | |
Possible complications during treatment
Complications of the operation itself:
- Rupture of a narrowed artery with bleeding requires emergency open surgery or installation of a special covered stent (stent graft). Fortunately, it is very rare.
- Thrombosis of the reconstructed artery is a rare complication that occurs with increased blood clotting. If preoperative preparation is carried out using antiplatelet preparation, then the risk is minimal. If thrombosis is observed during the intervention, then thrombectomy or thrombolysis (administration of drugs that resolve the clot) is performed. If signs of intestinal circulatory disorders are observed after surgery, the patient is taken back to the operating room and blood clots are removed using Rotarex or special aspiration catheters.
Complications of vascular access:
- Hematoma in the puncture area
- Arterial thrombosis in the puncture area
- Damage to nerves in the puncture area
These complications are extremely rare and can be easily eliminated if detected early.
Additional information affecting the course and outcome of the disease
Tests used to confirm ischemia in SCS
The most informative is tonometry based on measuring pCO2 of the mucosa.
Intraluminal pCO2 measurements are performed with a nasogastric and nasojejunal catheter connected to a capnograph.
The appearance and increase of the pCO2 gradient occurs when the blood flow decreases below 50% of the initial flow and its subsequent sharp change.
The best diagnosis of CMI is tonometry against the background of functional load or food test:
- sensitivity 76%
- specificity 92%.
Disadvantages of tonometry:
- complexity and high cost of technology,
- discomfort during the examination,
- duration of the study,
- errors in violation of measurement technology,
- Capnographs are not produced or serviced.
Surgery
After operation:
- KSCS symptoms (pain) are relieved in 83-88% of patients when observed for up to 30 days;
- after vascular reconstruction, symptoms regress in almost 100%;
- after 5 years of asymptomatic patients after decompression 69%, after reconstruction 83%;
- after 10 years, asymptomatic after decompression 53%, after reconstruction 76%.
Predictors of poor prognosis:
- atypical pain syndrome with periods of remission,
- history of asthenoneurotic condition,
- mental illness,
- alcohol abuse,
- age over 60 years,
- weight loss of less than 20 pounds (9 kg),
- vomiting and pain that occurs without provoking factors.
Asthenoneurotic or mental deviation:
- in 28% of adults with SCS,
- in 43% of children with SCHS,
- requires mandatory splanchnicganglionectomy,
- extended psychiatric/psychological analysis of patients with SCS before and after surgery.
Observation program after treatment method
The results of angioplasty and stenting of visceral arteries are monitored using ultrasound control after 3 months and then annually.
One year after the intervention, it is advisable to perform multislice computed tomography with contrast of the abdominal aorta and its branches.
After treatment, the patient is prescribed antithrombotic drugs. Most often these are aspirin and clopidogrel (Plavix). These medications must be taken regularly, and doctors must be notified before performing any other interventions.