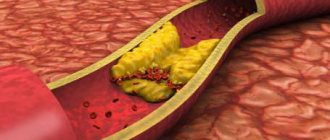
Narrowing of the carotid arteries is observed with atherosclerosis, a systemic process affecting all arteries. The main manifestation of atherosclerosis is the appearance of atherosclerotic plaques on the inner wall of the artery. These plaques are composed of cholesterol, calcium and fibrous tissue. Gradually increasing in volume, plaques narrow the lumen of the arteries and disrupt normal blood flow. When plaques form in the lumen of the carotid arteries, cerebral circulation is disrupted.
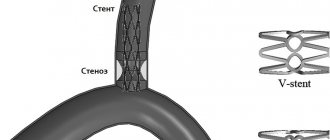
Carotid artery stenting is a procedure that involves installing a thin wire structure in the form of a cylinder into the lumen of a narrowed vessel, which plays the role of a frame - a stent. A stent is usually placed in a previously dilated artery.
The carotid arteries begin from the aortic arch. Around the middle of the neck they are divided into external and internal. The external carotid arteries supply blood to all the soft tissues of the head. The internal carotid arteries supply blood to the brain.
The appearance of plaques on the walls of the internal carotid arteries is fraught with dire consequences. Plaques are sites where blood clots form. This leads to complete blockage of the lumen of the arteries. A so-called ischemic stroke occurs. In addition, thromboembolism may develop. This condition occurs when a small blood clot breaks off from an atherosclerotic plaque, blocking the arteries of the brain. When blockage of small-caliber arteries occurs, a transient ischemic attack develops.
There are several types of surgical treatment for carotid artery disease. And one of them is carotid stenting .
Preparation for carotid artery stenting surgery
Typically, preparation for carotid stenting involves taking aspirin a week before surgery. This is necessary to reduce blood clotting. Before the operation, the doctor conducts diagnostic tests such as duplex ultrasound scanning and computed tomography, and, if necessary, angiography and magnetic resonance angiography are performed. These methods make it possible to determine the location of the atherosclerotic plaque. The speed of blood flow through the vessels of the brain, the diameter of their lumen and other parameters of cerebral circulation.
Currently, carotid stenting surgery is indicated for patients at high risk of complications from endarterectomy. Indications for carotid stenting include significant narrowing (60%) of the lumen of the carotid arteries, symptoms of microstroke and stroke. If you do not have any symptoms, the indications for stenting are significant narrowing (80%) of the lumen of the carotid arteries and a high risk of complications from endarterectomy. In addition, carotid stenting is indicated for patients who have previously undergone endarterectomy in cases of recurrent narrowing of the arterial lumen.
Symptoms of atherosclerosis
The disease may not manifest itself in any way in the early stages. In most patients, the first sign of pathology is a stroke. But atherosclerosis can be recognized by indirect symptoms:
- feeling of weakness, tingling only on one half of the body (right/left);
- inability to control the motor activity of the arm/leg;
- temporary loss of vision in one eye;
- slurred speech.
Symptoms may subside within a few hours, but this is a warning sign. They indicate a high risk of stroke, so you should consult a doctor immediately.
Risk factors for complications of carotid stenting
These factors include:
- High blood pressure;
- Allergy to X-ray contrast agents;
- Calcification (impregnation with lime) and large-scale narrowing of the carotid arteries;
- Sharp bends and other anatomical features leading to difficulties in stent placement;
- Plaques of significant size, or atherosclerosis of the aorta in the area of the beginning of the carotid arteries;
- Age over 80 years;
- Concomitant blockages of the arteries of the vessels of the arms and legs.
Angioplasty and stenting of the carotid arteries
Only a number of completed randomized studies have been published, which directly compared ESA with angioplasty and carotid artery stenting. Nowadays there will be much more evidence for the usefulness of stenting and against this method. The SAPPHIRE study center randomized 334 patients with asymptomatic carotid artery stenosis of either greater than 50% or greater than 80% to the ECA stenting procedure. The primary outcome measures were death, stroke or myocardial infarction within 30 days of the procedure and ipsilateral stroke and death between 31 days and 1 day after the procedure. The primary end point was recorded in 20 patients in the stenting group (cumulative incidence 12.2%) and 32 patients in the endarterectomy group (cumulative incidence 20.1%). There was no statistically significant difference between the two procedures (p = 0.053), but non-inferiority for stenting was equal to endarterectomy. It is important to note that a high incidence of perioperative complications was avoided both for endarterectomy and for stenting in this high-risk cohort. The incidence of stroke and death at 30 days for asymptomatic patients was 10.2% for endarterectomy and 5.4% for stenting (p = 0.20). These results provide information about the benefits that drug therapy may have in this group of patients.
The SPACE study was the first large randomized controlled study to compare endarterectomy versus stenting in symptomatic patients. The incidence of ipsilateral stroke and death at 30 days was similar—6.3% for endarterectomy and 6.8% for stenting.
The results of the EVA-3S follow-up on the 30th day have been published. This study included patients who had recently (within 120 days) hemispheric or retinal transient ischemic attack (TIA) or non-disabling stroke and minor stenosis of symptomatic carotid artery in 60 years. % to 99%. Patients were randomized to endarterectomy (n = 262) or stenting (n = 265). The incidence of stroke and death at 30 days was higher in the stenting group (9.6%) and lower in the endarterectomy group (3.9%). However, the investigation could have been compromised due to a lack of information about the various centers in which the stenting took place. In addition, in 8.1% of the cohort, the stenting procedure was completed without distal embolic closure. The terminal points were less likely to occur in patients in whom stenting was performed with an embolic stent, but equally so in those in whom stenting was performed without a stent.
In people with atherosclerotic lesions of the carotid arteries, a variety of embolic mechanisms have been tested. In typical cases, these structures contain 50 to 70% macroscopic embolic material. Microscopic material that leaks through these devices includes red blood cells, white blood cells, platelets, and fibrous hyperclinite tissue fragments. No clinical significance was identified for this material.
In the United States, we recommend clinical stenosis of the carotid arteries only in patients who have symptomatic carotid artery stenosis of 70% or greater, and only in cases where the clinical evidence does not provide adequate evidence for diagnosis and the sickness of this illness. Stents and embolic protection devices are thoroughly cut, therefore clinical investigations are necessary in order to carry out their straightening.
Carotid stenting procedure
Stenting surgery is usually performed under local anesthesia. Before the operation, the patient is connected to special monitoring equipment that monitors parameters such as blood pressure and heart rate.
During surgery, the surgeon usually talks to the patient and also instructs the patient to periodically squeeze a toy or ball to monitor brain function. Some surgeons perform carotid stenting under general anesthesia.
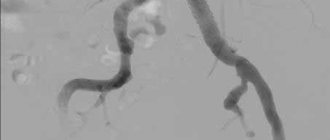
Before surgery, heparin is administered intravenously to reduce blood clotting. The surgical site is numbed with an anesthetic. Before stenting, angiography is performed - an x-ray method that allows you to determine the location of the narrowing of the vessel. After which the stenting procedure begins.
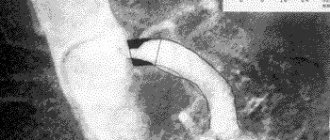
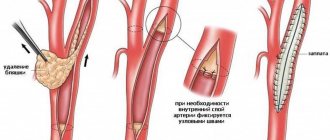
Angioplasty is usually performed before stenting. In this case, a catheter with an inflatable balloon at the end is inserted through the femoral or upper limb artery. The catheter is brought to the site of narrowing of the artery, which is monitored in real time on an X-ray monitor. Next, the balloon is inflated and the lumen of the artery expands. In this case, the patient does not feel pain, since there are no nerve endings on the inner wall of the vessels. At this stage of the operation, the surgeon installs a special balloon, basket or filter behind the narrowing of the artery in order to prevent embolism (blockage) and the development of stroke that occurs as a result of plaques or blood clots breaking off.
After widening the lumen of the artery, a stent is installed using an inflatable balloon. To do this, a compressed stent is inserted into the lumen of the artery using another catheter. Once the stent is at the site previously expanded with the balloon, it relaxes and follows the wall of the artery. To more firmly “implant” the stent into the artery wall, the balloon is inflated again. After this, the catheter-filter device is removed. The stent remains in the lumen of the artery. The entire operation takes on average 1-2 hours, sometimes longer.
Endarterectomy of the carotid arteries
A number of randomized clinical studies of ESA and drug therapy were conducted in parallel with drug therapy itself in patients with symptomatic carotid artery stenosis. More studies - ECST (the European Carotid Surgery Trial), NASCET (the North American Symptomatic Carotid Endarterectomy Trial) and Veterans Administration Cooperative Trial 309 - were the subject of meta-analysis after they concluded the harmonization of the world's stages of stenosis in the carotid arteries. As a result, we managed to accumulate data from 6092 participants and collected 35,000 patients under surveillance in dynamics. Of the 6,092 patients, 601 (10%) were female, over 75 and 1,763 (28%) were female. Carotid endarterectomy increased the risk of ipsilateral ischemic stroke, intraoperative stroke, and operative death in patients with less than 30% stenosis. The procedure is not less costly in patients with stenosis of 30–49%. However, in patients with stenosis of 50–69%, ESA showed a reduction in the 5-point absolute risk of ipsilateral stroke by 4.6% (95% CI, 0.6–8.6%). A more pronounced decrease in the 5-point absolute risk (16%, 95% CI, 11.2–20.8%) was found in patients with stenosis of 70–99%, but not in patients as and Mali Stan, close until occlusion. Patients with a stage close to occlusion did not lose the essential benefits of the ESA, but the number of participants with such a level of stenosis was small, so it is important to change the basic procedure. ESA is small, but there are fewer positive effects in women and less in men.
Asymptomatic stenosis of the carotid artery of moderate to high severity is also a risk factor for ischemic stroke. A cohort study of 1115 patients with asymptomatic carotid artery stenosis found that the risk of stroke increased with the grade of stenosis.
Carotid endarterectomy has proven effective in patients with asymptomatic high-grade carotid artery stenosis. A systematic review of 3 randomized studies involving 5223 patients found that ECA significantly reduced the risk of perioperative stroke and death, as well as subsequent stroke (terminal risk [RR] 0.69). When asymptomatic carotid artery stenosis is detected, ECA has a much greater positive effect in men and young patients.
Postoperative period after carotid artery stenting
Immediately after surgery, the doctor applies pressure to the catheter insertion site for 15-30 minutes to prevent bleeding. After surgery, it is recommended to stay in bed for several hours so that the doctor can monitor the occurrence of complications. It is recommended to limit heavy lifting for a while. After surgery, it is not recommended to take baths (you can shower). The doctor will also advise you to drink plenty of fluids to quickly remove the contrast agent from your body. After carotid stenting surgery, it is recommended to take blood thinners (aspirin). In addition, it is periodically necessary to monitor the condition of the carotid arteries using duplex ultrasound scanning.
Medications
Certain medications may also be used under medical supervision to control chronic diseases and prevent blood clots. Your doctor may prescribe aspirin or other blood thinners to be taken daily. He may also recommend taking medications to maintain normal blood pressure, such as angiotensin converting enzyme (ACE) inhibitors (Enalapril), angiotensin II receptor antagonists (Losartan), or calcium channel blockers (Amlodipine). and/or a drug of a number of statins (Simvastatin (Simvastatin)), which lower blood cholesterol levels.
Complications of carotid stenting
The most serious complication of carotid stenting is embolism (blockage) of blood vessels in the brain, which leads to stroke. Another complication that causes blockage of blood vessels is the formation of a blood clot along the stent. In addition, there is a complication such as restenosis - repeated blockage of the vessel. Another type of complication is associated with the toxic effect of the contrast agent on the kidneys, which is especially pronounced in patients with renal diseases. Less common is a hematoma or false aneurysm in the area where the catheter is inserted.
Diagnosis of important carotid artery stenosis
Traditional angiography is increasingly being used to identify carotid artery stenosis in patients with murmurs over the artery or symptomatic ischemic cerebrovascular disease, but it is not treated invasive methods, which include computer tomographic angiography, magnetic resonance angiography and duplex ultrasonography of the carotid arteries.
When performing angiography of the carotid arteries, physicians can use different techniques to assess the size of the artery diameter stenosis. Therefore, when interpreting a digital display, you need to know how it was indicated.
One-hundred-year-old duplex ultrasonography of the carotid arteries The Fellowship of Radiologists of Northern America proposes, in assessing the importance of carotid artery stenosis, to compare the criterion of peak systolic fluid (PSV) with hemorrhage through the internal the carotid artery is greater than 230 cm/s and the diameter of the artery lumen is approximately 50%. Secondary criteria for the importance of stenosis include a PSS of the internal carotid artery/hilar carotid artery greater than 4.0 and terminal diastolic fluidity (CDS) and bleeding through the internal carotid artery b more than 100 cm/s. Other authors found a 95% positive predictive value for arterial diameter stenosis of 60% or greater when combining the criteria of PSS over 290 cm/s and DFS over 80 cm/s.
When non-invasive investigations are conducted correctly, they produce more accurate results. A systematic review of 63 publications of MRA, carotid ultrasonography, and both methods is consistent with MRA having an overall sensitivity of 95% and an overall specificity of 90% for diagnosing stenosis of 70–99%, consistent with and stenosis less than 70%. For duplex ultrasonography of the carotid arteries, a sensitivity of 86% and a specificity of 87% were obtained. In both situations, angiography with digital processing of information was used as the gold standard. Magnetic resonance angiography has significant discriminatory power when diagnosing stenosis of 70–99%, while ultrasonography and MRA has significant advantages when diagnosing occlusion of the carotid artery.
Currently, the optimal methods for assessing carotid artery stenosis are Doppler ultrasonography and contrast-enhanced MRA.
Screening for asymptomatic carotid artery stenosis
Prophylactic endarterectomy is indicated in patients who have a low risk of surgical complications and high-grade atherosclerotic stenosis of the carotid artery. However, no consensus has been reached on how best to screen these patients. The presence of a murmur over the carotid artery is a poor predictor of severe carotid artery stenosis. For example, in the third of 330 consecutive patients who were admitted to the cerebrovascular clinic, there was a small murmur over the carotid artery, and its positive predictive value was less than 37% for the detection of carotid artery stenosis of the middle artery this is an important step. Patients with multiple risk factors, such as smoking, hypertension, and ICS, have a high likelihood of demonstrating atherosclerotic disease in the carotid arteries even before they undergo a blood level test. Therefore, it is important to carry out screening of the carotid arteries in patients, if there may be evidence of vascular risk factors and noise over the carotid arteries.
Infusion of information and practical tips on clinical research
Most, but not all, publications have shown that the evidence and practical skills of surgeons have a significant impact on the risk of complications after endarterectomy of the carotid arteries. When examining the Canadian administrative data base, it was revealed that if an endarterectomy is performed on a patient by a surgeon who performs few such operations and performs in the hospital, who ends up receiving few such operations, then the risk is the decrease in internal hospital stroke and death increased by 3.5 times, equal with the surgeon, who receives a lot of such deliveries and works at the hospital, where a lot of such operations are carried out. These findings allow the framework to develop assumptions, which is the main connection between the surgeon’s knowledge and low sickness during the final operation, and therefore they must be interpreted carefully, so that the selection of patients can be applied to the results. Results at 30 days from the NASCET (the Asymptomatic Carotid Atherosclerosis Study) and other randomized clinical studies show a lower incidence of sagging at 30 days in asymptomatic younger patients, as and there are few comorbid conditions, equal with symptomatic older patients , like a bunch of comorbid conditions.
How to prepare?
The doctor will study the medical documentation, conduct a medical examination, and give a preliminary assessment of the situation and the cost of stenting. Before angioplasty, the following studies are performed:
- Ultrasonography. An ultrasound probe is placed on the skin in the projection of the carotid artery to obtain an image of the affected area and blood flow in the brain.
- Magnetic resonance imaging (MRI) or CT angiography (with contrast). The studies produce high-quality images of blood vessels using radiofrequency waves in a magnetic field or using X-rays. The resulting images are used to determine the diameter of the vessel, the location and severity of the plaque.
- Angiography. During the study, a radiopaque contrast agent is injected into the artery and images are recorded to assess the condition of the vessels. The data obtained will help determine the optimal treatment methods for carotid artery atherosclerosis.
- You will be given detailed instructions about what you can and cannot drink and eat before your surgery.