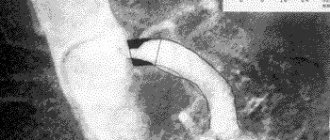
Angioplasty and stenting of the heart arteries is a method of treating coronary heart disease (CHD), which is performed without incisions under X-ray control and consists of restoring the patency of blocked coronary vessels. The essence of coronary angioplasty is to install a special catheter with a small balloon in the narrowing area. After inflation of the balloon, the lumen of the coronary artery is restored. To maintain the lumen of the coronary artery, it is necessary to install a metal frame - a stent.
Coronary angioplasty is a treatment that saves thousands of lives in patients with acute myocardial infarction. The advent of this technology has made it possible to reduce the mortality rate of a heart attack by 10 times and improve the quality of life in most patients with coronary artery pathology.
Long-term results of coronary angioplasty and stenting depend on follow-up and the stents used. Modern stents significantly improve the prognosis of the further course of the disease.
The endovascular clinic of the Innovative Vascular Center has achieved excellent results in emergency and planned operations for coronary heart disease. To correct stenoses and occlusions of the coronary arteries, we use the most modern endovascular instruments (balloons and stents). Every month, the clinic performs about 100 interventions on the coronary arteries in patients with acute coronary syndrome and elective angina.
- Our surgeons managed to achieve a minimum number of adverse outcomes in patients with myocardial infarction, and this figure remains the lowest in the Moscow region over the past years.
- Coronary angioplasty is performed using the latest Philips Allura Xper FD20 angiographic unit.
- Our endovascular surgeons use the safest radial approach on the arm.
- Our cardiac stenting technology often eliminates the need for coronary artery bypass grafting.
- We use the best stents to achieve optimal results.
- We have the most understandable and affordable prices for cardiac stenting.
What is coronary artery stenting?
More than 2 million stents are implanted annually. And this is understandable, because stents are used to treat one of the most common diseases - coronary heart disease.
Coronary angioplasty and stenting is an intravascular treatment for coronary heart disease. The basis of coronary heart disease is the narrowing of the blood vessels that supply the heart (coronary arteries) by cholesterol plaques. Stenting allows narrowed arteries to widen. To do this, a special balloon is placed inside the artery and inflated, thus “flattening” the cholesterol plaque and restoring blood flow through the artery. After this, a metal frame—a stent—is implanted into the narrowing site to “fix” the result. In this case, there is no need to open the chest and all manipulations are carried out through a small puncture in the artery in the arm or groin.
Types of stents
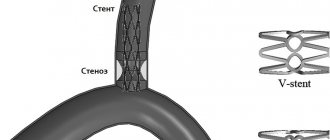
A stent is a high-tech design, which is a tubular frame made of a medical alloy (cobalt, steel, chromium, tantalum, platinum and nithiol), absorbable materials or polymers with improved biocompatibility, which, when placed in the lumen of a narrowed vessel, expand it and resume blood flow on it.
There are about 400 types of stents, differing in manufacturer, composition, cells, coating and placement system.
Types of stent designs:
- Balloon-expandable:
- tubular;
- spiral;
- wire;
- sinusoidal (ring).
- Self-expanding (mesh).
Cells are divided into closed, open, with tanks, various thicknesses of beams and lintels.
Stent shapes:
- cylindrical;
- conical;
- bifurcation;
- ultra-low profile (for narrow vessels).
Types of stents by type of coating:
- "Passive":
- carbon;
- titanium oxynitride;
- "artificial endothelium".
- Mechanical:
- stent grafts;
- with micro mesh.
- Medicinal:
- limus;
- paclitaxel;
- others (“Tacrolimus”, “Trapidil”, “Dexamethasone”, “Heparin”).
- Hybrid (combination of active and passive).
Hybrid stents have a polymer coating that releases a substance that resists endothelial fouling of the structure. The second layer encapsulates the stent, preventing metal particles from penetrating into the tissue.
The newest models have an asymmetric coating of the drug, which prevents it from entering the systemic bloodstream.
A new development in cardiology is biodegradable stents made in the USA, which provide temporary mechanical support for opening the coronary artery with subsequent resorption for 24 months. This group is intended for implantation in young patients or with non-calcified plaque.
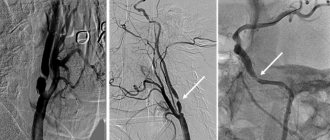
Who is indicated for cardiac stenting?
Stenting of cardiac vessels is indicated for patients with severe angina pectoris, after myocardial infarction and pre-infarction conditions, patients with proven ischemia (lack of blood to the heart) based on the results of stress tests. In this case, the decision on stenting is made only based on the results of coronary angiography - a contrast study of the heart vessels. Coronary angiography, like stenting, is performed in the cath lab. Often coronary angiography “transitions” into vascular stenting because performed through the same puncture in the artery.
Postoperative period
The patient is discharged on the 2nd day after surgery with a mandatory follow-up ultrasound scan.
After carotid artery stenting, combination antiplatelet therapy with clopidogrel 75 mg/day and aspirin 100 mg/day is prescribed for up to 12 months. Subsequently, aspirin and anti-cholesterol drugs - statins remain.
A control ultrasound scan is performed one month after stenting surgery. The patency of stented segments should be assessed at intervals of 6 months. If signs of restenosis are detected, the patient is prescribed a multislice computed tomography scan with contrast.
What alternative methods to stenting exist?
- Drug therapy. You need to understand that it is tablets, and not stents, that primarily reduce the risk of myocardial infarction and determine the prognosis in patients with coronary artery disease. Therefore, in many patients with controlled angina pectoris, in the absence of objective evidence of severe myocardial ischemia (lack of blood), coronary stenting can be abandoned, despite significant narrowing in the coronary arteries.
- Coronary bypass surgery. Abdominal surgery, which is often performed using a heart-lung machine. During bypass surgery, bypasses (shunts) are constructed from the patient’s arteries and veins, allowing blood to be supplied to the heart, bypassing areas of the arteries affected by cholesterol plaques.
Preparation for coronary angiography
To plan the operation, it is necessary to obtain information about the condition of the coronary arteries and heart function. For this purpose, diagnostic tests are carried out, which in an emergency include an ECG and laboratory diagnostics, and in a planned case, a more detailed examination is necessary.
Examination before elective surgery includes:
- ECG (including Holter monitoring)
- Echocardiography (including with load)
- MSCT coronary angiography or preliminary coronary angiography
- Gastroscopy (EGD)
- X-ray of the lungs
Before surgery, you may be given a loading dose of antithrombotic drugs to avoid early thrombotic complications.
How to choose between stenting, bypass surgery and drug therapy?
This is the task of your cardiologist, who takes into account the following data:
- The severity of symptoms, namely: the severity of angina pectoris, the severity of shortness of breath, in other words, how much ischemic disease “interferes with the life” of the patient.
- Objective evidence of myocardial ischemia (lack of blood). Most often this is a stress test, ideally stress echocardiography, which should be performed by qualified doctors in a center with a large number of such studies.
- Coronary angiography data. With widespread severe damage to all three coronary arteries, the results of bypass surgery are better.
- Accompanying illnesses. If a patient has diabetes mellitus and multivessel disease of the heart arteries, for example, coronary bypass surgery is usually indicated.
Complications
Every year the number of complications from the procedure decreases. This is due to improved tools, new drug support regimens and the accumulation of experience by doctors.
Possible complications:
- Cardiac (often develops during PTBA):
- spasm of the coronary artery (CA);
- dissection of the coronary artery (ruptures of the internal and/or muscular lining of the artery);
- acute vascular occlusion;
- phenomenon of non-resumption of blood flow;
- perforation of the operated vessel.
- Extracardiac:
- transient disturbance of cerebral blood flow;
- allergy to contrast agent;
- hematoma, infection, thrombotic occlusion, bleeding at the site of vessel puncture;
- ischemia of the lower extremities;
- retroperitoneal bleeding;
- contrast-induced nephropathy;
- lactic acidosis;
- microembolism.
In the postoperative period, rhythm disturbances, heart failure, and in 1.1% of cases - thrombocytopenia and bleeding are possible.
Technique for stenting coronary arteries (with professional jargon)
“We install the introducer”
To get to the heart vessels, the doctor needs to get into the patient’s arterial system. For this purpose, one of the peripheral arteries is used - the femoral (in the groin) or the radial (on the forearm). Under local anesthesia, a puncture is made in the artery and an introducer is installed - a special tube, which is the “entry gate” for all the necessary instruments.
"Let's put a guide"
Then a special thin-walled tube about a meter long - a guiding catheter (“guide”) is passed through the patient’s arteries and stops, slightly short of the heart, in the aorta. It is from the aorta that the coronary arteries that supply the heart depart. The tips of the catheters are curved in such a way that it is convenient for the doctor to enter one of the coronary arteries, right or left. By controlling the catheter, the doctor “enters” one of the coronary arteries. Half the job is done.
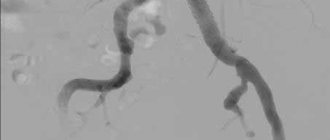
“Starting a conductor”
But how to get to the point of maximum narrowing in the artery? To do this, we need a “rail” along which all our tools will “ride”. This rail is the coronary guidewire - a thin (0.014 inch = 0.35 mm) metal “lint” with a soft tip (so as not to “scratch” the artery during the operation). Sometimes it is quite difficult to place a guidewire behind the site of narrowing; the tortuosity of the artery, the angle of departure of the branches of the artery, or pronounced narrowing due to the presence of plaques interfere. You can take a “harder” or “slipperier” conductor. Well, or just a favorite, because every doctor has his own preferences. One way or another, the guide ends up behind the site of narrowing on the periphery of the artery that we want to stent.
"Ballooning"
The first instrument that gets to the site of narrowing of the artery is a coronary balloon with a diameter most often from 1 to 3.5 mm and a length of 10-20 mm. The balloon is put on the conductor and moves along it to the point of maximum narrowing where it inflates. The pressure inside the cylinder reaches 15-20 A
Next, along the conductor, to the place that was narrowed before the balloon was inflated, the same balloon is inserted, on the surface of which a stent is fixed in a folded state. The balloon is inflated, the stent is expanded and “pressed” into the artery wall. The stent does not always expand perfectly and then the final stage of the procedure is needed - postdilatation (in simple terms - re-inflation).
"Let's blow it out"
A rigid balloon is placed inside the implanted stent and inflated with high pressure (up to 25 atmospheres). Most often, after this, the stent straightens and adheres well to the walls of the artery.
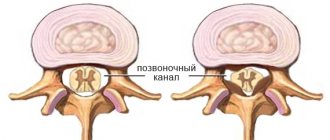
Application area
One of the common causes of the development of heart pathologies is a decrease in vascular elasticity and vasospasm. The arteries gradually lose their ability to expand, which leads to local disturbances in blood supply. Also, if the process is chronic, this contributes to the accumulation of cholesterol deposits on the vascular walls. Scientists all over the planet are actively working to develop an effective method to combat this disease. Coronary stenting is one of the existing ways to solve the problem.
Stenting is a procedure for integrating a special dilating device into a vessel. It is a tube with a mesh texture that can take the desired shape when implanted. The device acts as a frame. As a result, the narrow or spasmodic section of the artery should expand, and the blood flow should return to its previous state.
This treatment method belongs to endovascular surgical interventions and is considered minimally invasive. It is performed exclusively by experienced surgeons of the highest category.
Let's consider the stenting algorithm using the heart as an example. The catheter on which the element is fixed is passed through the femoral artery through the introducer. The conductor must be moved to the designated area where it is planned to install the expander. As soon as the catheter is inserted, the artificial frame is fixed, inflated under the action of the balloon, and normalizes blood supply to the heart muscle.
The operation involves local anesthesia. The average duration is relatively short, from 20 minutes to 3 hours. If necessary, the surgeon installs several devices at once.
Hemostasis
What to do with a hole in an artery?
If the intervention was carried out through the radial artery (on the arm), a special bracelet with a cushion (hemostatic cuff) is put on the wrist, which will put pressure on the injection site and prevent bleeding. Depending on the situation, the cuff will remain on the arm from 3 to 12 hours.
In case of femoral access, there are 2 main options:
- Manual (manual) hemostasis. After the introducer is removed, the doctor presses with his hands on the injection site for 15 minutes. Then apply a pressure bandage for 6-8 hours. The patient should lie on his back with his leg straight.
- Closure devices are special “plugs” that allow you to close the artery from the inside. In this case, there is no need to put pressure on the leg and a pressure bandage is not needed. A special patch is applied to the injection site and several hours of bed rest are recommended.
Stenting is completed.
Rehabilitation
The patient spends the first few hours in the intensive care unit, where the doctor monitors blood pressure levels and heart parameters. If there are no contraindications, during rehabilitation it is recommended to drink more fluid (about two liters per day) so that the body quickly removes the contrast fluid. It is better to avoid heavy lifting and intense exercise. A few days after discharge from the hospital, the patient returns to his normal life.
After surgery, it is important to strictly follow the doctor’s recommendations and attend scheduled cardiologist appointments on time. Taking blood-thinning drugs: aspirin (Cardiomagnyl, thrombo ACC, Cardiasca, etc.) and clopidogrel (Plavix) requires special attention.
General recommendations after surgery
Patients after bypass surgery and stenting are advised to have a proper, varied diet. It is necessary to avoid eating fatty, fried and salty foods. Products with high cholesterol content are strictly prohibited. At the request of the patient, you can receive a referral to a nutritionist who will write out the optimal individual diet.
The rehabilitation period after surgery involves taking medications. In addition to the standard set of medications, you must take anticoagulants prescribed by your doctor. Many people refuse them due to the high cost. However, ignoring the cardiologist’s instructions can lead to the formation of a blood clot in the installed stent/replaced area of the vessel.