Arterial hypertension (AH) is one of the most pressing health problems both in Russia and throughout the world. This is due to the high prevalence and high risk of its complications - coronary heart disease (CHD), cerebral strokes, heart and kidney failure. The prevalence of hypertension in economically developed countries reaches 25% [1].
In Russia, 40% of men and women over 18 years of age have elevated blood pressure (BP) [2]. According to Russian recommendations for the diagnosis and treatment of hypertension, the strategic goal of therapy for this disease is to reduce the risk of cardiovascular complications (CVC) as much as possible. The most important condition for effective antihypertensive therapy is adequate blood pressure control, i.e. achieving its target level, which is taken as blood pressure
However, in Russia, only 5.7% of men and 17.5% of women with hypertension achieve target blood pressure levels. If you do not increase the effectiveness of therapy, i.e., do not increase the proportion of adequately treated patients with hypertension, you cannot count on a turning point in reducing cardiovascular risk.
Currently, it is possible to use two strategies for treating hypertension to achieve target blood pressure: monotherapy and combination treatment (see figure). Monotherapy is based on finding the optimal drug for a particular patient, and switching to combination therapy is advisable only if the latter has no effect. Combination therapy already at the start of treatment involves the selection of an effective combination of drugs with different mechanisms of action.
Each of these approaches has its own advantages and disadvantages. The advantage of monotherapy is that if the drug is successfully selected, the patient will not need to additionally take another drug. However, as a rule, with monotherapy it is possible to achieve target blood pressure on average only in 30–40% of patients with hypertension. This is quite natural, since one class of drugs is not able to control all pathogenetic mechanisms of increased blood pressure: the activity of the sympathetic nervous system and the renin-angiotensin-aldosterone system, volume-dependent mechanisms. In addition, monotherapy requires the doctor to painstakingly search for the most optimal antihypertensive drug for the patient with frequent changes in drugs and their dosages, which often deprives the doctor and the patient of confidence in success and ultimately reduces adherence to treatment. This is especially true for patients with mild and moderate hypertension, most of whom do not experience discomfort from increased blood pressure and are not motivated to treatment.
The disadvantage of combination therapy is the inconvenience associated with the fact that the patient has to additionally take one more, and sometimes several, drugs. However, in most cases, the prescription of antihypertensive drugs with different mechanisms of action allows, on the one hand, to achieve target blood pressure, and on the other hand, to minimize the number of side effects. Combination therapy also makes it possible to suppress counterregulatory mechanisms of increased blood pressure. Thus, the transition to combination therapy, which allows effective control of various mechanisms of increased blood pressure, gives hope for increasing the effectiveness of antihypertensive therapy.
There are various combinations of antihypertensive drugs. Among the combinations of two drugs, the following are considered effective and safe: diuretic + beta-blocker; diuretic + ACE inhibitor (ACE inhibitor); diuretic + angiotensin II receptor antagonist (ARA); dihydropyridine calcium antagonist + beta-blocker; calcium antagonist + ACE inhibitor; calcium antagonist + diuretic; alpha-blocker + beta-blocker; centrally acting drug + diuretic. In addition, combinations of an ACE inhibitor, a calcium antagonist, an ARA and a diuretic with an I1 imidazoline receptor agonist are possible. The most popular in Russia is the combination of an ACE inhibitor and a diuretic. As the results of the Pythagoras study show, almost a third of doctors in Russia prefer a combination of these drugs [4].
The most important step towards improving the strategy of combination therapy was the creation of fixed combinations of antihypertensive drugs (two components in one tablet), which significantly improve patient adherence to therapy. However, along with the advantages (the ability to take one tablet containing two drugs), this approach also has serious disadvantages. Thus, the doctor cannot vary the doses of each of the drugs included in the combination, which complicates treatment, especially when adverse reactions occur that are clearly related to one of the components included in the combination. To avoid such difficulties, it was necessary to create several different dosage forms, which may partially alleviate the problem (for example, the drugs Enap-H and Enap-HL, containing different doses of the diuretic), but does not solve it completely.
In this regard, it is of interest to create non-fixed combinations containing two drugs in one blister, which will allow, if necessary, to vary the doses of each of them. The first drug of this type in Russia was Enzix - a combination of enalapril with indapamide.
The creation of this form of the drug was largely facilitated by the results of the multicenter study EPIGRAF, in which doctors from 38 clinics from 17 cities of Russia took part [5]. In total, the study included 550 patients with grades II–III hypertension (initial systolic blood pressure > 160 mm Hg), and among them there were patients not only with essential, but also with symptomatic hypertension. A feature of this study was that already at the beginning of treatment, patients were prescribed a combination of enalapril and indapamide. Moreover, if the dose of indapamide was constant - 2.5 mg, then the dose of enalapril varied depending on the initial blood pressure level. However, doctors had the opportunity to adjust doses depending on the achievement of the target blood pressure level within 14 weeks. The average dose of enalapril in the study was 15.2 mg. As a result of treating patients with hypertension with differentiated doses of enalapril and indapamide, it was possible to achieve a significant reduction in both systolic and diastolic blood pressure. Moreover, in 70% of patients it was possible to achieve the target blood pressure level, despite its very high initial level. Adverse reactions were noted in only 8.1% of patients, and in 5.4% they were due to an excessive decrease in blood pressure, which can be eliminated with more careful selection of drug dosages.
The main conclusion of the study is that the effectiveness and safety of the combination of enalapril with indapamide in the treatment of hypertension does not depend on gender, age and the cause of the increase in blood pressure (primary hypertension or secondary hypertension of renal origin). Particular attention should be paid to the latter circumstance in connection with the entrenched opinion that the effectiveness of antihypertensive therapy is lower in patients with symptomatic hypertension. The combination of enalapril with indapamide was especially preferred in women in whom ACE inhibitor monotherapy may be less effective.
The results of the EPIGRAF study made it possible to work out the most effective doses of enalapril and indapamide for patients with hypertension of varying degrees, which became the basis for the creation of three types of the drug Enzix: ENZIX - 10 mg of enalapril and 2.5 mg of indapamide (single dose in the morning) for patients with stage I hypertension; ENZIX DUO – 10 mg enalapril and 2.5 mg indapamide (morning) + 10 mg enalapril (evening) for patients with stage II hypertension; ENZIX DUO FORTE – 20 mg enalapril and 2.5 mg indapamide (morning) + 20 mg enalapril (evening).
The effectiveness and safety of Enzix were assessed in the EPIGRAPH-2 study, which was a comparative randomized multicenter study that included nine centers in Russia and one in Serbia [6]. A total of 313 patients were included in the study and randomized into two groups. The Enzix group included 211 patients, and the control group included 102 patients. The control group was treated with other classes of antihypertensive drugs (except ACE inhibitors and diuretics). After 2, 4 and 6 weeks of treatment in cases where it was not possible to achieve target blood pressure (
All patients randomized to the Enzix group were divided into two subgroups depending on the initial blood pressure level.
In the first subgroup, 118 patients with stage I hypertension and initial systolic blood pressure of 140–160 mm Hg. Art. a combination of 10 mg enalapril and 2.5 mg indapamide (corresponding to the ENZIX form) was prescribed. During treatment, 88 (74.6%) of them continued to take the original dose, and in 26 (22.1%) patients the dose of enalapril was doubled (10 mg in the morning + 10 mg in the evening) while maintaining the dose of indapamide (2.5 mg in the morning ), which corresponded to the ENZIX DUO form. Only one patient with stage I hypertension required a combination of 40 mg of enalapril (20 mg in the morning + 20 mg in the evening) and 2.5 mg of indapamide, which corresponded to the ENZIX DUO FORTE form. Three patients did not complete the study.
In the second subgroup, 93 patients with stage II hypertension and systolic blood pressure 160–180 mm Hg. Art. Therapy began with 20 mg of enalapril (10 mg each morning and evening) and 2.5 mg of indapamide (corresponding to the ENZIX DUO form). During treatment in 46 patients, this dosage was maintained, and in 45 patients, the dose of enalapril was increased to 40 mg/day (20 mg in the morning + 20 mg in the evening) with a constant dose of indapamide 2.5 mg, which corresponded to the form of ENZIX DUO FORTE. For two more patients, the initial dose of enalapril was reduced to 10 mg while maintaining the original dose of 2.5 mg of indapamide, which corresponded to the ENZICS form.
When analyzing the number of patients whose blood pressure levels normalized as a result of treatment, the group of patients receiving Enzix (72.5%) had some advantages compared to the control group (66.7%). And this, despite the fact that systolic blood pressure in the “experimental” group was initially 2.7 mm Hg. Art. higher than in the control. If we sum up the total number of patients who responded positively to treatment (the number of patients with normalization of blood pressure or a decrease in systolic blood pressure by more than 20 mm Hg from the initial level), then by the end of treatment it reached 82.4% on average for the group, taking Enzix, and among patients with stage I hypertension this value was 89.8%, and in patients with stage II hypertension – 77.2%.
Thus, early treatment of patients with grades I–II hypertension with a non-fixed combination of enalapril and indapamide (Enzix) in comparison with routine antihypertensive therapy makes it possible to achieve normalization of blood pressure levels more often. In addition, the Enzix group was able to significantly reduce the number of patients with left ventricular hypertrophy and proteinuria, improve quality of life, and reduce the number of hospitalizations and additional visits to the doctor. Among other things, Enzix therapy is cost-effective.
Very important importance is currently attached to the metabolic effects of antihypertensive therapy. The essence of the metabolic theory is that a number of antihypertensive drugs, such as diuretics and beta-blockers (especially non-selective ones), tend to worsen the lipid profile and worsen insulin resistance, which can in the long term increase the risk of developing diabetes mellitus and reduce the effectiveness of therapy in preventing the development of cardiovascular disease [7].
Recently completed large-scale studies have confirmed the validity of the metabolic theory. In groups of patients taking diuretics and beta-blockers, the incidence of diabetes was significantly higher than when treated with calcium antagonists, ACE inhibitors and ARBs [8–10]. In this regard, the effectiveness of antihypertensive therapy must be assessed not only from the point of view of achieving target blood pressure, but also from the standpoint of the likelihood of metabolic effects. This fully applies to combination therapy. It is appropriate to emphasize that the components of Enzix do not cause concern in this regard. Enalapril, as studies show, is metabolically neutral, and indapamide occupies a special place among diuretics. At recommended doses (1.5–2.5 mg per day), it not only provides adequate antihypertensive effects, but is also metabolically neutral. It has been proven that indapamide does not cause hypokalemia or changes in carbohydrate [11] and lipid profiles [12]. Particularly compelling evidence for the metabolic indifference of indapamide comes from a meta-analysis of three studies involving a total of 1195 patients. Based on the results of treatment with the retard form of indapamide for 9–12 months, no effect on carbohydrate and lipid profiles, as well as uric acid levels, was detected [13].
In addition to the diuretic effect, indapamide has a vasodilating effect by reducing the sodium content in the arterial wall, regulating the entry of calcium into vascular smooth muscle cells, as well as increasing the synthesis of prostaglandin E2 in the kidneys and prostacyclin in the endothelium [14]. Thus, indapamide, having a more pronounced direct effect on blood vessels compared to other diuretics, affects endothelial function. It has an antioxidant effect, increasing the bioavailability of NO and reducing its destruction [15]. The LIVE study demonstrated the ability of indapamide therapy to cause regression of left ventricular myocardial hypertrophy [16].
Modern rational combination therapy in the treatment of patients with arterial hypertension
According to epidemiological studies, the prevalence of arterial hypertension (AH) among adults in developed countries ranges from 20 to 40% and increases with age [1]. Elevated blood pressure is found in more than 50% of men and women over 60 years of age [2]. The relevance of the problem is supported by the increasing processes of urbanization of society, which create the preconditions for the emergence of risk factors (RFs), such as stress, physical inactivity, obesity, bad habits and disturbed ecology. Elevated blood pressure is one of the main risk factors for the development of cerebral stroke, coronary heart disease (CHD) and other cardiovascular diseases of atherosclerotic origin, which are associated with more than 50% of all deaths [3].
Clinical practice and the results of many multicenter studies have shown [4–6] that the use of monotherapy in the treatment of hypertension rarely leads to target blood pressure levels, increases the risk of adverse events and reduces patient adherence to treatment. The use of drugs in a rational combination regimen requires compliance with a number of mandatory conditions: safety and effectiveness of the components; the contribution of each component to the expected result; different but complementary mechanism of action of the components; the best result compared to each of the components; balance of components in terms of bioavailability and duration of action; strengthening organoprotective properties; impact on the universal (most common) mechanisms of blood pressure increase; reduction in adverse events and improved tolerability [7–9].
According to modern national recommendations [10], recommendations of the European Society of Arterial Hypertension (EOH) and the European Society of Cardiology (ESC) [11], the treatment tactics for essential hypertension depend on the level of blood pressure and the degree of risk of cardiovascular complications. The main goal of treatment is to minimize the risk of developing cardiovascular complications (CVD) and death from them. The main objectives are normalization of blood pressure levels in order to prevent complications, in the absence or minimal level of adverse drug reactions (ADRs), correction of all modifiable risk factors (smoking, dyslipidemia, hyperglycemia, obesity), prevention, slowing down the rate of progression and/or reducing organ damage - targets, as well as treatment of associated and concomitant diseases - coronary artery disease, diabetes mellitus (DM), etc. [10, 11].
When treating patients with hypertension, blood pressure should be less than 140/90 mm Hg. Art., which is its target level. If the prescribed therapy is well tolerated, it is advisable to reduce blood pressure to lower values. In patients with a high and very high risk of cardiovascular disease, it is necessary to reduce blood pressure to 140/90 mm Hg. Art. or less within 4 weeks. In the future, subject to good tolerance, it is recommended to reduce blood pressure to 130/80 mmHg. Art. and less. In patients with coronary artery disease, blood pressure should be reduced to the target value of 130/85 mm Hg. Art. In patients with diabetes and/or kidney disease, the target blood pressure level should be less than 130/85 mmHg. Art. [10].
Of course, treatment for hypertension should begin with lifestyle changes: reducing excess body weight, limiting the consumption of table salt and alcoholic beverages, increasing physical activity, etc. Limiting the consumption of table salt is a fairly effective way to reduce blood pressure. It was noted that limiting the consumption of table salt enhances the antihypertensive effect of many antihypertensive drugs, including AT1-angiotensin receptor blockers and β-blockers.
One of the most important conditions for ensuring adequate blood pressure control and increasing patient adherence to treatment is the optimal choice of antihypertensive drug as part of mono- or combination pharmacotherapy.
Currently, five main classes of antihypertensive drugs are recommended for the treatment of hypertension [10]:
1. angiotensin-converting enzyme inhibitors (ACE inhibitors) (captopril, enalapril, perindopril, lisinopril, fosinopril, quinapril, trandolapril, etc.);
2. AT1 receptor blockers (ARBs) (valsartan, losartan, telmisartan, candesartan, irbesartan, etc.);
3. slow calcium channel blockers (SCBC) (nifedipine, amlodipine, etc.);
4. beta-blockers (BAB) (carvedilol, bisoprolol, nebivolol, metoprolol tartrate, metoprolol succinate, atenolol, etc.);
5. thiazide and thiazide-like diuretics (hydrochlorothiazide (HCTZ), indapamide).
As additional classes of antihypertensive drugs for combination therapy, α-blockers (prazosin, doxazosin), imidazoline receptor agonists (moxonidine), and a direct renin inhibitor (aliskiren) can be used.
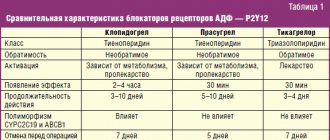
According to these national recommendations [10], the choice of an antihypertensive drug should be related to the characteristics of its action, belonging to a certain class, since at present, the results of clinical studies conducted according to the rules of evidence-based medicine have made it possible to establish situations of preferential class choice of drugs. When choosing an antihypertensive drug, it is necessary first of all to evaluate the effectiveness, the likelihood of side effects and the benefits of the drug in a specific clinical situation (Table 1).
The choice of drug is influenced by many factors, the most important of which are:
- the patient has a risk factor;
- target organ damage;
- concomitant clinical conditions, kidney damage, MS, diabetes;
- concomitant diseases for which it is necessary to prescribe or limit the use of antihypertensive drugs of various classes;
- the patient’s previous individual reactions to drugs of various classes;
- the likelihood of interaction with medications prescribed to the patient for other reasons;
- socioeconomic factors, including the cost of treatment.
It is necessary to begin treatment with the use of one drug in the minimum daily dose (this recommendation does not apply to patients with severe hypertension or those in whom previous therapy was ineffective). The use of new drugs should begin with the use of low doses, the goal of each successive stage of treatment should be to reduce blood pressure levels by 10–15% [10]. If blood pressure does not decrease to the desired level, further treatment is carried out by gradually - step by step - increasing doses or adding new drugs. Ineffective drugs (not causing a decrease in blood pressure by 10–15 mm Hg) and drugs that cause ADRs should be replaced [12].
There are no uniform recommendations regarding which drugs should be used to start treating a patient. The choice of drugs depends on age, gender and the presence of concomitant diseases.
Currently, the treatment of most patients with hypertension uses drugs that alter the activity of the RAAS. These are ACE inhibitors, beta blockers and angiotensin II receptor blockers (ARBs). ARBs are one of the modern and most dynamically developing classes of antihypertensive drugs. ARBs suppress the effect of angiotensin II through AT1 receptors. It has been established that hypersecretion of angiotensin II leads not only to the development of hypertension, but also to damage to target organs, being one of the main factors in the progression of hypertension and its complications, remodeling of the heart and blood vessels. It is no coincidence that AT1-angiotensin receptor blockers are classified as the main antihypertensive drugs. Numerous controlled studies, such as LIFE, VALUE, MARVAL, PRIME, IDNT, DETAIL [13], have shown that AT1 blockers are effective and safe antihypertensive drugs. AT1-angiotensin receptor blockers have proven to be particularly effective in preventing the development of cerebral stroke. To prevent stroke in patients with hypertension, AT1 blockers can be used both instead of diuretics or calcium antagonists, and together with them. ARBs, like ACEIs, can also prevent the development of type 2 diabetes, reducing the risk of its occurrence by 20–25% [14]. Therefore, it can be assumed that AT1-angiotensin receptor blockers should be used for the treatment of hypertension primarily in patients with a high risk of developing stroke or diabetes. Excellent tolerability is an undoubted advantage of AT1 blockers during long-term antihypertensive therapy. The use of AT1-angiotensin receptor blockers can improve patient adherence to long-term therapy, since ARBs are much less likely than other antihypertensive drugs to be discontinued due to the development of side effects. Unlike thiazide diuretics, beta blockers and ACE inhibitors, the antihypertensive effectiveness of AT1-angiotensin receptor blockers does not depend on the age, gender or race of patients [15].
The renin-angiotensin-aldosterone system (RAAS) plays a central role both in the occurrence of hypertension and in the implementation of pathophysiological processes that ultimately lead to serious cardiovascular complications such as cerebral stroke, myocardial infarction, vascular remodeling, nephropathy, congestive heart failure and the development of atherosclerotic processes. ACE inhibitors were the first group of drugs acting directly on the RAAS, which were widely introduced into clinical practice. The long period of their use, numerous clinical studies, and extensive experience of practical doctors in their use have led to the fact that these drugs are currently used in Russia more often than other antihypertensive drugs. ACE inhibitors in moderate doses reduce SBP to a slightly lesser extent than diuretics and calcium antagonists. The choice of a specific ACEI for long-term therapy in patients with hypertension has important clinical implications, since these drugs are prescribed essentially for life. Of the ACE inhibitors with proven effectiveness, perindopril and ramipril seem to be the most promising [16, 17].
Clinical practice and the results of many multicenter studies have shown that the use of monotherapy in the treatment of hypertension rarely leads to target blood pressure levels, increases the risk of adverse events and reduces patient adherence to treatment. The most important conditions for increasing patients’ adherence to treatment are their understanding of the goals, objectives, modern methods and principles of treatment, as well as the correct choice of antihypertensive treatment by the doctor. The tactics of using combination therapy with the selection of drugs with different mechanisms of action already at the beginning of treatment gives a much greater chance of successful blood pressure control. Low-dose combination rational antihypertensive therapy may be the first choice measure, especially in patients with a high risk of developing cardiovascular complications, the advantages of which include: a simple and convenient dosage regimen for the patient; facilitating titration; ease of prescribing the drug; increasing patient adherence; reduction of adverse events by reducing doses of components used; reducing the risk of using irrational combinations; confidence in the optimal and safe dosage regimen; reduction in price [17–21].
It should be noted that the latest both American and European recommendations emphasize the need to avoid, if possible, the tactics of frequent changes in medications and their dosages in patients. It is now becoming obvious that the effectiveness of monotherapy with drugs of all main groups is low and comparable: after a year of treatment, even with almost perfect adherence to treatment, the effect of monotherapy does not exceed 50% versus almost 30% with placebo. The tactics of “sequential monotherapy” in reality may require 4–5 changes in therapy, each of which may be complicated by the development of side effects. This tactic takes a lot of time, deprives the doctor and the patient of confidence in success, which ultimately has a negative psychological impact on the patient and leads to low adherence to treatment for hypertension. It is the underestimation of the role of combination therapy that is one of the common reasons for unsatisfactory blood pressure control [17–21].
Combination antihypertensive therapy has many advantages:
- enhancing the antihypertensive effect due to the multidirectional effects of drugs on the pathogenetic mechanisms of hypertension development, which increases the number of patients with a stable decrease in blood pressure;
- reducing the incidence of side effects both due to lower doses of combined antihypertensive drugs and due to the mutual neutralization of these effects;
- ensuring the most effective organ protection and reducing the risk of development and number of cardiovascular complications.
Numerous randomized clinical trials and real clinical practice experience have shown all the advantages of combination therapy, which can be summarized as follows [22, 23]:
- simultaneous use of drugs from two different pharmacological groups more actively reduces blood pressure due to the fact that there is an effect on various pathogenetic mechanisms of hypertension;
- the combined use of lower doses of two drugs acting on different regulatory systems will allow for better control of blood pressure, given the heterogeneity of the response of hypertensive patients to antihypertensive drugs;
- prescribing a second drug may weaken or balance the triggering of mechanisms to counteract the decrease in blood pressure that occurs when prescribing one drug;
- a sustained decrease in blood pressure can be achieved with smaller doses of two drugs (than with monotherapy);
- smaller doses allow you to avoid dose-dependent side effects, the likelihood of which is higher with a larger dose of a particular drug (during monotherapy);
- the use of two drugs can to a greater extent prevent damage to target organs (heart, kidneys) caused by hypertension;
- prescribing a second drug can to a certain extent reduce (and even completely eliminate) the undesirable effects caused by the first (even if quite effective) drug;
- Prescribing a second drug (in particular, a diuretic) allows you to obtain a rapid antihypertensive effect of a combination of drugs, since most antihypertensive drugs (ACE inhibitors, CCBs, ARBs, and partly beta blockers) exhibit their full effect only in the 2-3rd week . reception (and even later).
Combinations of two antihypertensive drugs are divided into rational (effective), possible and irrational. All the advantages of combination therapy are inherent only in rational combinations of antihypertensive drugs [24].
These include [10]:
- ACE inhibitor + diuretic;
- ARB + diuretic;
- ACEi + dihydropyridine BMCC;
- ARB + dihydropyridine BMCA;
- dihydropyridine BMCC + BAB;
- dihydropyridine BMCC + diuretic;
- beta blocker + diuretic;
- BAB + α-adrenergic blocker.
The issue of combining three or more drugs has not yet been sufficiently studied, since there are no results from randomized controlled clinical trials studying the triple combination of antihypertensive drugs. Thus, the antihypertensive drugs in these combinations are grouped together on a theoretical basis. However, in many patients, including patients with refractory hypertension, only with the help of three or more component antihypertensive therapy can the target blood pressure level be achieved [25]. Recommended combinations of three antihypertensive drugs include:
- ACE inhibitor + dihydropyridine BMCC + beta blocker;
- ARB + dihydropyridine BMCA + BAB;
- ACE inhibitor + BMCC + diuretic;
- ARB + BMCC + diuretic;
- ACE inhibitor + diuretic + beta blocker;
- ARB + diuretic + beta blocker;
- dihydropyridine BMCC + diuretic + beta-blocker.
Since combination therapy has become one of the main directions in the treatment of patients with hypertension, fixed combinations of antihypertensive drugs containing two drugs in one tablet have become widespread, which improves the patient’s psychological attitude towards treatment and makes it possible to reduce the risk of complications and side effects. The optimal combination of components implies the absence of unwanted hypotension, which can lead, especially in elderly patients, to increased cardiovascular risk. Rational selection of components according to their pharmacokinetic profile creates the prerequisites for single use of drugs that require two or three times in monotherapy.
The advantages of fixed (official) combinations include:
- potentiation of the antihypertensive effect of drugs;
- ease of administration and dose titration process;
- reduction in the frequency of side effects (low dose, mutual neutralization of NDR);
- increasing patient adherence to treatment;
- reducing the cost of treatment.
Currently, there are quite a lot of official combination drugs: Capozide (captopril + HCTZ), Co-Renitek (enalapril + HCTZ), Noliprel (perindopril + indapamide), Accusid (quinapril + HCTZ), Co-diovan (valsartan + HCTZ), Gizaar (losartan + HCTZ), Exforge (valsartan + amlodipine), Equator (lisinopril + amlodipine), Logimax (metoprolol + felodipine), Tarka (verapamil + trandolapril), etc. The most frequently prescribed of all non-fixed and fixed drug combinations is the combination of an ACE inhibitor with a thiazide diuretic or an ARB with a thiazide diuretic. The high effectiveness and safety of this combination in the treatment of hypertension is noted in the recommendations of the WHO, VNOK, EOG - EOC and JNS 7. The action of type 1 AT receptor blockers is specific, since they, unlike ACE inhibitors, do not affect the activity of other neurohumoral systems, in particular bradykinin, which are associated with characteristic side effects (dry cough and angioedema). The effect of “escape” of pharmacological blockade of the RAAS from the action of ACE inhibitors is explained by the synthesis of angiotensin II in some organs and tissues with the help of other enzymes without the participation of ACE.
It is currently believed that chronic stimulation of the RAAS leads to the activation of growth factors and fibrosis at the tissue level, which determines the development of pathological processes in target organs, therefore the possibility of blocking the tissue link of the RAAS seems promising for achieving the organoprotective effect of antihypertensive therapy. A number of studies have not revealed a direct dependence of the reno- and cardioprotective effect of antihypertensive therapy on the degree of blood pressure reduction, which indicates the importance of non-hemodynamic effects of RAAS blockade. When used together, thiazide diuretics not only enhance but also prolong the antihypertensive effect of ARBs. The combined use of ARBs and diuretics has been shown to significantly reduce blood pressure in patients with both high and low renin activity, and the response to this combination therapy is about 80% or higher.
Another example of a favorable combination is the combination of BMCC with an ACE inhibitor, which leads to a decrease in the severity of edema associated with the use of dihydropyridines. In addition, the combination of a non-dihydropyridine BMCC with an ACE inhibitor may potentially enhance the positive effect of the latter on vascular elastic properties.
Irrational combinations, in which there is no potentiation of the antihypertensive effect of drugs and/or side effects are enhanced when used together, include combinations of beta blockers and centrally acting drugs, beta blockers and non-dihydropyridine BMCCs, and beta blockers with ACE inhibitors, ARBs, and imidazoline receptor agonists. The combination of ACEIs and ARBs is currently considered prohibited.
Conclusion
The most important conditions for increasing patients’ adherence to treatment are their understanding of the goals, objectives, modern methods and principles of treatment, as well as the correct choice of antihypertensive treatment by the doctor. The tactics of using combination therapy with the selection of drugs with different mechanisms of action already at the beginning of treatment provides a significantly greater chance of successfully controlling blood pressure and the risk of developing cardiovascular complications. The advantages of combination therapy consist in potentiating the antihypertensive effect and reducing the number of side effects and are inherent only in so-called rational combinations of antihypertensive drugs. For adequate treatment of hypertension, it is advisable to use combination therapy, starting with low doses of drugs.
Literature
- Oganov R.G., Timofeeva T.N., Koltunov I.E. and others. Epidemiology of arterial hypertension in Russia. Results of federal monitoring 2003-2010 // Cardiovascular therapy and prevention. 2011. No. 1. P. 9–13.
- ABC Of Hypertension / edited by D. Gareth Beevers, Gregory H. Lip and Eoin O'Brien. 5th ed. Malden, Mass.: BMJ Books, 2007. p. 88.
- Ezzati M., Lopez AD, Rodgers A. et al. Selected major risk factors and global and regional burden of disease // Lancet. 2002. Vol. 360(9343). P. 1347–1360.
- Hansson L., Zanchetti A., Carruthers SG et al. Effects of intensive blood–pressure lowering and low–dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomized trial // Lancet. 1998. Vol. 351. P. 1755–1762.
- Dahlof B. Sweedish trial in old patients with hypertension (STOP-Hypertension). //Clm. Exp. Hypertens. 1993. Vol. 15. P. 925–939.
- Chazova I.E., Belenkov Yu.N. ROSA – Russian study on optimal blood pressure lowering. https://www. cardiosite.ru/research/article.asp? id=2559.
- Karpov Yu.A. Combination therapy of arterial hypertension - control effect and treatment success // Breast Cancer. 2006. No. 20. pp. 1458–1461.
- 1999 World Health Organization – International Society of Hypertension Guidelines for the Management of Hypertension // J. Hypertens. 1999. Vol. 17. P. 151–183.
- Kobalava Zh.D. Evolution of combination antihypertensive therapy: from multicomponent high-dose free combinations to low-dose fixed combinations as the first choice // Breast Cancer. 2001. No. 18. pp. 789–794.
- Diagnosis and treatment of arterial hypertension. Recommendations of the Russian Medical Society on arterial hypertension and the All-Russian Scientific Society of Cardiologists. Fourth revision // Systemic hypertension. 2010. No. 3. P. 5–26.
- ESH-ESC Guidelines Committee. 2013 guidelines for the management of arterial hypertension // J. Hypertension. 2013. Vol. 31. P. 1281–1357.
- Karpov Yu.A. New recommendations for arterial hypertension RMOAG/VNOK 2010: issues of combination therapy // RMZh. 2010. No. 22. P. 1290.
- Polosyants O.B. Sartans in cardiological practice // RMZh. 2008. No. 11. pp. 1593–1597.
- Preobrazhensky D.V., Peresypko M.K., Nosenko N.S. and others. AT1-angiotensin receptor blockers: range of organoprotective effects // Handbook of a polyclinic physician. 2004. No. 1. P. 8–14.
- Matcar DB, McCrory DC, Orlando LA et al. Comparative Effectiveness of Angiotensin-Converting Enzyme Inhibitors (ACEIs) and Angiotensin II Receptor Antagonists (ARBs) for Treating Essential Hypertension. Comparative Effectiveness Review no. 10. (Prepared by Duke Evidence-based Practice Center under Contract No. 290-02-0025.) Rockville, MD: Agency for Healthcare Research and Quality. November 2007. Available at: www.effectivehealthcare.ahrq.gov/reports/final.cfm
- Moiseev S.V. Valsartan: from the realities of clinical practice to new opportunities // Clinical pharmacology and pharmacotherapy. 2009. No. 3. P. 32–43.
- Kirichenko A.A., Ebzeeva E.Yu. Differentiated approach to the treatment of arterial hypertension // Consilium Medicum. 2006. T. 4. No. 3.
- Preobrazhensky D.V., Stetsenko T.M. and others. Therapy of hypertension: combinations of an ACE inhibitor and a diuretic // Consilium Medicum. 2006. T. 4. No. 7.
- 1999 World Health Organization – International Society of Hypertension Guidelines for the Management of Hypertension // J. Hypertens. 1999. Vol. 17. P. 151–183.
- Gosse P., Sheridan DJ, Zannad F. et al. Regression of LVH in hypertensive patients treated with indapamide SR 1.5 mg versus enalapril 20 mg: the LIVE study // J. Hypertens. 2000. Vol. 18. P. 1465–1475.
- Chalmers J., Castaigne A., Morgan T. et al. Long-term efficacy of a new, fixed, very-low-dose angiotesin-converting enzyme-inhibitor/diuretic combination as first-line therapy in elderly hypertensive patients // J. Hypertens. 2000. Vol. 18. P.1–11.
- Bubnova M.G. Modern principles of prevention and treatment of arterial hypertension. Analysis of the main provisions of international recommendations // Directory of a polyclinic doctor. 2005. No. 4. P. 8–14.
- Preobrazhensky D.V., Stetsenko T.M. and others. Selection of the optimal drug for long-term therapy of arterial hypertension // Consilium Provisorum. 2005. No. 2. pp. 21–23.
- Arutyunov G.P., Rozanov A.V. Pharmacotherapy of arterial hypertension: the place of fixed combinations of drugs // Arterial hypertension. 2003. No. 6. pp. 218–221.
- Chazova I.E., Belenkov Yu.N., Ratova L.G. and others. From idea to clinical practice. First results of the Russian national study of optimal blood pressure reduction (ROSA) // Syst. hypert. 2004. No. 2. P. 18–23.
- Chalmers J., Castaigne A., Morgan T. et al. Long-term efficacy of a new, fixed, very-low-dose angiotesin-converting enzyme-inhibitor/diuretic combination as first-line therapy in elderly hypertensive patients // J. Hypertens. 2000. Vol. 18. P. 1–11.
Antihypertensive therapy as the basis of neuroprotection in modern clinical practice
Arterial hypertension (AH) is one of the most pressing problems of modern therapy, cardiology and neurology. The prevalence of hypertension in European countries, including the Russian Federation, is in the range of 30–45% of the general population, with a sharp increase as the population ages. Hypertension is a leading risk factor for the development of cardiovascular diseases (CVD), such as myocardial infarction (MI), cerebral stroke, coronary heart disease (CHD), chronic heart failure (CHF), as well as cerebrovascular diseases (CVD): chronic cerebral ischemia brain (CHI), hypertensive encephalopathy, ischemic or hemorrhagic stroke, transient ischemic attack. Hypertension is the most common component of comorbidity in the practice of any doctor, present in 90% of cases of all possible combinations of diseases [1, 2]. The most common comorbidity is hypertension with atherosclerosis or dyslipidemia. The main complication of atherosclerosis of the coronary arteries is coronary artery disease, myocardial infarction and cardiosclerosis, leading to progressive CHF, and damage to the main arteries of the brain is manifested by symptoms of CCI with the subsequent development of vascular dementia or cerebral stroke [3, 4]. Today, about 9 million people in the world suffer from CVD. All this makes it relevant to constantly study the problem of early diagnosis and correction of hypertension in order to prevent the most common CVDs and CVDs [5].
Quadruple antihypertensive combination - capabilities and advantages
The key point in the use of antihypertensive therapy remains effective control of blood pressure (BP) and achieving optimal values, determined individually for each patient, taking into account all existing risk factors for CVD and concomitant conditions. Today, five main classes of antihypertensive drugs are recommended for the treatment of hypertension: angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), calcium antagonists (CAs), beta-blockers (BBs) and diuretics, for which the ability to prevent the development of cardiovascular complications proven in numerous randomized clinical studies. All of these classes of drugs are suitable for initial and maintenance therapy, both as monotherapy and as part of combinations. Early start with rational combination therapy is a new approach recommended by modern guidelines for the treatment of hypertension [6, 7]. Let's consider which combinations of antihypertensive drugs are rational, well studied and most often prescribed in modern therapy. ACE inhibitors block the formation of angiotensin II from angiotensin I, preventing vasospasm and ensuring the maintenance of target blood pressure values. In clinical practice, the most commonly used drugs are enalapril, lisinopril, and captopril [7]. Enalapril has the most extensive evidence base for reducing overall mortality - 7 studies (n = 12,791 patients) [8]. Separately, it should be emphasized that in modern therapy it is enalapril that takes the lead in the treatment and prevention of CHF. Antihypertensive drugs from the diuretic group reduce the load on the myocardium, reducing circulating blood volume (CBV). A decrease in blood volume under the influence of diuretics is achieved due to the accelerated removal of fluid from the body. Loop diuretics reduce the reabsorption of Na+, K+, Cl– in the thick ascending part of the loop of Henle, reducing fluid reabsorption, have a fairly pronounced and rapid effect and, as a rule, are used only for emergency care (for forced diuresis in pulmonary edema, overhydration, etc. .). The most well-known drug in this group is furosemide. Thiazide-like diuretics (hypothiazide, indapamide, chlorthalidone), reducing the reabsorption of Na+ and Cl– in the thick segment of the ascending loop of Henle and in the initial part of the distal tubule of the nephron, reduce urine reabsorption. When taken systematically in patients with hypertension, the risk of cardiovascular complications is reduced. A representative of thiazide-like diuretics, indapamide does not cause disturbances in lipid and carbohydrate metabolism, and therefore is widely used in patients with various types of metabolic disorders, unlike other representatives of this class. A combination with BBs is also possible, which act on the vascular system by stimulating b-adrenergic receptors and are widely used in clinical practice in patients with hypertension and vascular comorbidity. BBs reduce the heart rate, lengthening diastole and improving blood supply to the myocardium, since the heart receives substances necessary for functioning from the blood only during diastole. Independent randomized studies confirm a decrease in heart rate and an increase in life expectancy in patients with long-term use of BB [5]. The most popular beta-blockers with a proven improvement in prognosis, including in patients with coronary artery disease, are metoprolol, bisoprolol, and carvediol. ACs are used no less widely than BBs in the clinical practice of treating hypertension. These drugs block the entry of calcium into vascular smooth muscle cells and cardiomyocytes. This blockade is accompanied by vasodilation, but at the same time, a weakening of myocardial contractility. In addition, AKs reduce the activity of the sinus node, and when blood pressure drops, they can cause tachycardia. Thus, with a brief discussion of the most frequently prescribed classes of drugs in the form of mono- or combination therapy, taking into account evidence-based medicine, additional properties and, of course, the economic component of treatment, it was possible to identify the leaders. This is how the modern low-dose neuroprotective combination drug Hypotef was created. Hypotef contains enalapril, indapamide, metoprolol tartrate and vinpocetine; it has a complex effect, influencing all stages of the development of target organ damage in hypertension, which is especially important in patients with CVD. A special feature of Hypotef is not only the unique combination of the three most popular antihypertensive classes, which provide multifaceted organoprotective support and improve the prognosis, but also the nootropic vinpocetine included in the drug, which potentiates the antihypertensive effect and has a powerful evidence base for improving the state of cerebral circulation [9]. The effectiveness of vinpocetine has been repeatedly confirmed in large-scale studies, so it has been shown that vinpocetine therapy helps reduce the severity of neurological symptoms such as headache, dizziness, tinnitus in patients with hypertension, as well as a significant improvement in mood and memory. In patients after an ischemic stroke, the use of vinpocetine, compared with the control group, contributed to a greater extent to the regression of speech, motor and memory disorders [9]. Hypotef has a uniform, long-term antihypertensive effect with the achievement of target blood pressure values comparable to the effect of 20 mg of enalapril or 50 mg of metoprolol [10]. The gradual decrease in blood pressure was well tolerated by patients, without symptoms of hypotension, even with a significant decrease in blood pressure (maximum to –31.3/16 mmHg over 12 weeks of treatment) [11]. A comparative study of FORCAGE with modern antihypertensive combinations showed the same organ-protective effectiveness of Hypotef in relation to the kidneys and heart and higher efficiency in reducing vascular age (1.5 times), arterial stiffness (1.5 times) and intima-media thickness (1.7 times) [12, 13]. Hypotef normalizes diurnal variability: in the Hypotef group, the number of “dippers” increased by 32%, and in the group taking other modern combinations, only by 25%, while in this group the number of patients with an excessive nocturnal decrease in blood pressure increased. With a comparable hypotensive effect, Hypotef was well tolerated by patients, there were no cases of hypotension, and patient compliance was higher than in the comparison groups [11–13]. The possibility of effective use of the drug Hypotef in a patient with hypertension and a high additional risk can be considered in the following clinical example.
Patient A., born in 1965, came to see a general practitioner at the district clinic with complaints of rapid heartbeat, headache, frequent dizziness, “noise and ringing” in the ears, severe fatigue during exercise, and memory impairment.
Heredity: father - stroke, acute coronary syndrome at the age of 50 years; mother - hypertension, coronary artery disease, type 2 diabetes mellitus, sister - hypertension, type 2 diabetes mellitus.
Anamnesis. Over the course of several years, blood pressure increased to max 200/110 mm Hg. Art., currently receives enalapril 5 mg 2 times a day as antihypertensive therapy, adapted to 150/90 mmHg. Art. Several years ago, fasting hyperglycemia was first identified; a test with 75 g of glucose revealed impaired glucose tolerance. Since then, the patient has been following a diet, monitoring her weight, and her weight is stable.
Past illnesses: frequent colds, duodenal ulcer.
Epidemiological history: tuberculosis, viral hepatitis, diabetes mellitus.
Bad habits: smokes, does not abuse alcohol.
Allergy history: Pinosol nasal drops - Quincke's edema.
Current condition: general condition is satisfactory.
On physical examination: the patient's height is 175 cm, weight 95 kg, body mass index - 31 kg/m2, waist circumference - 112 cm, hip circumference - 100 cm, and the waist-to-hip ratio is > 0.95, indicating abdominal type of obesity, which is usually combined with metabolic disorders. Hypersthenic physique. The skin is of normal color. Subcutaneous fat tissue is moderately developed. There is no swelling. In the lungs there is vesicular breathing, no wheezing. NPV = 16 per minute. Heart sounds are clear, rhythmic, heart rate = 88 per minute. Blood pressure = 152/90 mm Hg. Art. The abdomen is soft, painless on palpation. The liver is not enlarged. The effleurage symptom is negative on both sides.
Based on the results of laboratory and instrumental examination, no changes in the results of clinical blood and urine tests were detected. Biochemical analysis is presented in table. 1.
According to echocardiography: signs of left ventricular hypertrophy. Left ventricular ejection fraction - 61%.
The results of 24-hour blood pressure monitoring (Table 2) confirmed the presence of hypertension, despite the therapy being taken. The average systolic blood pressure (SBP) per day was 154 mm Hg. Art. (daytime SBP - 157 mm Hg), diastolic blood pressure (DBP) - 95 mm Hg. Art., which exceeded normal values. A disturbance in the circadian rhythm of SBP of the non-dipper type was noted, i.e., lack of a sufficient reduction in blood pressure at night, which is especially unfavorable with regard to the development of complications such as stroke, heart attack, chronic cerebral ischemia and cognitive impairment.
Diagnosis: “Arterial hypertension, 1st degree, risk IV. NK - 0. Hyperlipidemia IIb. Obesity 1st degree. Visceral type of obesity. Prediabetes: impaired glucose tolerance. Impaired fasting glucose. Duodenal ulcer without exacerbation.”
Received therapy at the time of treatment: Enap 5 mg 2 times a day (morning, evening); Omez 20 mg 1 time/day (at night).
The therapy received was adjusted:
1) Enap was replaced with the drug Hypotef - 1 tablet in the morning and 1 tablet in the evening; 2) the drug pitavastatin 4 mg, 1 tablet in the evening after dinner was added to the therapy.
When the patient was re-examined after 3 months, it was revealed that during the therapy, the patient’s condition improved significantly: headaches regressed, general well-being improved, performance increased, the sensation of “noise and ringing” in the ears, as well as “lapses” in memory, disappeared. To assess the effectiveness of therapy, repeated 24-hour blood pressure monitoring was carried out; the results confirmed the achievement of target values - up to 125/80 mm Hg. Art. and normalization of the daily blood pressure profile (Table 3). Biochemical analysis showed achievement of target values for LDL and total cholesterol levels (Table 4). It was also noted that there was no worsening of carbohydrate disorders during the therapy.
Thus, rational antihypertensive therapy prescribed to the patient in the form of a low-dose combined neuroprotective drug Hypotef and statin therapy showed high effectiveness in a short time. The disappearance of symptoms such as headache, dizziness, tinnitus, as well as a subjective feeling of improved memory makes the patient committed to this therapy and makes it possible to carry out long-term treatment. The patient tolerates the prescribed therapy well; she is recommended to continue taking all previously prescribed medications under monitoring lipid levels and blood pressure.
Taking into account modern recommendations for the treatment of hypertension and data on the study of the clinical effectiveness of the drug Hypotef, it seems possible to talk about a truly rational solution to many problems in a patient with hypertension using one unique four-component neuroprotective drug - Hypotef, which can significantly improve the patient’s quality of life and avoid unsafe polypharmacy.
Literature
- Redon J., Olsen MH, Cooper RS, Zurriaga O., Martinez-Beneito MA, Laurent S. et al. Stroke mortality trends from 1990 to 2006 in 39 countries from Europe and Central Asia: implications for control of high blood pressure // Eur Heart J. 2011; 32: 1424–1431.
- Shishkova V.N. Neuroprotection in patients with arterial hypertension: minimizing an unfavorable prognosis // Therapeutic archive. 2014; 8: 113–118.
- Shishkova V.N. Cognitive impairment as a universal clinical syndrome in the practice of a therapist // Therapeutic archive. 2014; 11: 128–134.
- Stroke. Guide for doctors / Ed. Kotova S.V., Stakhovskoy L.V. M: MIA Publishing House, 2013.
- Shishkova. V. N., Adasheva T. V., Kapustina L. A. Fundamentals of stroke prevention in modern clinical practice // Doctor. 2018; 29 (7): 3–12.
- Chazova I.E., Zhernakova Yu.V. on behalf of the experts. Clinical recommendations. Diagnosis and treatment of arterial hypertension // Systemic hypertension. 2019; 16 (1): 6–31.
- 2018 EOK/EOAG Recommendations for the treatment of patients with arterial hypertension // Russian Journal of Cardiology. 2018; 23 (12): 143–228.
- Korzun A. I., Kirillova M. V. Comparative characteristics of ACE inhibitors. St. Petersburg: VMedA, 2003. 24 p.
- Chukanova E. I. Modern aspects of the epidemiology and treatment of chronic cerebral ischemia against the background of arterial hypertension (results of the CALIPSO program) // Neurology, neuropsychiatry, psychosomatics. 2011; 3 (1): 38–42.
- Evdokimova A. G. et al. Clinical effectiveness of combination antihypertensive therapy in fixed doses: focus on Hypoteff // Therapy. 2016; 6 (10): 68–78.
- Skotnikov A. S., Khamurzova M. A. Organoprotective properties of antihypertensive therapy as prevention of the development of “vascular” comorbidity // Treating Physician. 2017; 7: 16–24.
- Skotnikov A.S., Yudina D.Yu., Stakhnev E.Yu. Antihypertensive therapy of a comorbid patient: what to focus on when choosing a drug // Attending Physician. 2018; 2:24–30.
- Skotnikov A. S., Khamurzova M. A. New combinations for the complex treatment of arterial hypertension to help the general practitioner // Polyclinic. Cardiologist today. Special issue. 2017/2018; 1:47–55.
V. N. Shishkova, Candidate of Medical Sciences
FSBEI HE MGMSU named after. A. I. Evdokimova Ministry of Health of the Russian Federation, Moscow
Contact Information
DOI: 10.26295/OS.2019.68.63.015
Antihypertensive therapy as the basis of neuroprotection in modern clinical practice / V. N. Shishkova For citation: Attending physician No. 6/2019; Page numbers in the issue: 68-73 Tags: antihypertensive therapy, organ-protective support, comorbidity, cerebral circulation