Pharmacological properties
Pharmacodynamics.
Telmisartan is an oral specific angiotensin II receptor antagonist (type AT1). With high affinity, telmisartan replaces angiotensin II at the sites of its binding to a variety of at1 receptors, through which the action of angiotensin II is mediated. Telmisartan does not exhibit any partial agonist effect on the at1 receptor. Telmisartan selectively binds to the AT1 receptor for a long time, without exerting even a partial agonistic effect on it. The bond is long lasting.
Telmisartan has no affinity for other receptors, including AT2 receptors and other AT receptors. The functional role of these receptors is not clear, as is the effect of their possible stimulation by angiotensin II, the levels of which are increased by telmisartan. Telmisartan reduces plasma aldosterone levels, does not block ion channels and does not reduce plasma renin levels. It does not inhibit angiotensin-converting enzyme (kininase II), an enzyme that also breaks down bradykinin. Therefore, bradykinin-mediated side effects are not expected.
In humans, a dose of 80 mg of telmisartan almost completely inhibits the increase in blood pressure caused by angiotensin II. The inhibitory effect lasts throughout the day and is determined up to 48 hours.
Pharmacokinetics. Telmisartan is rapidly absorbed, but the amount of drug that is absorbed varies. The average bioavailability of telmisartan is about 50%.
When telmisartan is administered with food, the AUC for telmisartan decreases from about 6% (40 mg dose) to about 19% (160 mg dose). 3 hours after administration, the concentration in the blood plasma becomes the same as when using telmisartan without food. It is believed that a slight decrease in AUC does not reduce the therapeutic effectiveness of the drug. There is no linear relationship between dose and plasma levels. Cmax and, to a lesser extent, AUC increase disproportionately at doses above 40 mg.
Telmisartan is highly bound to plasma proteins (more than 99.5%), mainly to albumin and α1-acid glycoprotein. The mean volume of distribution (Vss) at equilibrium is approximately 500 L.
Telmisartan is metabolized by conjugation to the glucuronide of the parent compound, which has no pharmacological activity.
Telmisartan is characterized by a biexponential pharmacokinetic curve with a terminal half-life of more than 20 hours. Cmax in blood plasma and, to a lesser extent, AUC increase disproportionately to the dose. When using telmisartan in recommended doses, no clinically significant accumulation was detected. Plasma concentrations were higher in women than in men, without a corresponding effect on efficacy.
After administration (and intravenous administration), telmisartan is almost completely excreted in the feces, mainly unchanged. Cumulative urinary excretion is less than 1% of the administered dose. The total plasma clearance (CLtot) is high (about 1000 ml/min) compared to blood flow through the liver (about 1500 ml/min).
Special categories of patients
Children. The pharmacokinetics of two doses of telmisartan were assessed as a secondary objective in hypertensive patients (n=57) aged 6 to 18 years after receiving telmisartan at a dose of 1 or 2 mg/kg body weight for 4 weeks of treatment. Pharmacokinetic objectives included determining steady-state telmisartan levels in children and adolescents and examining age-related differences. Although the study was powered to reliably evaluate pharmacokinetics in children under 12 years of age, the results are generally consistent with those obtained in adults and support the nonlinearity of telmisartan, particularly for Cmax.
Floor. Cmax and AUC in women are approximately 3 and 2 times higher, respectively, than in men.
Elderly patients. The pharmacokinetics of telmisartan do not differ between elderly patients and those under 65 years of age.
Patients with impaired renal function. In patients with moderate, moderate and severe renal failure, a 2-fold increase in plasma concentrations was noted. However, low plasma concentrations were detected in patients with renal failure undergoing dialysis. Telmisartan has a high affinity for plasma proteins in patients with renal failure and cannot be eliminated by dialysis. In patients with renal failure, T½ does not change.
Patients with impaired liver function. Pharmacokinetic studies in patients with liver impairment demonstrated an increase in bioavailability to approximately 100%. In patients with liver failure, T½ does not change.
Head of the Department of Internal Medicine No. 1 of the Tashkent Medical Academy. Doctor of Medical Sciences, Associate Professor, N. M. Nurillaeva.
Increased activity of the reninangiotensin system (RAS) is one of the main targets for pharmacological intervention in patients with high blood pressure (BP). Angiotensin type 1 receptor blockers or sartans act directly on angiotensin II type 1 receptors (AT1), suppressing its main physiological effects: vasoconstrictor, increased aldosterone synthesis and catecholamine release from the adrenal glands and presynaptic membranes, stimulation of myocardial hypertrophy and vascular smooth muscle cells , as well as collagen synthesis. By being highly specific and preventing the action of angiotensin II at the tissue level, these drugs provide more complete RAS blockade than angiotensin-converting enzyme inhibitors (ACEIs). Alternative pathways for the formation of angiotensin II have been established, especially at the level of the tissue component of the RAS, where its formation occurs without the participation of ACE, but with the participation of other enzymes (tonin, chymases, cathepsin). Compared to other classes of antihypertensive drugs, sartans cause fewer adverse reactions and are better tolerated. When treated with AT1 receptor blockers, the content of kinins does not increase, which avoids side effects due to the accumulation of bradykinin, such as cough and angioedema, observed when taking ACE inhibitors.
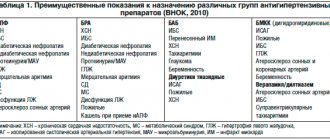
Sartans are the drugs of choice for the treatment of arterial hypertension (AH), with concomitant metabolic syndrome, left ventricular hypertrophy and microalbuminuria/proteinuria of any origin, as well as chronic heart failure (CHF). Currently, the ARB group is represented by four subgroups that differ in chemical structure: biphenyl tetrazole derivatives - losartan, irbesartan, candesartan; non-biphenyl tetrazole derivatives – telmisartan; non-biphenyl non-tetrazoles – eprosartan; non-heterocyclic compounds – valsartan. One of the most famous and widely studied representatives of the class of AT1 receptor blockers with proven organoprotective properties is telmisartan.
The pharmacokinetic properties of telmisartan have a number of advantages that significantly expand the therapeutic possibilities of using antihypertensive drugs: the longest half-life, unlike other AT1 blockers, with the simultaneous absence of metabolic oxidation in the liver through the cytochrome P450 isoenzyme system and the effect of food intake on bioavailability. Moreover, in a comparative in vitro study, it was found that telmisartan has the highest AT1 receptor binding ability among various sartans: telmisartan > olmesartan > candesartan ≥ valsartan ≥ losartan. In this case, the corresponding decay rate constants in the same order were: 0.0032, 0.0042, 0.0052, 0.0099, 0.010 per minute with half-lives of 213, 166, 133, 70, 67 minutes. The high lipophilic properties of telmisartan contribute to its maximum absorption and penetration into tissues with simultaneous blockade of systemic and tissue RAS. The volume of distribution of telmisartan is the largest among AT1 receptor blockers - 500 liters, which contributes to its wide penetration into tissues. Telmisartan is excreted in the bile and no dose adjustment is required in patients with mild to moderate renal insufficiency; however, in patients with severe renal insufficiency, including those on hemodialysis, an initial dose of 20 mg once daily is recommended. Telmisartan is not removed from the blood during hemodialysis. After its withdrawal, the blood pressure level gradually returns to its original level without the manifestation of “rebound” syndrome.
Telmisartan, in addition to blocking AT1 receptors, is a partial agonist of peroxisome proliferator-activated receptor subtype g (PPARg). They are directly involved in the development of insulin resistance and metabolic syndrome, as they provide regulation of glucose formation in the liver. Unlike other AT1 blockers, telmisartan has maximum effectiveness in stimulating PPARg receptors. In a comparative study by S. Benson et al. (2004) in vitro demonstrated the ability of telmisartan to increase the activity of PPARg receptors by 27 times, while the other 6 sartans increased their activity only by 2–3 times. These advantages of telmisartan are associated with the structure of its molecule, which is similar to thiazolidinediones, and the activation of PPARg receptors by telmisartan accounts for 25–30% of the maximum effect of pioglitazone or rosiglitazone, used in the treatment of diabetes mellitus and metabolic syndrome.
The antihypertensive efficacy of telmisartan in real clinical practice was assessed in the MICARDIS Community Access Trial (MICCAT-2), which included 1615 patients with arterial hypertension (AH). To objectify the results obtained, the method of daily monitoring (ABPM) was used. Initially, telmisartan was prescribed at a dose of 40 mg, after 2 weeks the dose was increased to 80 mg for office blood pressure ≥140/85 mm Hg. Art., after 4 weeks, if necessary, hydrochlorothiazide was added at a dose of 12.5 mg, and after 4 subsequent weeks, the achieved antihypertensive effect was analyzed in patients. The decrease in office blood pressure in 675 previously untreated patients and in 940 previously treated patients was -23/-12 and -17/-10 mmHg. Art. respectively. According to ABPM results, the average daily blood pressure decreased by 16.8/11.4 mmHg. Art. in persons with an initial blood pressure level during the day ≥130/85 mm Hg. Art.. In general, at the end of the MICCAT-2 study, 79% of patients achieved control when measuring office blood pressure and 70% achieved control when carrying out ABPM. Control of blood pressure during the day while taking telmisartan was also accompanied by a significant decrease in blood pressure in the early morning hours, the most vulnerable time for patients with cardiovascular diseases (CVD), which amounted to 11.5/-7.0 mm Hg. Art., and in 95 patients with an initially high level of blood pressure during these hours (>30 mm Hg. Art.), it decreased by -17.2/-10.1 mm Hg. Art..
The multicenter randomized trials PRISMA I and II using ABPM compared the hypotensive effects of telmisartan at a dose of 40–80 mg per day and ramipril at a dose of 2.5–10 mg per day in patients with stage I–II hypertension. Patients in two groups were prescribed to take these drugs in the morning. After 14 weeks of treatment, average daily blood pressure decreased by 14.8/9.9 mmHg. Art. in the telmisartan group, which was significantly different from the achieved blood pressure per day in the group of patients taking ramipril, in whom the decrease in blood pressure averaged 7.9/5.4 mm Hg. Art. [23, 50]. Researchers paid special attention to the dynamics of blood pressure in the last 6 hours of the drug dosing time interval to assess their effect on blood pressure in the early morning hours, which are associated with an increased risk of developing acute coronary and cerebrovascular accidents. In patients treated with telmisartan, in the last 6 hours of action of the drug, a decrease in blood pressure was observed to a greater extent, in contrast to those in the ramipril group (-12.7/-8.8 and -7.9/-5.4 mm Hg. Art. respectively; p<0.05).
Other comparative clinical studies have also demonstrated the antihypertensive benefits of telmisartan among representatives of the class of AT1 receptor blockers in terms of duration and strength of action, especially in the early morning hours, and even in the case of skipping a drug dose, in contrast to losartan, candesartan, and valsartan.
Clinical observations were conducted on the effectiveness and safety of the use of telmisartan in patients with hypertension in combination with diabetes mellitus or obesity in the multicenter randomized trial SMOOTH. With the combined use of telmisartan at a dose of 80 mg and hydrochlorothiazide at a dose of 12.5 mg for 6 weeks, a positive effect of treatment on blood pressure control during the day and in the early morning hours was demonstrated with good tolerability and no changes in metabolic parameters (blood glucose, glycated hemoglobin, total cholesterol, triglycerides, potassium...
The prospective ATHOS study in 1000 elderly patients over 60 years of age and with a predominant increase in systolic blood pressure (SBP) analyzed the daily BP profile after 6 weeks of use of telmisartan at a dose of 40–80 mg with hydrochlorothiazide 12.5 mg compared with amlodipine at a daily dose of 5–80 mg. 10 mg with hydrochlorothiazide 12.5 mg [33]. The decrease in SBP in the last 6 hours from the time of taking these drugs was comparable in both groups of elderly patients - 18.3 and -17.4 mmHg. Art. respectively. However, SBP control during the day in the telmisartan group was higher - 65.9% - compared to amlodipine - 58.3% (p = 0.012). Premature discontinuation of treatment was observed more often in patients in the amlodipine group (11.3%) in contrast to the telmisartan group (5%), mainly due to the appearance of peripheral edema.
Despite the fact that in the ProFESS study, additional administration of telmisartan did not significantly reduce the number of recurrent ischemic strokes in patients, experimental studies have shown that telmisartan is able to penetrate the blood-brain barrier and block the vasoconstrictor effect of angiotensin II on cerebral arteries [18, 45, 52 ]. These results may indirectly explain the proven improvement in cognitive function within 24 weeks in elderly patients 61–75 years old with hypertension in the clinical observation of R. Fogari et al. (2006). After 12 weeks of treatment, with the combined use of telmisartan at a dose of 80 mg with hydrochlorothiazide at a dose of 12.5 mg, there was a significant improvement in the assessment of episodic memory on the corresponding scale by 17.1% compared to the baseline, as well as in indicators of visuospatial orientation.
The use of drugs that block the RAAS helps reduce the progression of kidney damage in patients with hypertension and diabetes mellitus by reducing pressure in the renal glomeruli, the activity of inflammation and oxidative stress. Evidence of the renoprotective effect of telmisartan, independent of antihypertensive action, has been demonstrated at all stages of the renal continuum, from improving endothelial function to reducing proteinuria in patients in the TRENDY, DETAIL, INNOVATION studies.
The comparative AMADEO study demonstrated the superiority of the renoprotective effect of telmisartan compared to losartan in patients with hypertension and type 2 diabetes mellitus complicated by nephropathy [4]. After 52 weeks of treatment, in the group of people taking telmisartan, there was a more significant decrease in the ratio of protein to creatinine in the urine, in contrast to those taking losartan (29% versus 20%; p = 0.03) with comparable values of reduction in blood pressure. Another study, VIVALDI, with a similar population to the AMADEO study, found no differences in reductions in urinary protein excretion, creatinine clearance, and GFR between patients taking telmisartan 80 mg daily and valsartan 160 mg daily.
To date, according to the results of clinical studies, there is evidence in addition to the antihypertensive properties of the pleiotropic effects of telmisartan, the main of which are increased sensitivity to insulin, improved endothelial function, renoprotective effect in both hypertensive and normotensive patients, reduction of left ventricular hypertrophy (LVH) and episodes of atrial fibrillation (Table 2).
The most significant multicenter studies that examined the effect of telmisartan on cardiovascular morbidity and mortality are ONTARGET and TRANSCEND.
The aim of the ONTARGET study was to compare monotherapy with telmisartan at a dose of 80 mg per day with monotherapy with the ACE inhibitor ramipril at a dose of 10 mg and their combined use on the effect on the development of cardiovascular complications (CVD) and mortality in patients with vascular diseases or diabetes mellitus with organ damage . The primary composite endpoint included cardiovascular mortality, nonfatal myocardial infarction, nonfatal stroke, and heart failure hospitalizations. At a median follow-up of 56 months, primary endpoint events occurred in 1423 patients (16.7%) in the telmisartan group, 1412 (16.5%) in the ramipril group, and 1386 (16.3%) in the telmisartan group. with simultaneous administration of telmisartan and ramipril. Despite the fact that the ONTARGET study initially did not include patients with intolerance to ACE inhibitors, during the treatment of patients in the ramipril group, 360 people (4.2%) developed a cough, which was observed significantly less often in the group of patients taking telmisartan (1.1%; p<0.001). Angioedema appeared in 25 patients (0.3%) in the ramipril group, in contrast to those in the telmisartan group, where this side effect was observed in 10 people (0.1%; p = 0.01). In the group of combined use of telmisartan and ramipril, in comparison with other groups, the largest number of side effects was recorded: hypotensive episodes occurred in 4.8% of cases, cough - 4.6%, syncope - 0.3%, renal dysfunction - 13, 5%. Based on the increased incidence of severe renal failure in this group of patients, the latest European guidelines on arterial hypertension (2013) prohibit the simultaneous use of ACE inhibitors and sartans in the combined treatment of patients with hypertension [28]. Treatment with RAS blockers had a significant protective effect on LVH. It was concluded that telmisartan was non-inferior to ramipril in reducing cardiovascular mortality and complications and was associated with fewer side effects, particularly cough and angioedema, than ramipril.
The placebo-controlled TRANSCEND trial assessed the effect of telmisartan on the prevention of CV events in high-risk patients with CVD or diabetes mellitus with organ damage (without proteinuria) who were intolerant to ACE inhibitors. The primary endpoint was similar to the ONTARGET study, and composite endpoints similar to the HOPE and ADVANCE studies were also studied. There were no significant differences over 5 years in the number of complications in patients between the telmisartan and placebo groups included in the primary endpoint. However, in the number of adverse outcomes, a composite endpoint of micro- and macrovascular disease, similar to the ADVANCE study, telmisartan treatment compared with placebo achieved a significant 11% reduction in the cumulative incidence of cardiovascular death, non-fatal myocardial infarction or stroke. , hemodialysis, 2-fold increase in serum creatinine, new cases of proteinuria, or use of laser therapy for diabetic retinopathy (RR = 0.89). Also in the TRANSCEND study, significant differences were revealed in secondary endpoints - in the telmisartan group compared with placebo, there was a decrease in new cases of both LVH by 38% and microalbuminuria/proteinuria by 23%, a decrease in the progression of microalbuminuria to proteinuria by 42%, a reduction in cases hospitalizations for CVD by 8%. The renoprotective effect of telmisartan was also demonstrated by the effect on the composite endpoint of hemodialysis, 2-fold increase in serum creatinine, or new cases of microalbuminuria and/or proteinuria - with a 19% reduction in the number of cases compared with patients taking placebo.
A comparative retrospective analysis by JW Lin et al. (2014) with 690,463 Korean patients at high cardiovascular risk demonstrated potential differences between the most common AT1 receptor blockers in their effects on overall and cardiovascular mortality [25]. Patients treated with telmisartan and olmesartan had a 7% lower relative risk of all-cause mortality compared with patients treated with losartan (HR=0.93; 95% CI 0.90–0.96 and HR=0.93; 95 % CI 0.88–0.97, respectively). A study of the causes of deaths showed that treatment of patients with olmesartan reduced the relative risk of cardiovascular mortality by 16%, and telmisartan reduced the relative risk of mortality from cerebrovascular diseases by 11% compared with treatment with losartan.
Thus, the pharmacological properties and proven clinical effects of the AT1 receptor blocker telmisartan provide wide opportunities for its use in daily clinical practice in the treatment of patients with high and very high risk hypertension, especially in combination with obesity, diabetes mellitus, and kidney damage for the purpose of effective control blood pressure and reduce the risk of developing cardiovascular events.
To summarize the still short, but already rich in interesting results, history of the study and use of ARBs in evidence-based cardiology, it should be concluded that telmisartan is a modern and effective antihypertensive drug that has a number of advantages over other ARB drugs in terms of the ability to prevent the development and progression of cardiovascular accidents, nephropathy in patients with diabetes mellitus and having a cardiovascular and nephroprotective effect similar to ACE inhibitors is characterized by better tolerability. In addition, further study of new mechanisms of the positive effect of telmisartan on carbohydrate, fat metabolism and the cardiovascular system through PPARγ modulation can significantly expand the indications for its use in clinical practice.
Currently, the government is actively promoting a course to stimulate import substitution of medicines. One of them is the drug Mirel (telmisartan).
Mirel at a dose of 80 mg completely blocks the hypertensive effect of angiotensin II. Its effect lasts more than 24 hours (including the last 4 hours before taking the next dose) and persists after 48 hours. The onset of the hypotensive effect is noted within 3 hours after the first dose. The maximum reduction in blood pressure is observed 4 weeks after the start of treatment. In patients with arterial hypertension, Mirel (telmisartan) reduces systolic and diastolic blood pressure without affecting heart rate. In case of abrupt discontinuation of the drug, blood pressure gradually returns to its original level without the development of withdrawal syndrome. The effect of Mirel (telmisartan) on cardiovascular disease and mortality has not been established. Clinical studies have shown that the use of Mirel (telmisartan) is associated with a statistically significant decrease in left ventricular mass in patients with arterial hypertension and left ventricular hypertrophy.
Pharmacokinetics. After oral administration, it is quickly absorbed from the gastrointestinal tract. Bioavailability is about 50%. When Mirel (telmisartan) is taken simultaneously with food, the reduction in AUC values ranges from 6% (at a dose of 40 mg) to 19% (at a dose of 160 mg). 3 hours after taking the drug, the concentrations of telmisartan in the blood plasma level out, regardless of taking the drug on an empty stomach or with food.
Distribution. Binding to blood plasma proteins is more than 99.5%, mainly with albumin and α1-glycoprotein. The average apparent Vd at equilibrium is approximately 500 L.
Metabolism. Mirel (telmisartan) is metabolized by conjugation with glucuronic acid. The metabolite does not exhibit pharmacological activity.
Excretion. T1/2 - more than 20 hours. Mirel (telmisartan) is mainly excreted in feces, mainly unchanged, through the kidneys - less than 2%. Total plasma clearance is quite high (approximately 900 ml/min) compared to hepatic blood flow (approximately 1,500 ml/min).
Unlike other sartans (Valsartan, Losartan, candesartan, olmesartan, eprosartan, irbesartan), Mirel has a pronounced effect on the receptors that activate peroxisome proliferator (Peroxisome Proliferator Activated Receptor, PPAR), and provides a synergistic effect on key risk factors for the development of cardiovascular complications . Prescribed for adults orally at a dose of 40 mg 1 time / day. In some patients, a hypotensive effect can be achieved by prescribing the drug at a dose of 20 mg/day. If necessary, the dose of the drug can be increased to 80 mg/day. It should be borne in mind that the maximum hypotensive effect develops after 4-8 weeks. In patients with severe arterial hypertension, telmisartan is used in a daily dose of 160 mg (as monotherapy) or in combination with hydrochlorothiazide 12.5-25 mg/day. Patients with renal failure (including those on hemodialysis), elderly patients do not require dose adjustment of the drug. In patients with mild to moderate liver dysfunction, the daily dose of the drug should not exceed 40 mg.
Side effect. From the central nervous system: headache, dizziness, fatigue, insomnia, anxiety, depression, convulsions, visual disturbances. From the cardiovascular system: marked decrease in blood pressure (including orthostatic hypotension), bradycardia, tachycardia, chest pain; rarely - fainting. From the respiratory system: infections of the upper respiratory tract (including pharyngitis, bronchitis, sinusitis), cough; rarely - dyspnea. From the digestive system: nausea, vomiting, dyspepsia, diarrhea, abdominal pain, impaired liver function. From the urinary system: impaired renal function (including acute renal failure), peripheral edema, urinary tract infections (including cystitis), hypercreatininemia. From the musculoskeletal system: myalgia, arthralgia, low back pain, tendinitis-like symptoms, leg cramps. From the hematopoietic system: rarely - anemia, eosinophilia, thrombocytopenia. Laboratory indicators: rarely - hyperkalemia, hyperuricemia; in isolated cases - an increase in the level of CPK in the blood. Allergic reactions: skin rash; rarely - erythema, itching, eczema, sweating, urticaria, angioedema. Other: influenza-like syndrome.
Contraindications: obstruction of the biliary tract; severe liver dysfunction; hereditary fructose intolerance; pregnancy; lactation period (breastfeeding); hypersensitivity to telmisartan and other components of the drug. The drug is not indicated for use in children and adolescents, because There are no data on efficacy and safety in this category of patients. Mirel (telmisartan) is contraindicated for use during pregnancy and during pregnancy. There is no experience with the use of telmisartan in patients after kidney transplantation. When using Mirela (telmisartan) in patients with impaired renal function, it is recommended to regularly determine serum potassium and creatinine levels. In patients with reduced blood volume and hyponatremia resulting from diuretic therapy, restriction of salt intake, diarrhea or vomiting, when using telmisartan, a pronounced decrease in blood pressure may develop, especially when prescribing the drug for the first time. Reduced blood volume and hyponatremia should be restored before using telmisartan. In cases where vascular tone and renal function are largely dependent on the activity of the renin-angiotensin-aldosterone system (for example, in patients with severe chronic heart failure or concomitant kidney diseases, including renal artery stenosis), the use of drugs which affect the state of this system may be accompanied by the development of acute arterial hypotension, hyperazotemia, oliguria and, in rare cases, acute renal failure. Therefore, caution should be exercised in prescribing telmisartan to this category of patients. In patients with primary aldosteronism, antihypertensive drugs whose mechanism of action is to inhibit the activity of the renin-angiotensin-aldosterone system are usually ineffective. In such cases, the use of telmisartan is not recommended. In patients with aortic or mitral stenosis, idiopathic hypertrophic subaortic stenosis, the use of telmisartan (as well as other vasodilators) requires special caution. It should be taken into account that when using antihypertensive drugs in patients with ischemic cardiopathy or coronary artery disease, in the event of an excessive decrease in blood pressure, myocardial infarction or cerebrovascular accident may develop. It should be taken into account that when using telmisartan, especially in the presence of kidney disease and/or heart failure, as well as simultaneously with potassium-sparing diuretics, salt substitutes containing potassium, and other drugs that increase the concentration of potassium in the blood (heparin), the risk of developing hyperkalemia increases. Therefore, in these cases it is recommended to monitor the level of potassium in the blood. Telmisartan should be prescribed with caution to patients with impaired liver function. Since telmisartan is excreted mainly in the bile, the elimination of the drug may be delayed in patients with impaired liver function. If pregnancy is planned, telmisartan should be replaced with another antihypertensive drug. If pregnancy is established, the use of telmisartan should be discontinued as soon as possible. Preclinical studies did not reveal a teratogenic effect of the drug, but a fetotoxic effect was noted.
.Drug interaction. The simultaneous use of telmisartan with thiazide diuretics (hydrochlorothiazide) is possible, since this increases the hypotensive effect. Temilsartan may enhance the hypotensive effect of other antihypertensive drugs. No other clinically significant interactions were identified. Digoxin, warfarin, hydrochlorothiazide, glibenclamide, ibuprofen, paracetamol, simvastatin and amlodipine were studied in pharmacokinetic studies. There was an increase in the average digoxin concentration by 20% (in one case the increase in concentration reached 39%). When using telmisartan and digoxin simultaneously, it is advisable to periodically determine the concentration of digoxin in the blood. With the simultaneous use of ACE inhibitors and lithium preparations, a reversible increase in the concentration of lithium in the blood was observed, accompanied by a toxic effect. In rare cases, such changes have been reported with the use of angiotensin II receptor antagonist drugs. When using lithium preparations and angiotensin II receptor antagonists simultaneously, it is recommended to determine the concentration of lithium in the blood. With simultaneous use of telmisartan with NSAIDs (including acetylsalicylic acid at a dose of ≥0.3 g/day and COX-2 inhibitors), acute renal failure may develop in patients with dehydration. Patients taking telmisartan in combination with NSAIDs should be adequately hydrated and renal function should be monitored at the start of therapy. Compounds acting on the renin-angiotensin system, such as telmisartan, may exhibit synergism. When used concomitantly with NSAIDs, a decrease in the effect of antihypertensive drugs such as telmisartan was observed due to inhibition of vasodilation by prostaglandins.
Thus, the results of large-scale clinical studies completed in recent years have shown that angiotensin II receptor blockers (ARBs) meet modern requirements for antihypertensive drugs and are effective and safe for the treatment of patients with arterial hypertension (AH) in various clinical situations (metabolic syndrome, diabetes diabetes, renal dysfunction, etc.). They were included in the first-line drugs for the treatment of hypertension according to the 2010 RMOAG/VNOK recommendations.
Application
Telmisartan-teva should be taken orally once a day with a sufficient amount of liquid, regardless of food intake.
Treatment of hypertension. The recommended dose is 40 mg/day. For some patients, a dose of 20 mg/day will be sufficient. If the blood pressure level does not decrease to the desired levels, then the dose can be increased to a maximum of 80 mg 1 time per day. Telmisartan-Teva can be prescribed in combination with thiazide diuretics, such as hydrochlorothiazide, which exhibit additional blood pressure lowering effects when administered together with telmisartan. When deciding whether to increase the dose, it should be borne in mind that the maximum hypotensive effect occurs 4–8 weeks from the start of treatment.
Prevention of cardiovascular diseases. The recommended dose is 80 mg 1 time per day. It is unknown whether the 80 mg dose of telmisartan is effective in reducing cardiovascular morbidity.
At the beginning of treatment with telmisartan, in order to reduce the risk of cardiovascular diseases, careful monitoring of blood pressure is recommended. It may be necessary to appropriately adjust the regimen of drugs that lower blood pressure.
Renal dysfunction. In patients with mild or moderate renal failure, there is no need for dose adjustment. There is limited experience with use in patients with renal failure or hemodialysis. For these patients, the recommended low starting dose is 20 mg.
Liver dysfunction. For patients with mild to moderate liver dysfunction, the dose should not exceed 40 mg/day. The drug is contraindicated in patients with severe liver dysfunction.
Elderly patients. No dose adjustment is required.
Academpharm
Pharmacodynamics
Telmisartan is a specific angiotensin II receptor antagonist (AT1 type), effective when taken orally. Telmisartan displaces angiotensin II from the AT1 receptor binding site, which is responsible for the known mechanisms of action of angiotensin, and exhibits very high affinity for this site. Telmisartan does not demonstrate partial agonism at the AT1 receptor. Telmisartan selectively and long-lastingly binds to the AT1 receptor. Telmisartan has no affinity for other receptors, including AT2 and other less studied angiotensin receptors. The functional role of these receptors is unknown, as is the effect of their possible excessive stimulation by angiotensin II, the concentration of which increases with the administration of telmisartan. Telmisartan reduces plasma aldosterone levels, does not inhibit human plasma renin, and does not block ion channels. Telmisartan does not inhibit angiotensin-converting enzyme (kininase II), an enzyme that breaks down bradykinin. Therefore, an increase in bradykinin-mediated side effects is not expected.
In humans, an 80 mg dose of telmisartan almost completely suppresses the increase in blood pressure caused by angiotensin II. The inhibitory effect persists for 24 hours and remains significant for up to 48 hours.
Clinical efficacy and safety
Treatment of essential arterial hypertension
After taking the first dose of telmisartan, the onset of antihypertensive action is observed within 3 hours. The greatest reduction in blood pressure is usually achieved 4-8 weeks after the start of treatment and persists with long-term treatment.
The antihypertensive effect persists continuously for 24 hours after dosing, including 4 hours before the next dose, as shown by ambulatory blood pressure measurements. This is confirmed by the ratio of maximum and minimum drug levels, which exceeded 80% after taking 40 and 80 mg of telmisartan in placebo-controlled clinical studies. There was a clear tendency for the time to return systolic blood pressure (SBP) to baseline to depend on the dose taken. Data for diastolic blood pressure (DBP) did not show such a clear relationship.
In patients with arterial hypertension, telmisartan reduces SBP and DBP without affecting pulse rate. The contribution of the diuretic and natriuretic effect to the antihypertensive activity of the drug has not yet been determined. The antihypertensive effectiveness of telmisartan is comparable to that of other classes of antihypertensive drugs (shown in clinical studies comparing telmisartan with amlodipine, atenolol, enalapril, hydrochlorothiazide and lisinopril).
After abrupt cessation of treatment with telmisartan, blood pressure gradually (over several days) returns to its original level without the development of withdrawal syndrome.
The incidence of dry cough was significantly lower in patients treated with telmisartan compared with patients treated with angiotensin-converting enzyme inhibitors in clinical studies directly comparing these two antihypertensive therapy regimens.
Prevention of cardiovascular events
The clinical trial compared the effects of telmisartan, ramipril, and their combination on cardiovascular outcomes in patients over 55 years of age at risk for cardiovascular events. Telmisartan had a similar effect to ramipril for the primary outcome of cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for congestive heart failure. Telmisartan was noninferior to ramipril in the total incidence of cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke.
Patients treated with telmisartan were less likely to develop cough or angioedema compared to patients treated with ramipril. Co-administration of telmisartan and ramipril did not provide additional benefits compared with taking either drug alone. Cardiovascular and all-cause mortality were higher with combination treatment. In addition, the incidence of hyperkalemia, renal failure, hypotension, and syncope was significantly higher in the combination treatment group. Therefore, the use of a combination of telmisartan and ramipril in this population is not recommended.
so that a slight decrease in AUC reduces therapeutic efficacy. There is no linear relationship between the dose taken and the plasma level of telmisartan. When taking doses above 40 mg, there is a disproportionate increase in maximum plasma concentration (Cmax) and, to a lesser extent, AUC.
Distribution
Telmisartan is highly bound to plasma proteins (>99.5%), predominantly to albumin and α-1 acid glycoprotein. The average apparent volume of distribution at equilibrium (Vdss) is about 500 l.
Metabolism
Telmisartan is metabolized by conjugation of the parent compound with a glucuronide. This conjugate has not been shown to have pharmacological activity.
Removal
Telmisartan exhibits biexponential disintegration pharmacokinetics with a terminal half-life of >20 hours. Cmax and, to a lesser extent, AUC increase disproportionately with increasing dose. There are no data on clinically significant accumulation of telmisartan when taken at the recommended dose. Plasma concentrations were higher in women than in men, which did not have a significant effect on the effectiveness of treatment.
Following oral or intravenous administration, telmisartan is excreted almost exclusively in the feces, predominantly as unchanged substance. Total urinary excretion is <1% of the dose taken. The total plasma clearance (Cltot approximately 1000 ml/min) is high compared to the blood flow in the liver (about 1500 ml/min).
Pharmacokinetics in special groups of patients
Influence of gender
Differences in plasma concentrations of telmisartan were noted: in women, Cmax and AUC were, respectively, approximately 3 and 2 times higher than in men.
Elderly patients
The pharmacokinetics of telmisartan in elderly people does not differ from that in patients under 65 years of age.
Renal dysfunction
In patients with mild to moderate renal impairment and severe renal failure, a twofold increase in plasma concentrations was observed. However, lower plasma concentrations were observed in patients with renal failure on hemodialysis. Telmisartan is highly bound to plasma proteins in patients with renal failure and is not excreted during dialysis. The half-life does not change in patients with impaired renal function.
Liver dysfunction
Pharmacokinetic studies in patients with impaired liver function showed an increase in absolute bioavailability of almost 100%. The half-life does not change in patients with impaired liver function.
Contraindications
Hypersensitivity to the active substance or any of the excipients of the drug.
Pregnant women or women planning to become pregnant (see Use during pregnancy or lactation). Obstructive diseases of the bile ducts. Severe liver dysfunction. Children under 18 years of age. The simultaneous use of telmisartan and aliskiren-containing drugs is contraindicated in patients with diabetes mellitus or impaired renal function (glomerular filtration rate 60 ml/min/1.73 m2) (see INTERACTIONS and PHARMACOLOGICAL PROPERTIES).
Telmisartan tablet 80 mg x28
Telmisartan Telmisartan
Compound
Composition per 1 tablet 40 mg: active ingredient - telmisartan - 40.00 mg. Composition per 1 tablet 80 mg: active ingredient - telmisartan - 80.00 mg.
Pharmacotherapeutic group
Angiotensin II receptor antagonist.
ATX code
C09CA07
pharmachologic effect
Telmisartan is a specific angiotensin II receptor antagonist (ARA II) (AT1 type), has a high affinity for the AT1 subtype of angiotensin II receptors, through which the action of angiotensin II is realized. Displaces angiotensin II from its connection with the receptor, without having an agonist effect on this receptor. Telmisartan binds only to the AT1 subtype of angiotensin II receptors. The connection is long-term. It has no affinity for other receptors, including AT2 receptors and other, less studied angiotensin receptors. The functional significance of these receptors, as well as the effect of their possible excessive stimulation by angiotensin II, the concentration of which increases under the influence of telmisartan, have not been studied. Telmisartan reduces the concentration of aldosterone in the blood plasma, does not reduce the activity of renin in the blood plasma and does not block ion channels. Telmisartan does not inhibit angiotensin-converting enzyme (ACE, kininase II), which also catalyzes the degradation of bradykinin. This avoids side effects associated with bradykinin (for example, dry cough). Arterial hypertension: Telmisartan at a dose of 80 mg completely blocks the hypertensive effect of angiotensin II in patients. The onset of antihypertensive action is observed within 3 hours after the first dose of telmisartan. The effect of the drug lasts for 24 hours and remains significant for up to 48 hours. A pronounced antihypertensive effect usually develops after 4-8 weeks of regular use of telmisartan. In patients with arterial hypertension, telmisartan reduces both systolic and diastolic blood pressure (BP) without affecting heart rate (HR). In case of abrupt withdrawal of telmisartan, blood pressure gradually (within several days) returns to initial values without the development of withdrawal syndrome. In comparative clinical studies, it was shown that the antihypertensive effect of telmisartan is comparable to the antihypertensive effect of drugs of other classes (amlodipine, atenolol, enalapril, hydrochlorothiazide and lisinopril). The incidence of dry cough was significantly lower in patients receiving telmisartan compared to those receiving ACE inhibitors. In patients aged 55 years or older with a history of coronary artery disease, stroke, transient ischemic attack, peripheral arterial disease, or complications of type 2 diabetes mellitus (eg, retinopathy, left ventricular hypertrophy, macro- or microalbuminuria) who are at risk for cardiovascular disease -vascular complications. Telmisartan had an effect similar to that of ramipril in reducing the primary composite endpoint of cardiovascular mortality, nonfatal myocardial infarction, nonfatal stroke, or hospitalization due to chronic heart failure. Telmisartan was as effective as ramipril in reducing the secondary endpoints of cardiovascular mortality, nonfatal myocardial infarction, or nonfatal stroke. The effectiveness of reducing the risk of cardiovascular mortality with doses of telmisartan less than 80 mg has not been studied. Dry cough and angioedema were less frequently described with telmisartan compared with ramipril, while arterial hypotension occurred more frequently with telmisartan. The safety and effectiveness of telmisartan in children and adolescents under 18 years of age have not been established.
Indications for use
Reduce cardiovascular morbidity and mortality in patients aged 55 years and older at high risk of cardiovascular disease.
Contraindications
- Hypersensitivity to the active substance or to the auxiliary components of the drug, - pregnancy and breastfeeding, - obstructive diseases of the biliary tract, - severe liver dysfunction (class C according to the Child-Pugh classification), - simultaneous use with aliskiren or aliskiren-containing drugs in patients with diabetes mellitus and/or moderate or severe renal impairment (glomerular filtration rate (GFR) less than 60 ml/min/1.73 m2 body surface area), - simultaneous use with angiotensin-converting enzyme inhibitors in patients with diabetic nephropathy, - lactase deficiency, lactose intolerance, glucose-galactose malabsorption, age up to 18 years (efficacy and safety have not been established).
Method of administration and dosage
Inside, regardless of the time of meal. Arterial hypertension: The initial recommended dose is 1 tablet (40 mg) of Telmisartan once a day. In some patients, taking telmisartan 20 mg per day may be effective. A 20 mg dose can be obtained by splitting a 40 mg tablet in half according to the score. In cases where the therapeutic effect is not achieved, the maximum recommended dose of Telmisartan can be increased to 80 mg once a day. Alternatively, the drug can be taken in combination with thiazide diuretics, for example, hydrochlorothiazide, which, when used together with telmisartan, had additional antihypertensive effects. If it is necessary to increase the dose, it should be taken into account that the maximum antihypertensive effect usually develops 4-8 weeks after the start of treatment (see section “Pharmacodynamics”). Reduction of cardiovascular morbidity and mortality: The recommended dose is 1 tablet of Telmisartan 80 mg once daily. Regular monitoring of blood pressure and, if necessary, dose adjustment of drugs that lower blood pressure are recommended. Special groups of patients For patients with mild to moderate renal impairment, no dose adjustment is required. Experience with telmisartan in patients with severe renal impairment or patients on hemodialysis is limited. A lower initial dose of 20 mg per day is recommended for these patients (see section "Special Instructions"). Liver failure In patients with mild to moderate liver dysfunction (Child-Pugh class A and B, respectively), the daily dose of Telmisartan should not exceed 40 mg. In patients with severe liver dysfunction (class C according to the Child-Pugh classification), the use of the drug is contraindicated (see section “Contraindications”). For elderly patients, no dose adjustment is required.
Release form
Tablets 40 mg and 80 mg. 5, 7, 10 or 20 tablets in a blister pack made of polyvinyl chloride film and printed varnished aluminum foil. 10, 20, 28, 30, 40, 50 or 100 tablets in polyethylene terephthalate jars for medicines, sealed with screw-on lids with first opening control or a “push-turn” system made of polypropylene or polyethylene or polypropylene jars for medicines, sealed with lids pull-on with tamper-evident control made of polyethylene or polypropylene jars for medicines, sealed with tamper-evident pull-on lids made of high-density polyethylene. One can or 1, 2, 3, 4, 5, 8 or 10 blister packs along with instructions for use are placed in a cardboard package (pack).
Terms of release from pharmacies
Dispensed by prescription.
Side effects
Serious adverse events, including anaphylactic reactions and angioedema, are possible in isolated cases, and acute renal failure has also been observed.
Infectious diseases and infestations: infectious diseases of the upper respiratory tract (including pharyngitis and sinusitis), infectious diseases of the urinary tract (including cystitis), sepsis (including fatal ones)1.
Disorders of the blood and lymphatic system: anemia, thrombocytopenia, eosinophilia.
Immune system disorders: hypersensitivity, anaphylactic reactions.
Metabolism disorders: hyperkalemia, hypoglycemia (in patients with diabetes mellitus).
Mental disorders: depression, insomnia, anxiety.
Neurological disorders: fainting, drowsiness.
Visual disorders: visual impairment.
Disorders of the hearing and vestibular apparatus: vertigo.
Cardiovascular system disorders: bradycardia, tachycardia, arterial hypotension2, orthostatic hypotension.
Disorders of the respiratory system, chest and mediastinal organs: shortness of breath, cough, interstitial lung disease.
Cases of interstitial lung disease have been reported transiently with telmisartan during post-marketing surveillance. However, a causal relationship has not been established.
Digestive system disorders: abdominal pain, diarrhea, dyspepsia, flatulence, vomiting, stomach discomfort, dry mouth, dysgeusia.
Hepatobiliary system disorders: liver dysfunction/liver function disorders. Patients of Japanese nationality have been reported to be more susceptible to these adverse reactions.
Skin and subcutaneous tissue disorders: hyperhidrosis, itching, rash, erythema, angioedema (including fatal), drug-induced dermatitis, toxic dermatitis, eczema, urticaria.
Musculoskeletal and connective tissue disorders: myalgia, back pain (eg sciatica), muscle cramps, arthralgia, limb pain, tendon pain (tendinitis-like symptoms).
Disorders of the urinary system: renal dysfunction, including acute renal failure.
General disorders: chest pain, asthenia (weakness), flu-like symptoms.
Laboratory indicators: increased level of creatinine in the blood, increased level of uric acid in the blood, increased level of liver enzymes, increased level of CPK in the blood, decreased level of hemoglobin.
Description of selected adverse reactions
Sepsis. It was reported that patients receiving telmisartan had a higher incidence of sepsis compared to those receiving placebo. This could be either an accident or a sign of a process, the essence of which is still unknown.
Hypotension. This adverse reaction was noted frequently in patients with controlled blood pressure who were treated with telmisartan to reduce cardiovascular disease in addition to standard therapy.
Liver dysfunction/liver disorders. According to post-marketing data, the majority of cases of liver dysfunction/hepatic disorders were observed in patients of Japanese nationality. Patients of Japanese nationality are more susceptible to these adverse reactions.
Interstitial lung disease. Cases of interstitial lung disease have been observed transiently with telmisartan during post-marketing surveillance. However, a causal relationship has not been established.
1 An increased incidence of sepsis has been reported with telmisartan compared with placebo. This phenomenon may be a coincidental occurrence or associated with a mechanism whose operation is currently unknown.
2Reported to occur frequently in patients with controlled blood pressure treated with telmisartan to reduce cardiovascular morbidity in addition to standard therapy.
special instructions
Pregnancy. During pregnancy, treatment with angiotensin II receptor antagonists should not be started. If continuation of therapy cannot be considered essential for a patient who is planning a pregnancy, she should switch to alternative antihypertensive therapy that has an established safety profile for use during pregnancy. If pregnancy is established, treatment with angiotensin II receptor antagonists should be stopped immediately and, if necessary, alternative treatment should be started (see contraindications and use during pregnancy or lactation).
Liver failure. Telmisartan-Teva should not be used in patients with cholestasis, obstructive diseases of the biliary system and severe liver failure, since telmisartan is mainly excreted in the bile. In patients with these diseases, the hepatic clearance of telmisartan is reduced. Telmisartan-Teva should be used with caution in patients with mild to moderate hepatic impairment.
Renovascular hypertension. There is a risk of severe hypotension and renal failure in patients with bilateral renal artery stenosis or renal artery stenosis of a solitary kidney when treated with drugs that affect the renin-angiotensin-aldosterone system.
Kidney failure and kidney transplantation. When using the drug in patients with impaired renal function, it is recommended to periodically monitor the level of potassium and creatinine in the blood plasma. There is no experience with the use of the drug in patients after kidney transplantation.
Decreased intravascular fluid volume. Symptomatic arterial hypotension, especially after the first dose of the drug, may occur in patients with reduced blood volume or hyponatremia, which resulted from intensive diuretic therapy, a salt-restricted diet, or diarrhea and vomiting. Such conditions should be corrected before using the drug. Before starting treatment, it is necessary to normalize sodium levels and intravascular fluid volume.
Double blockade of the renin-angiotensin-aldosterone system. There is evidence that concomitant use of ACE inhibitors, angiotensin II receptor blockers or aliskiren increases the risk of hypotension, hyperkalemia and reduces renal function (including acute renal failure).
Therefore, dual blockade of the renin-angiotensin-aldosterone system when adding an ACE inhibitor to an angiotensin II receptor antagonist is not recommended. If a double block is considered absolutely necessary, it should only be done under specialist supervision and subject to continuous close monitoring of renal function, electrolytes and blood pressure.
ACE inhibitors and angiotensin II receptor blockers should not be used concomitantly in patients with diabetic nephropathy.
Other conditions accompanied by stimulation of the renin-angiotensin-aldosterone system. In patients whose vascular tone and renal function are largely dependent on the activity of the renin-angiotensin-aldosterone system (for example, patients with severe congestive heart failure or significant kidney disease, including renal artery stenosis), treatment with drugs that also affect this system , can cause acute arterial hypotension, hyperazotemia, oliguria, or less commonly, acute renal failure.
Primary aldosteronism. Typically, patients with primary aldosteronism do not respond to antihypertensive drugs that suppress the renin-angiotensin system, so prescribing telmisartan to patients with this condition is not recommended.
Stenosis of the mitral and aortic valves, obstructive hypertrophic cardiomyopathy. As with the use of other vasodilators, the drug should be prescribed with caution to patients with mitral and aortic stenosis or obstructive hypertrophic cardiomyopathy.
Hyperkalemia. The use of drugs that affect the renin-angiotensin-aldosterone system can cause hyperkalemia. In elderly patients, patients with renal failure, patients with diabetes, patients concomitantly receiving other drugs that can increase potassium levels, and/or patients with intercurrent illnesses, hyperkalemia can be fatal.
Before concomitant use of drugs that suppress the renin-angiotensin-aldosterone system, the benefit-risk ratio should be assessed.
The main risk factors for hyperkalemia to consider are:
- diabetes mellitus, renal failure, age (70 years);
- combination with one or more drugs that affect the renin-angiotensin-aldosterone system and/or with nutritional supplements containing potassium. Drugs or therapeutic classes of drugs that may precipitate hyperkalemia include potassium-containing salt substitutes, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor antagonists, NSAIDs (including selective COX-2 inhibitors), heparin, immunosuppressants (cyclosporine or tacrolimus), and trimethoprim;
- intercurrent manifestations, in particular dehydration, acute cardiac decompensation, metabolic acidosis, impaired renal function, unexpected deterioration of the kidneys (for example, infectious diseases), cell lysis (for example, acute limb ischemia, rhabdomyolysis, severe trauma).
Careful monitoring of plasma potassium is recommended in patients at risk.
Sorbitol. The drug contains sorbitol (E420), so it should not be prescribed to patients with hereditary fructose intolerance.
Ethnic differences. Telmisartan and other angiotensin receptor blockers have been found to be less effective in lowering blood pressure in blacks than in other races, possibly because renin levels in blacks with hypertension are lower than in other races. .
Other. As with the use of other antihypertensive drugs, an excessive decrease in blood pressure in patients with coronary artery disease and ischemic cardiopathy can lead to the development of myocardial infarction or stroke.
Diabetic patients who are treated with insulin or hypoglycemic drugs. Hypoglycemia may occur in patients receiving insulin or antidiabetic drugs. In these patients, it is necessary to monitor blood glucose levels, and this should also be taken into account when adjusting the dose of insulin or antidiabetic agents.
In patients with diabetes mellitus, cardiovascular risks (patients with diabetes mellitus, concomitant coronary artery disease), the risk of fatal myocardial infarction and sudden cardiovascular death may be higher when treated with antihypertensive drugs such as angiotensin II receptor antagonists and ACE inhibitors. In patients with diabetes mellitus, the course of concomitant coronary artery diseases may be asymptomatic and therefore they may be undiagnosed. Patients with diabetes mellitus should be carefully evaluated, such as stress testing, to identify and treat concomitant coronary artery disease before prescribing the drug.
Use during pregnancy or breastfeeding
Pregnancy. The drug is contraindicated for use in pregnant women or women planning pregnancy. If pregnancy is confirmed during treatment with the drug, its use should be stopped immediately and, if necessary, replaced with another drug approved for use in pregnant women.
There is insufficient data on the use of telmisartan in pregnant women.
The epidemiological basis for the risk of teratogenicity resulting from the use of ACE inhibitors in the first trimester of pregnancy has not been convincing, but a slight increase in risk cannot be ruled out. Although there are no controlled epidemiological data on the risk of teratogenicity with angiotensin II receptor antagonists, similar risks may exist for this class of drugs. When planning pregnancy, you should replace the drug in advance with another antihypertensive drug with an established safety profile for use during pregnancy. If pregnancy is established, treatment with angiotensin II receptor antagonists should be discontinued immediately and alternative treatment initiated if necessary.
It is known that the use of angiotensin II receptor antagonists in the second and third trimester of pregnancy causes fetotoxicity in humans (impaired renal function, oligohydramnios, delayed formation of cranial bones) and neonatal toxicity (renal failure, hypotension, hyperkalemia). If the use of angiotensin II receptor antagonists began in the second trimester of pregnancy, it is recommended to perform an ultrasound examination of the function of the fetal kidneys and skull bones. The condition of newborns whose mothers took angiotensin II receptor antagonists should be carefully monitored for the presence of arterial hypotension.
Lactation. Since there is no information regarding the use of telmisartan during breastfeeding, its use is not recommended and alternative treatments with established safety profiles should be used during breastfeeding, especially in newborns or premature infants.
Fertility. Preclinical studies did not reveal the effect of telmisartan on the fertility of men and women.
Children. The effectiveness and safety of the drug in children under 18 years of age have not been studied.
The ability to influence reaction speed when driving vehicles or working with other mechanisms. When using antihypertensive therapy, dizziness or drowsiness may sometimes occur. Therefore, if you need to drive vehicles or work with other mechanisms, this should be taken into account.
Telmisartan (Telmesteine)
Before starting and during treatment with Telmisartan, monitoring of blood pressure, renal function, and potassium levels in the blood serum is necessary. Transient arterial hypotension is not a contraindication for further treatment with Telmisartan after stabilization of blood pressure. If severe arterial hypotension reoccurs, the dose should be reduced or the drug discontinued. In the presence of renal failure, treatment is carried out with caution under the control of serum creatinine concentration.
Liver failure
Telmisartan should not be used in patients with cholestasis, biliary obstruction or severe hepatic impairment (Child-Pugh class C) (see section "Contraindications"), since telmisartan is mainly excreted in the bile. It is assumed that in such patients the hepatic clearance of telmisartan is reduced. Telmisartan should be used with extreme caution in patients with mild or moderate hepatic impairment (Child-Pugh class A and B).
Renovascular hypertension
When treated with drugs acting on the RAAS, the risk of severe arterial hypotension and renal failure increases in patients with bilateral renal artery stenosis and stenosis of the artery of a solitary kidney.
Kidney failure and kidney transplantation
When using Telmisartan in patients with impaired renal function, periodic monitoring of potassium levels and creatinine concentrations in the blood serum is recommended. There is no clinical experience with the use of Telmisartan in patients who have recently undergone kidney transplantation.
Decrease in circulating blood volume (CBV)
In patients with a decrease in blood volume and/or sodium content due to previous diuretic therapy, restriction of salt intake, diarrhea or vomiting, symptomatic arterial hypotension may occur, especially after the first dose of Telmisartan. Fluid and/or sodium deficiency must be corrected before starting Telmisartan.
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
The following consequences of RAAS inhibition have been noted: the occurrence of arterial hypotension, fainting, hyperkalemia and impaired renal function (including acute renal failure) in predisposed patients, especially when used in combination with drugs that also act on this system. Dual blockade of the RAAS, for example by adding an ACE inhibitor to an ARA II, is not recommended for patients with already controlled blood pressure and should be limited to selected cases with enhanced monitoring of renal function (including periodic monitoring of potassium levels and plasma creatinine concentrations).
Other diseases characterized by activation of the RAAS
In patients whose vascular tone and renal function depend primarily on the activity of the RAAS (for example, patients with chronic heart failure or kidney disease, including renal artery stenosis), the use of drugs acting on this system, such as telmisartan, has been associated with the occurrence of acute arterial hypotension, hyperazotemia, oliguria, or rarely - acute renal failure (see section "Side effects").
Primary hyperaldosteronism
Patients with primary hyperaldosteronism generally do not respond to treatment with antihypertensive drugs that act by inhibiting the RAAS. In this regard, the use of Telmisartan in these cases is not recommended.
Aortic and mitral valve stenosis
,
hypertrophic obstructive cardiomyopathy (HOCM)
As with other vasodilators, for patients with aortic and mitral stenosis or HOCM
special precautions are indicated.
Hyperkalemia
The use of drugs acting on the RAAS can cause hyperkalemia.
For elderly patients, patients with renal failure, patients with diabetes mellitus and also with arterial hypertension and coronary artery disease (CHD), patients receiving concomitant therapy with drugs that may cause an increase in potassium levels, and/or patients with concomitant disease, hyperkalemia can be fatal. Before considering the possibility of concomitant use of drugs acting on the RAAS, it is necessary to assess the benefit-risk ratio.
The main risk factors to consider are:
— Diabetes mellitus, renal failure, age (patients over 70 years old).
- Combination with one or more drugs acting on the RAAS and/or increasing serum potassium levels. Drugs or therapeutic classes of drugs that may cause hyperkalemia include potassium-containing salt substitutes, potassium-sparing diuretics, ACE inhibitors, ARB II, NSAIDs including selective COX-2 inhibitors, heparin, immunosuppressants (cyclosporine or tacrolimus) and trimethoprim .
- Intercurrent diseases, especially dehydration, acute heart failure, metabolic acidosis, impaired renal function, acute deterioration of kidney condition (for example, infectious diseases), cytolysis syndrome (for example, acute limb ischemia, rhabdomyolysis, severe trauma).
For patients at risk, regular monitoring of serum potassium levels is recommended (see section “Interaction with other drugs”).
In patients with diabetes mellitus and additional cardiovascular risk, for example, in patients with diabetes mellitus and coronary artery disease, the risk of fatal myocardial infarction and sudden cardiovascular death may be increased when taking antihypertensive agents such as ARBAs or ACE inhibitors.
In patients with diabetes mellitus, CAD may be asymptomatic and therefore may not be diagnosed. In patients with diabetes mellitus, before starting the use of Telmisartan, appropriate diagnostic studies, including exercise testing, should be carried out to identify and treat coronary artery disease.
Alternatively, Telmisartan can be used in combination with thiazide diuretics, such as hydrochlorothiazide, which have an additional antihypertensive effect.
Racial differences
As noted for ACE inhibitors, telmisartan and other ARBs appear to be less effective in lowering blood pressure in blacks than in other races, possibly due to a greater predisposition to decreased renin activity in the black diabetic population. and also with arterial hypertension and coronary artery disease.
Other
As with other antihypertensive drugs, an excessive decrease in blood pressure in patients with ischemic cardiomyopathy or coronary artery disease can lead to the development of myocardial infarction or stroke.
Interactions
Digoxin. with simultaneous use of telmisartan and digoxin, an average increase in digoxin Cmax in blood plasma (by 49%) and minimum concentrations (by 20%) was noted. At the beginning of treatment, in case of dose adjustment and discontinuation of telmisartan, digoxin levels should be monitored to maintain them within the therapeutic range.
Like other drugs that affect the renin-angiotensin-aldosterone system, telmisartan can cause hyperkalemia. This risk may increase when combined with other drugs that may also cause hyperkalemia (potassium-containing salt substitutes, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor antagonists, NSAIDs (including selective COX-2 inhibitors), heparin, immunosuppressants (cyclosporine or tacrolimus) and trimethoprim).
The incidence of hyperkalemia depends on associated risk factors. The risk increases with the use of the therapeutic combinations mentioned above. This risk is especially high when combined with potassium-sparing diuretics and salt substitutes containing potassium. Combination, for example, with ACE inhibitors or NSAIDs creates a lower risk if strict caution is observed during use.
Concomitant use is not recommended
With potassium-sparing diuretics or nutritional supplements containing potassium. Angiotensin II receptor antagonists, such as telmisartan, reduce potassium loss caused by diuretics. Potassium-sparing diuretics such as spironolactone, eplerenone, triamterene or amiloride, potassium-containing dietary supplements, or potassium-containing salt substitutes may lead to significant increases in plasma potassium levels. If concomitant use is indicated due to diagnosed hypokalemia, these drugs should be used with caution with frequent monitoring of plasma potassium.
With lithium. With simultaneous use of lithium with ACE inhibitors and angiotensin II receptor antagonists, including telmisartan, a reversible increase in plasma lithium concentration and toxicity was observed. If the use of such a combination is necessary, careful monitoring of lithium plasma levels is recommended.
Concomitant use requiring caution
NSAIDs. NSAIDs (eg acetylsalicylic acid in doses intended for the treatment of inflammatory processes, COX-2 inhibitors and non-selective NSAIDs) may reduce the antihypertensive effect of angiotensin II receptor antagonists.
In some patients with impaired renal function (eg, dehydrated patients or elderly patients with impaired renal function), concomitant use of angiotensin II receptor antagonists and COX depressants may lead to a further deterioration of renal function, including possible acute renal failure, which is usually reversible. Therefore, this combination should be used with caution, especially in elderly patients. Patients should receive adequate fluids and should consider monitoring renal function after initiating concomitant treatment and periodically thereafter.
An almost 2.5-fold increase in AUC0-24 and Cmax was reported when used simultaneously with ramipril and ramiprilat. The clinical significance of this report is unknown.
Diuretics (thiazide or loop). Pre-treatment with high doses of diuretics such as furosemide (loop diuretic) and hydrochlorothiazide (thiazide diuretic) may lead to dehydration and the risk of hypotension when starting treatment with telmisartan.
Should be taken into account when used simultaneously
Other antihypertensive drugs. The effect of telmisartan - lowering blood pressure - may be enhanced when used simultaneously with other antihypertensive drugs.
Given the pharmacological properties, it can be expected that drugs such as baclofen, amifostine can cause the hypotensive effects of all antihypertensive drugs, including telmisartan. Orthostatic hypotension may also be worsened by alcohol use, barbiturates, narcotics, or antidepressants.
GCS (systemic use). Decreased antihypertensive effect.
Double blockade of the renin-angiotensin-aldosterone system. It has been demonstrated that double blockade of the renin-angiotensin-aldosterone system with simultaneous use of ACE inhibitors, angiotensin II receptor antagonists or aliskiren is characterized by a higher incidence of adverse reactions such as arterial hypotension, hyperglycemia, decreased renal function (including acute renal failure), compared with using monotherapy.
Overdose
Information on overdose of telmisartan is limited.
The most pronounced symptoms of telmisartan overdose were arterial hypotension and tachycardia; Bradycardia, dizziness, increased plasma creatinine and acute renal failure have also been reported.
Telmisartan is not excreted from the body by hemodialysis. The patient should be closely monitored and receive symptomatic and supportive therapy. Treatment depends on the length of time since the overdose and the severity of symptoms. It is recommended to induce vomiting and/or lavage the stomach. Activated carbon can be used to treat an overdose. Plasma electrolyte and creatinine levels should be monitored frequently. If arterial hypotension occurs, the patient should be placed in a supine position and the balance of fluid and salt in the body should be restored.
Note!
Description of the drug Telmisartan-Teva table. 80mg No. 28 on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use.
Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug). Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.



![Rice. 1. ACCOMPLISH study: the effect of the combination of ACE inhibitor* amlodipine and ACE inhibitor hydrochlorothiazide on the risk of primary endpoint events (CVE) [14]](https://expert35.ru/wp-content/uploads/ris-1-issledovanie-accomplish-vliyanie-kombinacii-iapf-amlodipin-i-iapf-330x140.jpg)