Sign up
+7
Aortic heart disease is a valve lesion that may or may not involve the ascending aorta. Aortic stenosis is characterized by a narrowing of the aorta, which impedes blood flow. With this pathology, the valve functions are disrupted, complications arise, such as thromboembolism, chronic heart failure, strokes, and heart rhythm disturbances.
Causes of development of aortic stenosis
The disease can be congenital or acquired. The congenital form most often makes itself felt before the age of thirty. Acquired stenosis often becomes a consequence of rheumatism and manifests itself in adulthood. Other reasons for the development of stenosis include:
- Infectious form of endocarditis.
- Rheumatism.
- Myocarditis.
- Atherosclerosis.
- Aortic aneurysm.
- Morphan's syndrome and other systemic connective tissue diseases.
- Heart defects that occur after injuries.
- Tumors in the heart area.
Make an appointment with a specialist without queues, at a convenient time
Sign up
+7
Acquired heart defects
They develop throughout life for the following reasons:
- rheumatism ー damage to the connective tissue by one’s own antibodies that are produced against streptococci (develops in some children after scarlet fever or streptococcal tonsillitis);
- bacterial endocarditis - inflammation of the inner lining of the heart, leading to changes in the valves;
- atherosclerosis - deposition of cholesterol plaques in the walls of blood vessels;
- degenerative changes in valves - typical for older people, caused by tissue wear;
- damage to the aorta, valve apparatus due to syphilis and autoimmune diseases.
Features of the disease
Aortic stenosis itself occurs in 2% of all cases of acquired defects; in combination with valve insufficiency, the disorder can occur in almost 23% of cases. If the valve leaflets are inflamed, the tissues thicken and harden, causing the valve opening to narrow over time. Also, the valves can calcify and fuse along the commissures, greatly narrowing the useful area of the opening.
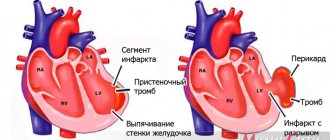
In normal condition, the useful area of the valve opening is from 2.5 to 3.5 square centimeters. If the hole decreases to approximately 0.8-1 cm2, hemodynamic disturbances begin. The critical indicator of the lumen area is 0.5-0.7 cm2. The left ventricle should constantly maintain systolic pressure within 200-250 mmHg. pillar At first, when the valve lumen narrows, the left ventricle compensates for the pathology, making maximum effort, and the person feels normal. Over time, blood begins to accumulate in the cavity, the myocardial fibers stretch, the ventricle begins to contract more actively, and the heart muscle “gets tired” and weakens. The myocardium of the left ventricle becomes hypertrophied, coronary insufficiency develops, and the muscle does not receive the necessary nutrition. Patients suffering from aortic valve stenosis are at high risk of sudden death.
Aortic valve insufficiency is a common companion to stenosis. Excessive pressure in the left ventricle provokes an increase in pressure in the left atrium, and then in the vessels of the pulmonary circulation. The changes primarily affect the connective tissue of the valve. As inflammation increases, the valve leaflets become deformed, their edges thicken, and can turn in and sag. As a result, the valves cannot close tightly, and blood returns to the heart. If the inflammatory process is stopped, valve deformation may continue, for example, due to the formation of scar tissue.
Introduction
Many researchers of sclerodegenerative aortic disease, according to their ideas about its pathophysiology, give different definitions to the disease: “cyanocyanic aortic stenosis”, “Mönckeberg disease”, “calcified aortic valve stenosis of sclerodegenerative origin”, “degenerative defect”, “age-related involution-calcium degeneration of the aortic valve”. valve." These names do not contradict each other, but rather are complementary, however, according to the latest literature data [9, 11, 13, 16, 18, 22], we will call this nosological form of aortic heart disease sclerodegenerative.
As a special form of aortic heart disease in elderly patients, it occurs quite often and by the age of 70 it is the main one [4, 8, 9, 13, 16].
In recent years, the structure of heart valve diseases has changed significantly and sclerodegenerative lesions of the aortic valve apparatus have taken first place in prevalence. The changes in the structure of valvular heart lesions are based on an increase in the life expectancy of the population and a decrease in the incidence of rheumatism [2, 13, 18].
According to the definition of researchers of this problem [8, 10, 12, 13, 16, 20], aortic heart disease of sclerodegenerative etiology can be diagnosed in patients aged 65 years and older who did not suffer from rheumatism, congenital aortic heart disease, or primary infective endocarditis.
Sclerodegenerative aortic valve disease is a fairly common disease. In industrialized countries, aortic valve damage ranks third, second only to coronary heart disease and arterial hypertension [9].
Patients in the older age group often suffer from atherosclerotic coronary disease, requiring myocardial revascularization. At the same time, the aging of the population increases the risk of developing aortic heart disease of sclerodegenerative origin in combination with atherosclerotic lesions of the coronary bed. The combination of aortic heart disease with coronary lesions in this category of patients has long ceased to be exclusive.
It is known that myocardial revascularization in the older age group when correcting aortic valve disease may be required in 45% of patients or even more [3, 6, 7]. The frequency of stenotic lesions of the coronary bed in the group of patients with sclerodegenerative lesions of the aortic valve varies from 35 to 65% [3, 6, 7, 12, 13, 24].
Hospital mortality after intervention on the aortic valve and coronary bed remains quite high and ranges from 5 to 11% [1, 3, 6, 7, 17].
Taking into account the above, we present our own experience of surgical treatment of patients with aortic disease of sclerodegenerative origin and coronary heart disease, and the identified features of the postoperative period.
Material and methods
The study included patients aged 65 years and older who, according to the anamnesis (and intraoperative findings), did not suffer from congenital heart disease, rheumatism, primary infective endocarditis, or who had atherosclerotic lesions of the coronary bed, dictating the need for myocardial revascularization.
At the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky, from 1994 to 2009, 54 patients aged 65 to 88 years (average age 68.4±5.9 years) were operated on for aortic heart disease of sclerodegenerative origin in combination with coronary heart disease.
In total, during this period, 89 patients were operated on for aortic heart disease of sclerodegenerative origin, of which 34 (38.2%) did not require coronary artery bypass grafting, since atherosclerotic lesions of the coronary bed were not diagnosed or there were hemodynamically insignificant stenoses (less than 60% of the vessel diameter ).
The condition of the majority of patients (88.9%) belonged to NYHA functional class (FC) IV. Men predominated - 47 (87%). 2 (3.7%) patients had previously suffered acute myocardial infarction. The mean left ventricular ejection fraction was 51.8±9.3%. The mean systolic gradient between the left ventricle and the aorta was 56.3 ± 27.8 mm Hg.
Clinical manifestations of IHD were observed in 45 (83.3%) patients. Extreme degree of calcification of the aortic valve (III degree according to the classification of the Scientific Center for Cardiovascular Surgery named after A.N. Bakulev, IV degree - according to B.A. Konstantinov) was noted in 48 (88.9%) cases.
Concomitant diseases are presented in the table.
Most often, patients suffered from arterial hypertension, chronic obstructive pulmonary diseases, multifocal atherosclerosis and varicose veins of the lower extremities.
According to the preoperative examination, calcification of the ascending aorta was diagnosed in 18 (33.3%) patients.
Atrial fibrillation upon admission was recorded in 5 (9.3%) patients, one of them had previously been implanted with a permanent pacemaker.
All surgical interventions were performed from a longitudinal median sternotomy in moderate hypothermia (from 28 to 32 °C). Cardioplegic solutions of St. Thomas, Consol, and Custodiol were used.
Aortic valve replacement in combination with coronary bypass surgery was performed in 50 patients. Due to an organic defect of the mitral valve (myxomatous degeneration of the leaflets), as well as widespread calcification with organic damage to the mitral valve, replacement of the mitral and aortic valves was performed in 3 patients. Replacement of the ascending aorta using the Bentall-De Bono technique with coronary bypass grafting was performed in one patient. In one observation, due to hemodynamically severe stenosis of the carotid artery, aortic valve replacement with coronary artery bypass grafting was supplemented with carotid endarterectomy from the left common carotid artery. Plastic surgery of the aortic root with a patch of xenopericardium using the Nix method was performed in 1 patient and in 3 cases it was performed for the purpose of suturing the aortotomy incision after decalcification of the surrounding tissues due to their rigidity.
In total, in 54 observations, 106 distal anastomoses with the coronary bed were formed, thus, the myocardial revascularization index was 1.9. In 19 (35.2%) cases, one coronary artery was bypassed, in 22 (40.7%) - two, in 9 (16.7%) - three, in 4 (7.4%) cases - four. The left internal mammary artery was used in 72.2% of cases. The reasons for refusing to use it were significant stenotic lesions of the left subclavian artery, as well as unsatisfactory blood flow through the artery after its isolation. Proximal anastomoses (n=36) on the clamped aorta were performed in 25 (69.4%) cases, and with lateral compression of the aorta - in 11 (30.6%) cases.
Mechanical prostheses were implanted in the position of the aortic valve in 37 (68.5%) cases, and biological ones in 17 (31.5%) cases.
The average duration of artificial circulation was 104.3±33.1 minutes (56-224 minutes), myocardial anoxia - 80.4±22.1 minutes (49-173 minutes), artificial ventilation - 12.4±7.3 hours (from 7.5 to 46 hours).
Results and discussion
Non-lethal complications (heart failure) were noted in 11 (20.3%) cases. Rhythm and conduction disturbances were recorded in 10 (18.5%) patients: paroxysms of atrial fibrillation - atrial flutter - in 6, transient atrioventricular block requiring temporary cardiac pacing - in 4. In 4 cases, the rhythm was restored with medication, in 2 cases cardioversion was performed. Subsequently, one patient was implanted with a permanent pacemaker system due to the development of sick sinus syndrome.
Respiratory failure requiring prolonged artificial ventilation and/or sessions of the recruiting maneuver “opening the lungs” followed by sessions of non-invasive mask ventilation was observed in 10 (18.5%) cases. Renal failure occurred in 4 (7.4%) patients. In one observation, 3 sessions of ultrahemodiafiltration were performed with complete restoration of renal function.
As for complications from the central nervous system, neurological dysfunction was noted in 5 (9.2%) cases: in 1 - dynamic cerebrovascular accident with complete regression of neurological symptoms even at the hospital stage and the absence of pathological changes according to computed tomography of the brain, in 4 (7.4%) there were signs of encephalopathy (short-term psychomotor agitation or retardation), which required a course of appropriate complex therapy.
It should be noted that out of 25 cases in which distal anastomoses were formed on the clamped aorta, neurological dysfunction occurred in 2 (8%), in a group of 11 patients after lateral compression of the aorta - in 3 (27.3%).
Suppuration of soft tissues was observed in 3 (5.6%) patients, bleeding requiring resternotomy was observed in 1 patient.
Hospital mortality was 3.7% (2 patients). In one observation, after replacement of the aortic and mitral valves and bypass of two arteries, complex conduction and rhythm disturbances developed in the immediate postoperative period, which led to the development of fibrillation and ineffective hemodynamics, which was the cause of death. In another observation, after aortic valve replacement and bypass surgery of two arteries, the cause of death was increasing cardiovascular failure.
Acquired valvular heart defects are the main cause of disability and premature death of patients worldwide [2, 9, 13, 16]. The relevance of the problem of sclerodegenerative aortic stenosis is due to the aging population, the high prevalence of this disease in the elderly, deteriorating quality of life, poor prognosis and high mortality of patients if surgical intervention is not performed [18]. The prevalence of aortic stenosis is 3-7%; among patients 80 years of age and older, its frequency increases to 15-20% [8, 9, 12, 16, 22]. Currently, in developed countries, sclerodegenerative aortic heart disease is the most common heart valve disease and ranks third among all cardiovascular diseases after arterial hypertension and coronary heart disease [11, 14, 16]. Sclerodegenerative aortic stenosis, regardless of severity, leads to an increased risk of myocardial infarction, cerebrovascular accident, heart failure and sudden death [4, 8, 9].
The history of studying sclerodegenerative lesions of the aortic valve dates back to 1904, when J. Monckeberg [19] described 2 observations of stenosis of the aortic mouth with significant calcification of the valves. It has long been believed that calcified aortic stenosis in the elderly is the result of a nonspecific, age-related degenerative process that develops as a result of “age-related wear” of the valve leaflets with passive deposition of calcium on them. This hypothesis has undergone significant changes in the last decade. Currently, epidemiological and experimental data have been obtained that the development of sclerodegenerative aortic stenosis is the result of an active cellular biological process in which lipoproteins accumulate in the valve leaflets, signs of an active inflammatory process, neurohormonal activation and endothelial dysfunction are determined. The active process of calcification leads to the subsequent formation of mature bone tissue in the valve leaflets [8, 9, 18, 20, 21].
Sclerodegenerative aortic stenosis is the result of a genetically determined immune-mediated inflammatory process in the leaflets of the aortic valve, usually leading after 60 years to pathological fibrosis and/or ectopic ossification of the leaflets, in which compaction and calcium weighting of the leaflets cause obstruction of the outflow tract without the primary formation of commissural adhesions [8, 9, 20, 21].
We should not forget that with aortic stenosis, significant hypertrophy of the left ventricular myocardium develops. In this context, work in recent years has forced a new assessment of the role of dysmetabolic processes in the heart muscle [8, 9]. Oxygen in the cardiomyocyte is sequentially used in two processes - β-oxidation of fatty acids and two-stage glycolysis. Under conditions of hypertrophy, oxygen is not enough to carry out the final stages of glycolysis: the oxidative decarboxylation of pyruvic acid is inhibited, which halves the synthesis of ATP and provokes an increased formation of membrane-damaging protons. After the addition of myocardial ischemia, which is an indispensable companion to the disease in question, a reorientation of energy metabolism in cardiomyocytes from glycolysis to β-lipid oxidation is observed, inevitably leading to the development of intracellular lactic acidosis. This process turns out to be key in the development of heart failure in hemodynamically significant aortic stenosis, especially in combination with coronary lesions [8, 9, 12, 13, 15]. That is why the condition of the majority of patients we observed belonged to NYHA FC IV.
The predominance of NYHA FC IV in our observations is explained by the elderly age of the patients, as well as concomitant diseases, among which the dominant role is played by arterial hypertension, chronic obstructive pulmonary diseases, and atherosclerotic lesions of various vascular systems.
There are similarities between vascular atherosclerosis and sclerodegenerative aortic stenosis: common clinical risk factors (age, arterial hypertension, smoking, hyperlipidemia, etc.) [8, 9, 16, 20-22], as well as morphological features (infiltration by macrophages and lymphocytes, deposition lipoproteins, foci of calcification). It is still not uncommon for a diagnosis to be formulated as “atherosclerotic stenosis of the aortic mouth,” but the question of whether the development of sclerodegenerative aortic stenosis in elderly patients is a sign of an atherosclerotic process remains controversial.
It should be noted that, unlike atherosclerosis, there is currently no convincing evidence of a cause-and-effect relationship between clinical factors and calcific aortic valve disease. The relationship between aortic sclerosis and age has been shown to be non-linear, with a clear increase in disease prevalence in men aged around 65 years and in women aged around 75 years [8, 20–22]. In addition, sclerodegenerative aortic stenosis does not develop in all elderly people, while half of the population over 80 years of age does not have characteristic changes in the aortic valve [8, 18, 20].
The association of risk factors for cardiovascular diseases with aortic stenosis is partly explained by the presence of concomitant coronary heart disease in patients with aortic stenosis [1, 3, 6, 7, 12, 13, 15, 20]. Convincing evidence that atherosclerosis and sclerodegenerative aortic stenosis are different diseases is the discrepancy between the severity of damage to the aortic valve and changes in the coronary arteries - only about 40% of patients with aortic stenosis have severe coronary heart disease, and vice versa, most patients with severe coronary artery disease never aortic stenosis does not develop [13].
According to some researchers, the prevalence of coronary heart disease in patients with aortic stenosis and typical angina ranges from 40 to 50%, in the presence of atypical chest pain - 25%, in the absence of chest pain - 20% [3, 6, 7, 18]. Even in patients under 40 years of age with aortic stenosis, without chest pain and without risk factors for coronary heart disease, coronary atherosclerosis is detected in 3-5% of cases, not to mention patients over 65 years of age with sclerodegenerative aortic valve disease [14].
It is known that angina pectoris may not always be an indicator of coronary damage in the presence of aortic stenosis. Only about half of these patients with the classic clinical picture of angina have significant damage to the coronary arteries. In most patients, myocardial ischemia is caused by overload of the left ventricle, which is explained by increased tension of its wall, hypertrophy and changes in microcirculation in the subendothelial layers of the left ventricular myocardium. At the same time, 14% of patients with aortic stenosis have lesions of the left main coronary artery or three-vessel lesions without angina [15]. In our study, lesions of the left main coronary artery or three-vessel lesions without angina pectoris were rare - in 5.6% of cases.
The natural course of aortic stenosis in elderly patients is characterized by a rather long latent period. The clinical picture of the disease manifests itself at the stage of severe damage to the aortic valve. With aortic stenosis, blood flow from the left ventricle to the aorta is hampered, as a result of which the systolic pressure gradient between the left ventricle and the aorta increases significantly. It usually does not exceed 30 mmHg, but can reach 100 mmHg. and more [4, 7, 12, 13, 18, 20]. Due to the increase in afterload of the left ventricle, its hypertrophy develops, which depends on the degree of narrowing of the aortic opening. So, if normally the area of the aortic opening is about 3 cm, then its reduction by half causes a pronounced hemodynamic disturbance. Particularly severe violations occur when the hole area decreases to 0.5 cm2. End-diastolic pressure may remain normal or increase due to impaired relaxation of the left ventricle, which is associated with its severe hypertrophy. Due to the great compensatory capabilities of the hypertrophied left ventricle, cardiac output remains normal for a long time, although during exercise it increases to a lesser extent than in healthy individuals [3, 4, 7, 13].
Clinical manifestations of the disease, in addition to angina, are signs of heart failure and/or often syncope. This signals that the course of the defect is entering a critical period, since after the manifestation of these symptoms, the average life expectancy is 2-3 years. Approximately one third of asymptomatic patients experience sudden death [4, 7, 8, 13, 16].
The incidence of stenotic lesions of the coronary arteries in patients with sclerodegenerative aortic valve disease varies depending on age. Significant damage to the coronary arteries (60% or more of the vessel diameter) is observed in 30-50% of patients, whose average age is 60-70 years. Such a lesion is registered in more than 50% of patients under the age of 75 years and in 41-65% of patients over 75 years of age [3, 7, 15]. According to our data, significant damage to the coronary bed in aortic disease of sclerodegenerative origin was noted in 60.7% of cases.
Statistics indicate that aortic valve insufficiency is less likely to be combined with coronary heart disease, especially compared to aortic stenosis. Among patients who underwent aortic valve replacement, the percentage of patients with aortic insufficiency is relatively small (does not exceed 10-25% of the total number of patients with aortic valve defects and coronary heart disease) [3, 7].
The main feature of aortic valve insufficiency, which essentially determines the entire pathophysiology of this disease, is an increase in the volume load on the left ventricle with its subsequent dilatation. Enlargement of the left ventricular cavity, as a rule, does not occur suddenly. The exception is patients with acute aortic regurgitation, who have severe symptoms associated with a sudden increase in left ventricular end-diastolic pressure and a decrease in effective cardiac output to the peripheral vasculature. At the same time, we must not forget that ischemic dysfunction of the left ventricle can also lead to an increase in its size [3, 4, 11].
The disease in patients with aortic heart disease, including sclerodegenerative origin, and coronary heart disease can occur in one of the following three scenarios [3]:
- aortic valve disease may be asymptomatic and discovered by chance during an examination for symptomatic coronary heart disease;
- without any symptoms, while the presence of a murmur over the aorta, detected during a routine medical examination, prompts additional examination and diagnosis of coronary heart disease;
- the disease may be detected relatively late, when the natural history of aortic valve disease leads to heart failure due to left ventricular overload (pressure or volume) and/or ischemic damage.
The presence of a long latent period, as mentioned above, during which the severity of hemodynamic obstruction of the left ventricular outflow tract gradually increases, makes it difficult to diagnose this disease in the early stages. Thus, at the outpatient stage, only every third patient with stenosis is diagnosed with calcified aortic valve stenosis of degenerative origin. The difficulty of diagnosis is also due to the low specificity of symptoms and their blurred nature in older people. In addition, the presence of other associated conditions, such as coronary heart disease, chronic heart failure, arterial hypertension, and their prevalence in elderly people make it difficult to correctly interpret echocardiographic data [9].
Overall hospital mortality during surgical treatment of combined lesions of the aortic valve and coronary bed ranges from 4.3-5.7% [14, 23] to 11-10.6% [6, 7]. Even balloon coronary angioplasty with stenting followed by aortic valve replacement does not allow achieving a hospital mortality rate below 8.3-7.8% [3, 7]. In our study, the mortality rate was 3.7%.
Since the group of patients we observed falls under the World Health Organization definition of “elderly and senile” age (65 years and older), there are features that must be taken into account during treatment [5]: the presence of concomitant diseases of organs and systems, decreased strength characteristics and elasticity tissues, extreme degree of calcification of the valve apparatus/annulus fibrosus, long-term restoration of muscle tone in the early postoperative period, long recovery period after surgery, delayed tissue repair.
This explains the fact that the average duration of mechanical ventilation in the early postoperative period was 12.4 hours. Often, due to the spread of calcifications to the aortic wall, mitral valve, or the formation of an aneurysm of the ascending aorta, it was necessary to expand the scope of surgical treatment: decalcification of surrounding tissues and the mitral valve, plastic surgery aortic root with xenopericardium or synthetic patch, replacement of the ascending aorta, which increases the duration of artificial circulation and myocardial anoxia.
Thus, in Russia, little attention has been paid to the study of aortic defect of sclerodegenerative origin in combination with coronary heart disease, which means that the practicing physician is not focused on the appropriate diagnostic search. At the same time, the rather rare diagnosis of atherosclerotic stenosis of the aortic mouth due to a lack of understanding of the true nature of the defect leads to the fact that the patient is more often prescribed a diet and cholesterol-lowering drugs than referred for a consultation with a cardiac surgeon. Such “pathogenetic treatment” only leads to the progression of petrified stenosis, which increases the risk of sudden death. Conservative symptomatic tactics in patients with aortic stenosis are generally ineffective, and even more so in patients with calcified aortic stenosis, not to mention the presence of hemodynamically significant lesions of the coronary bed.
In other words, refusal to interpret sclerodegenerative calcified stenosis of the aortic mouth as “atherosclerotic” will lead Russian cardiologists and therapists to form a completely definite view of the treatment prospects for such patients. Surgical treatment is recognized as the only effective treatment worldwide: aortic valve replacement (as a method with the best long-term survival rates) in combination with myocardial revascularization for ischemic disease or the use of balloon valvuloplasty.
In this report, we presented our small experience in the surgical treatment of aortic disease of sclerodegenerative origin in combination with coronary heart disease, however, we believe that the low hospital mortality rate, as well as the small number of complications, give reason to recommend a more aggressive approach when determining indications for surgical treatment of this severe group patients.
Of course, the question of the possibility of large-scale surgical intervention in elderly patients with aortic valve disease in combination with coronary heart disease is very relevant at the present time. The risk of peri- and postoperative complications increases with age, the severity of hemodynamic disorders, as well as the volume of surgical intervention, therefore the decision to perform surgical treatment in each specific observation must be made taking into account the individual risk, benefit and prospects for improving the quality of life in the future.
Symptoms of aortic valve stenosis
Stenosis that is in the compensation stage may not manifest itself at all. The patient's general condition may remain normal or satisfactory. The first manifestation is shortness of breath after any activity, severe fatigue, and weakness. Over time, attacks of angina pectoris, fainting, shortness of breath, a feeling of heaviness in the right hypochondrium, and swelling throughout the body appear. One of the severe manifestations of stenosis is pulmonary edema.
- Available: doctor’s appointment from 1500 rubles
- Convenient: open daily from 8:00 to 21:00
- Quickly: we will carry out all the diagnostics at the first appointment
- Complete: has all the necessary equipment
Heart defects in children
Congenital PS, depending on the severity, can manifest themselves in the first 3 years of a child’s life. Sometimes they are detected already in adulthood. The following signs indicate their possible presence:
- blue lips and nasolabial triangle when crying;
- the appearance of a “heart hump” - a bulge of the chest in the projection of the heart;
- shortness of breath, cough without signs of inflammatory diseases of the respiratory tract;
- delayed physical and mental development;
- the appearance of the “drumsticks” symptom.
Children with such manifestations should be shown to a pediatrician or pediatric cardiologist.
In the children's department, medical appointments are conducted by doctors who have undergone special training to identify health problems in children and infants, taking into account all age-related characteristics.
How is the diagnosis carried out?
At an appointment with a cardiologist, the patient is interviewed, physically examined, lifestyle and possible genetic predisposition to diseases are assessed. To exclude other pathologies of the cardiovascular system, differential diagnosis is used. Instrumental methods include:
- Electrocardiography, electrocardiogram.
- ECG.
- Echocardiography.
- Probing of the heart.
- Aortography.
- Coronary angiography.
- Ventriculography.
- Phonocardiography.
Treatment
Patients with stenosis must be monitored by a cardiologist. Patients in this category should take antibacterial drugs before any interventions and invasive procedures for preventive purposes to prevent the development of inflammation (for example, before visiting the dentist). Also, drug treatment involves controlling blood pressure and stabilizing it.
Surgical treatment has several indications:
- Septic embolism.
- Suppuration on the valve.
- Third degree of reverse blood flow.
- A valve infection that cannot be treated.
- Heart failure with congestion.
Surgical treatment means removing the diseased valve and replacing it with an artificial one. The valve can be mechanical or biological. The main differences of the biological valve:
- Three months after its installation, anticoagulant therapy is not required.
- The prosthesis is as close to natural as possible.
- Unlike a mechanical prosthesis, the valve does not make clicks.
- The biological valve is less durable; degenerative changes can be observed already in the second year of operation with a total service life of 10 years.
A mechanical valve is installed for life; its only disadvantage is the need to constantly take anticoagulants (blood thinners).
Prices for services
| Name | Time | Price | |
| Appointment with a cardiologist, treatment and diagnostic, primary, outpatient | 1500 | ||
| Treatment and diagnostic appointment with a cardiologist, repeated, outpatient | 1000 | ||
| Preventive, outpatient appointment with a cardiologist | 550 | ||
| Comprehensive consultation with a cardiologist ECG with interpretation + Echo-kg | 3650 | ||
| Call a doctor to your home (Khimki, Starbeevo, Ivakino, Naberezhnye) | 15000 | ||
| Calling a doctor to your home (Skhodnya, Podrezkovo, Novopodrezkovo, Planernaya station, Firsanovka) | 15000 | ||
| Call a doctor to your home (Kurkino, Novogorsk) | 15000 | ||
| Call a doctor to your home (Left Bank, Moscow, within the Moscow Ring Road) | 15000 | ||
| Medical consultation | 3300 | ||
| Extract from outpatient card | 660 | ||
| Consultation (interpretation) with analyzes from third parties | 1300 | ||
| Consultation on treatment adjustments | 550 | ||
| Repeated reception of CMN | 1600 | ||
| Initial reception of CMN | 2000 | ||
| Express test for determining the level of Troponin in the blood. | 1900 | ||
| Expand all prices | |||
Mechanical prostheses.
At the Republican Scientific and Practical Center, two modifications of bicuspid artificial heart valves have been developed and are used in the clinic: PLANIX-T and PLANIX-E. The difference between the design of the latest version of the domestic bicuspid artificial heart valve and the previous model is that the body of the prosthesis is coated with titanium oxide, which ensures high wear resistance and biological inertness. The high height of the rotating mechanism prevents jamming of the valves by heart tissue and made it possible to increase the opening angle of the valves to 900.