Congenital heart defects are estimated to occur in approximately 1% of newborns.
Their development is usually determined by a number of concomitant genetic and environmental factors. Congenital heart failure is a relatively common cause of death in newborns and infants. According to data, about 50% of children diagnosed with heart disease die before the first year of life. However, all existing heart defects can be treated with surgical procedures.
General information about the disease
Asphyxia is diagnosed in 4-6% of children. Moreover, the percentage varies depending on the degree of prematurity of the fetus. In babies born before 36 weeks, the incidence of pathology reaches 9%, and in children born after 37 weeks it decreases to 1-2%.
Scientific definitions of newborn asphyxia boil down to the fact that the child cannot breathe independently or makes superficial convulsive breathing movements that do not allow the body to receive sufficient oxygen. The authors consider infant asphyxia as suffocation, in which other signs that the fetus is alive remain: there is a heartbeat, the umbilical cord is pulsating, the muscles are weak but contracting.
The reasons for the development of newborn asphyxia include a complex of risk factors that disrupt the blood circulation and respiratory functions of the fetus in the womb and during birth. The most common reasons include:
- conflict of Rh blood between mother and child;
- abnormal fetal development;
- pathologies of the nervous system in a baby;
- circulatory disorders, heart disease in the baby;
- intracranial injury that the baby received during the birth process;
- infections affecting the fetus in the womb (chlamydia, herpes, rubella, etc.);
- extragenital pathologies of the mother (thyrotoxicosis, anemia, diabetes mellitus);
- infectious diseases in the second and third trimesters;
- complicated childbirth;
- premature or post-term pregnancy;
- bad habits of the mother (effects of alcohol, nicotine, drugs on the body);
- malnutrition during pregnancySource: Asphyxia of newborns. Zhetpisova L.B. West Kazakhstan Medical Journal, 2011.
The most common cause of asphyxia is intrauterine hypoxia, that is, the baby lacks oxygen in the womb.
Whatever the causes of the pathological condition, it causes the same processes in the child:
- disrupts metabolism and blood circulation;
- thickens and increases blood viscosity;
- damage is caused to the brain, liver, heart, adrenal glands;
- organs swell, bleeding occurs;
- disruptions in the functioning of the central nervous system occur.
The longer the body feels a lack of oxygen, the more serious the degree of damage to tissues, organs and systems becomes.
Types of Congenital Heart Defects
Congenital heart defects are most common in premature babies with low birth weight. The immediate causes of violations in the design of this organ are not fully understood. The coexistence of at least several genetic and environmental factors has a major influence on the occurrence of heart defects. The risk of their occurrence in a child increases when:
- A woman suffered from rubella in the first trimester of pregnancy.
- The pregnant woman smoked cigarettes, drank alcohol, or used drugs.
- Woman with diabetes.
- The child developed chromosomal abnormalities (including Down syndrome and Turner syndrome).
Heart defects can affect various structures of the organ, including the valves, ventricles, and blood vessels. Taking this into account it stands out:
- Defects in the parts of the heart.
- Abnormal abnormalities in large arteries.
- Improper blood flow to the heart.
- Partial or total stenosis of valves and blood vessels.
Main signs and symptoms
The most obvious diagnostic sign is respiratory distress. It is this that subsequently leads to disruption of the cardiovascular system, weakening of the child’s muscle tone and reflexes.
Clinical manifestations of moderate asphyxia:
- lethargy, weakness;
- decreased motor activity;
- weak reactions;
- depressed reflexes;
- low-emotional cry;
- tachycardia;
- arrhythmic breathing, sometimes with wheezing;
- the skin is bluish, but can quickly turn pink.
The child's condition is considered moderate. During the first 2-3 days of life, he is in a state of increased excitability, which can be replaced by a syndrome of depression, weakness, and lethargy. The condition manifests itself as small tremors of the arms and legs, disturbed sleep, and weak reflexes.
In severe asphyxia, the clinical picture includes:
- lack of cry at birth;
- reflexes are severely depressed or sharply reduced;
- the skin is bluish, pale, with a “marble pattern”;
- breathing is shallow, arrhythmic and periodically absent;
- wheezing is heard in the lungs;
- the heartbeat is weak, dull;
- convulsions.
If acute severe asphyxia is successfully overcome, breathing normalizes within 2-3 days and reflexes are restored. Source: Fetal hypoxia and asphyxia of the newborn. Kuznetsov P.A., Kozlov P.V. General Medicine, 2021. p. 9-15.
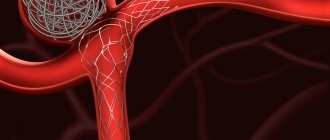
Narrowing of the aorta
Aortic stenosis occurs in approximately 8% of newborns with diagnosed heart disease. Given the location of the partial occlusion of the main artery, narrowing is observed:
The subvalve, which is a narrowing of the blood flow path from the left ventricle, is located below the aortic valve. The consequence of this disease is pressure overload, which leads to ventricular hypertrophy. With this heart defect, the following has been identified: coronary heart disease at an early age, severe arrhythmias, primarily ventricular, which can cause loss of consciousness or obstructive aortic stenosis, usually asymptomatic until adolescence, when there is chest pain with frequent fainting. A narrowing of the aorta that is not diagnosed at the right time can lead to serious complications, including valve damage.
Valvular aortic stenosis, which is characterized by partial closure of the lumen of the main artery at the level of the valve. This defect leads to rapidly progressing heart failure, accompanied by pulmonary edema. For this reason, the child requires immediate surgical intervention.
Types of newborn asphyxia
Classification is carried out according to several criteria. First of all, depending on the time of development of the pathological condition, the following are distinguished:
- primary, or intrauterine asphyxia - develops directly in the womb;
- secondary, or extrauterine asphyxia – occurs in the first hours of the baby’s life.
In turn, primary asphyxia is also divided into two subtypes:
- antenatal, or chronic - develops even before the onset of labor;
- intrapartum, or acute - occurs during the period of uterine dilation and fetal birth.
Classification of asphyxia according to the Apgar scale
To assess the severity of asphyxia in a newborn, the Apgar scale is used. With its help, the doctor evaluates heart rate, breathing, muscle tone, skin color and reflexes, and then determines the severity of the pathological condition.
To give a rating, the doctor evaluates each of the five signs as 0, 1 or 2 points. Accordingly, the maximum and best score is 10 points. The assessment is determined taking into account the following criteria:
| Sign | 0 points | 1 point | 2 points |
| Pulse, beats per minute | No | Up to 100 | From 100 and above |
| Breath | No | Irregular, weak | Active, child screams and cries |
| Muscle tone | Arms and legs dangling | Weak flexion of arms and legs | Active movements |
| Reflexes | No | Weak | Present, well expressed |
| Color of the skin | Pale, cyanotic | Body – pink, arms and legs – bluish | Pink body, limbs |
The condition is assessed in the first and fifth minutes of life. Accordingly, the child receives two ratings: for example, 8/10. If the score is 7 or lower, the baby’s condition is assessed additionally at the 10th, 15th and 20th minutes.
Depending on the Apgar score, the degree of asphyxia is determined:
- 1-3 points – heavy;
- 4-5 points – average;
- 6-7 points – mild or moderate.
The Apgar score is not highly sensitive. Therefore, if a child has abnormalities, additional diagnostics are necessary to assess asphyxia.
Symptoms
- Blue or cyanotic color of the skin, lips, ears.
- The appearance of bluish skin during breastfeeding or the baby’s cry.
- Pallor of the skin and coldness of the extremities (with “pale defects”).
- Heart murmurs.
- Signs of heart failure.
- Changes in the electrocardiogram, x-rays, echocardiographic examination (ultrasound of the heart).
Of course, with such symptoms, concerned parents immediately consult a doctor, and the heart defect is diagnosed in the first months of the child’s life, or at birth during the accompanying first examinations. Small defects sometimes manifest themselves only as unusual heart murmurs when heard during regular examinations by a pediatrician.
Even with a congenital heart defect, for some time after birth a child may look quite healthy in appearance during the first ten years of life. However, later the heart defect begins to manifest itself: the child lags behind in physical development, shortness of breath appears during physical exertion, pallor or even cyanosis of the skin.
To establish a true diagnosis, a comprehensive examination of the heart is necessary using modern high-tech equipment.
Surgical treatment is the most effective, and operations are often performed on newborns and children from the first year of life. Most often, the question of surgical treatment is raised even before the birth of the child, if it concerns “blue defects”. Therefore, in such cases, childbirth should take place in maternity hospitals at cardiac surgery hospitals. Therapeutic treatment is necessary if the timing of the operation can be postponed to a later date. If the question concerns “pale defects,” then treatment will depend on how the defect behaves as the child grows. Most likely, all treatment will be therapeutic.
Diagnostics
Asphyxia can be diagnosed during gestation (primary, or intrauterine) by:
- monitoring of fetal heart rate, which is carried out during cardiotocography;
- analysis of motor activity, breathing and muscle tone of the fetus, which is carried out during ultrasound examination.
In case of secondary or extrauterine asphyxia, the diagnosis is made taking into account the presence of signs of a pathological condition, the external condition of the baby, the severity of the lack of oxygen and further tests that are carried out after completing the emergency care algorithm for the child.
For diagnosis use:
- Apgar score;
- a blood test from the scalp, vessels of the fetal umbilical cord, during which the oxygen tension, carbon dioxide tension and blood acidity are determined.
In some cases, an ultrasound examination of the brain is also prescribed, which determines how much the central nervous system is affected. The examination also makes it possible to distinguish hypoxic damage to the nervous system from traumatic one.
Diagnosis of acquired and congenital heart defects
The basis for diagnosing both congenital and acquired heart defects is echocardiography (ECHO), which is a visual examination that allows for non-invasive examination of the structures of the heart - valves, chambers, atria and blood vessels. The most common type is transthoracic echocardiography. Contraindications for this test are obesity (BMI over 35), chronic obstructive pulmonary disease (COPD). Another test used in diagnosing acquired and congenital heart defects is a chest x-ray (X-ray), which can accurately determine the location, size and shape of the heart. It is important to note that the most popular cardiac examination, electrocardiography (ECG), cannot be the main examination for suspected heart disease.
Treatment
Clinical recommendations for asphyxia include the provision of first aid to the newborn as a priority. This is the most important step, which, if carried out competently, reduces the severity of the consequences of the pathological condition and the risk of complications. The key goal of resuscitation measures for asphyxia is to achieve the highest possible Apgar score by 5-20 minutes of the newborn’s life.
The stages and principles of ABC resuscitation allow for consistent and effective resuscitation of a newborn born with asphyxia. Source: Carrying out therapeutic hypothermia in newborns born with asphyxia. K. B. Zhubanysheva, Z. D. Beisembaeva, R. A. Maykupova, T. Sh. Mustafazade. Science of Life and Health, 2021. p. 60-67:
- Principle A (“airway”) is to ensure a clear airway during the first stage of resuscitation. To do this, you need to create the correct position: tilt your head back, lower it 15 degrees. After this, suck out mucus and amniotic fluid from the nose, mouth, trachea, and lower respiratory tract.
- Principle B (“breath”) – create ventilation, provide breathing. To do this, a jet oxygen flow is created - artificial ventilation of the lungs is performed using a resuscitation bag. If the child does not cry, tactile stimulation is added: stroking along the back, patting the feet.
- Principle C (“cordial”) – restore heart function. Indirect cardiac massage helps with this. If necessary, adrenaline, glucose, hydrocortisone and other drugs are administered. In this case, the auxiliary ventilation from the previous stage cannot be stopped.
Care for a newborn child who has suffered asphyxia is carried out in a maternity hospital. Babies with a mild form are placed in a special tent with a high oxygen content. In cases of moderate or severe asphyxia, infants are placed in an incubator - a special box where oxygen is supplied. If necessary, the airways are re-cleaned and freed from mucus.
The scheme of further treatment, recovery and care is determined by the attending physician. General care recommendations include:
- maintaining normal body temperature, blood pressure, heart rate;
- creating maximum comfort: optimal ambient temperature, comfortable position;
- carrying out respiratory therapy;
- conducting infusion therapy - administering fluid to meet needs Source: Protocol for therapeutic hypothermia for children born with asphyxia. Ionov O.V., Balashova E.N., Kirtbaya A.R., Antonov A.G., Miroshnik E.V., Degtyarev D.N. Neonatology: News. Opinions. Training, 2014. p. 81-83.
During rehabilitation, regular monitoring :
- baby's weight (twice a day);
- neurological and somatic status;
- volume of fluid consumed;
- nutrition composition;
- basic vital signs: pulse, blood pressure, saturation, respiratory rate;
- laboratory characteristics of blood, urine;
- X-rays of the chest, abdominal cavity;
- ultrasound examination of the abdominal cavity;
- neurosonography;
- electrocardiograms, echocardiograms.
After discharge, the baby should be regularly monitored by a pediatrician or neurologist.
Coarctation of the aorta (CoAo) is a congenital narrowing of the aorta, most often located just distal to the left subclavian artery near the ductus arteriosus (ligamentum arteriosus). The prevalence of coarctation is 0.2-0.6 per 1000 live births, the frequency is 5-8% among all congenital heart defects [1, 2]. This anomaly is often combined with other heart defects: patent ductus arteriosus, bicuspid aortic valve, ventricular septal defect (VSD), mitral valve anomaly as a component of Schon’s syndrome, etc. [3].
In 1903, L. Bonnet [4] proposed dividing patients with aortic coarctation into two types: juvenile and adult. Juvenile later became known as “preductal coarctation” and adult as “postductal” [5]. Important factors determining hemodynamic severity are the patency of the duct, the diameter of the arch, and the degree of obstruction at the site of coarctation. To evaluate the results, the classification of aortic coarctation proposed by the International Nomenclature and Database Conferences for Pediatric Cardiac Surgery is used: isolated; with VSD; with other complex cardiac anomalies, as well as a combination of these three types with isthmus hypoplasia and/or arch hypoplasia [6].
Embryology
There are two independent embryological theories that explain the occurrence of aortic coarctation: the flow theory and the ductal loop theory. Flow theory is based on the hypothesis that the flow of blood through the cardiac chambers and great vessels during the embryonic period often determines their size at birth [7]. When blood flow through the right side increases due to an intracardial shunt (VSD), blood flow through the left side and, consequently, across the isthmus correspondingly decreases. Similarly, left side obstruction (eg, mitral or aortic stenosis) reduces blood flow in the ascending aorta and isthmus. Thus, this theory is based on reduced flow across the isthmus in the prenatal period. Intracardiac defects that may cause coarctation according to the flow theory are clinically commonly associated in patients with coarctation. These defects include VSD, bicuspid aortic valve, and congenital aortic or mitral valve stenosis [3]. P. Venugopalan et al. [8] in their studies proved that with coarctation of the aorta, the size of the mitral valve is significantly smaller than in the control group. Minor hemodynamic disturbances in the embryonic circulation lead to a decrease in flow through the aortic arch [9]. The role of the limbus oval window is the deviation of the corresponding portion of blood from the inferior vena cava into the ascending aorta. Early narrowing of the oval window or abnormal angle of the limbus can lead to varying degrees of hypoplasia of the left heart structures. This may explain the development of Shawn syndrome [10]. This theory is confirmed by the fact that in case of defects with decreased blood flow through the right sections (tetralogy of Fallot, pulmonary stenosis, tricuspid atresia), coarctation of the aorta almost never occurs [7].
However, the flow theory is not very convincing in the absence of obvious intracardiac defects. In such a situation, the “ductal loop” theory is more acceptable. More than 100 years ago, J. Skoda [11] postulated that abnormal advancement of ductal tissue into the aorta is a significant factor in the pathogenesis of aortic coarctation. Later, during microscopy, it was seen that the circular ridge, which creates obstruction during coarctation, consists of similar cells found in the ductus arteriosus [12]. Compression and fibrosis of this “ductal loop” during ductal closure results in narrowing of the aorta and the occurrence of coarctation. This may explain the occurrence of coarctation of the aorta in the absence of concomitant intracardiac anomalies.
Other researchers have put forward alternative ideas that may also explain the occurrence of coarctation. A. Kappetein et al. [13] believe that an anomaly in the development of the neural crest plays a role in the pathogenesis of aortic coarctation. Genetic factors cannot be excluded, given the frequent occurrence of coarctation in women with Turner syndrome [14].
Pathophysiology
Patients with coarctation of the aorta are divided into two groups. The first group is newborns with juvenile coarctation, in whom the blood supply to the lower half of the body depends on the patent ductus arteriosus (PDA). If the disease is not diagnosed in time (i.e. before the duct closes), then they develop cardiogenic shock. In infancy, collaterals are not developed, and ischemia of organs below the site of coarctation after closure of the PDA leads to the development of renal failure and acidosis. At the same time, increased afterload on the left ventricle causes acute congestive heart failure. Preoperative management of these patients has been facilitated by the initiation of prostaglandin E1 (PGE1), which opens and maintains the ductus arteriosus open. Prostaglandin infusion was first (1975) successfully used in the treatment of infants with critical blue defects (pulmonary atresia, transposition of the great arteries) and later (1979) began to be used in newborns with interrupted aortic arch and juvenile coarctation [17]. The use of prostaglandin in combination with mechanical ventilation, inotropic support, and bicarbonate administration improves cardiac output, relieves metabolic acidosis and renal failure. Surgical correction must be performed after the patient's condition has stabilized.
Another group includes patients with the “adult” type of coarctation. At first glance, these are “asymptomatic” patients who are accidentally diagnosed with arterial hypertension during examination. As a rule, these are children of the older age group.
Diagnostics
Diagnosis of coarctation in newborns remains a significant problem. It is almost impossible to suspect a defect prenatally. It is difficult to make an accurate diagnosis in a timely manner even after birth. In juvenile coarctation, the wide ductus arteriosus provides adequate blood flow to the descending aorta - in such patients, a distinct pulsation and equal pressure in the arms and legs will be detected in the femoral arteries, and the main blood flow will be recorded by EchoCS in the abdominal aorta. When combined with VSD, there will be no difference in pulse oximetry data between the arms and legs. When the ductus arteriosus is closed, the clinical picture of the disease rapidly develops: cardiogenic shock, multiple organ failure.
Newborns with critical “adult” coarctation are in a state of shock. During examination, the child is pale, tachypnea and tachycardia are noted. There is no pulsation in the femoral arteries. The liver is enlarged, hypotension even in the arms. On the x-ray, the heart is dilated and there are signs of congestive heart failure. The ECG shows overload of the left sections.
In most cases, diagnosis is based on data from two-dimensional echocardiography with color Doppler ultrasound [15, 16]. According to EchoCS, in the “adult” type of coarctation, the absence of main blood flow in the descending aorta is determined, and a narrowing is visible in the isthmus region. In the juvenile type, a wide PDA with flow into the descending aorta is noted. There is a main blood flow in the abdominal aorta. The isthmus and aortic arch are often hypoplastic. Be sure to measure the dimensions of all segments of the aortic arch, and also pay attention to concomitant intracardiac anomalies. This point is especially important, as it can radically change the tactics of further surgical treatment. In most newborns, echocardiography is sufficient to make the diagnosis. In addition to the standard examination, it is advisable to perform a non-invasive study in the form of computed tomography with contrast enhancement of blood vessels [18, 19] (Fig. 1).
Figure 1. CT scan of a newborn with coarctation 3D reconstruction.
In recent years, invasive research has been used extremely rarely, however, if there are complex concomitant intracardiac anomalies, then after stabilization of the patient's condition, probing is performed. During the study, organic changes in blood vessels, hemodynamic parameters and intracardiac anatomy are assessed [9].
Indications for surgical intervention and timing
Juvenile coarctation in a newborn with its ductus-dependent systemic circulation is an absolute indication for emergency intervention. However, if the child is critically ill due to a closed duct, surgery may be delayed to stabilize the patient's condition as quickly as possible. Intensive preoperative therapy for such children consists of infusion of PGE1 and symptomatic correction of homeostasis indicators. The presence of an “adult” type of coarctation in an infant is accompanied by symptoms of congestive heart failure, which also requires immediate surgical treatment.
Correction methods
The first successful correction of coarctation was performed by C. Crafoord and G. Nylin in Sweden in 1944 [20]. Resection of coarctation in an infant was performed by W. Mustard et al. in 1953 [21]. Their technique consisted of creating a direct circular anastomosis (Fig. 2).
Figure 2. Simple end-to-end circular anastomosis (schematic). A start was made in surgical treatment, but long-term results were disappointing due to the high relapse rate. The further development of surgery in this area was reduced to the development and improvement of new anastomosing technologies, namely the exclusion of circular anastomosis and the complete elimination of pathological ductal tissue. In 1961, T. von Rueden et al. [22] proposed an isthmoplasty procedure similar to aortoplasty with a synthetic patch in order to avoid the formation of a circular anastomosis. J. Waldhusen and D. Nahrwold in 1966 [23] proposed an original aortoplasty with a left subclavian artery flap (Fig. 3).
Figure 3. Isthmoplasty with a subclavian artery flap (diagram). This procedure eliminated the circumferential anastomosis but was unable to eliminate the abnormal ductal tissue [24].
In 1977, J. Amato et al. [25] proposed resection of coarctation with the formation of an extended anastomosis (Fig. 4),
Figure 4. Resection of coarctation with the formation of an extended end-to-end anastomosis. in 1987, M. Elliott [26] improved this anastomosis for patients with arch hypoplasia, calling it radically extended. Other innovative methods that have been described by M. Meier et al. [27] and J. De Mendonca et al. [28], include reconstruction with a subclavian flap preserving the left subclavian artery, as well as using a reverse subclavian flap [29].
Combination of coarctation with other anomalies
There is still debate about the stages of correction of coarctation in combination with intracardiac anomalies. In fact, recent studies comparing both approaches demonstrate the superiority of single-stage surgical treatment (assuming the correction is biventricular) [30]. Recently, M. Kobayashi et al. [31] presented a 10-year experience in treating 90 newborns with aortic arch obstruction and associated anomalies. Overall mortality was 4.4-7.8% in different groups, survival rate over 10 years was 87%. To date, indications for treatment in several stages are an infant’s weight less than 1500 g, severe infection, intracranial hemorrhage, multiple organ failure and a very unfavorable anatomical structure [32].
Coarctation in combination with arch hypoplasia
In newborns with coarctation of the aorta, hypoplasia of the aortic arch occurs in 65 to 81% [30, 33]. More often, hypoplasia is present when coarctation is combined with shunt defects or underdevelopment of left heart structures, which confirms the flow theory in the development of coarctation [7].
The arch is conventionally divided into 3 segments: proximal (from the brachycephalic trunk to the left common carotid artery), distal part (from the left common carotid artery to the left subclavian artery) and isthmus. There is a rule according to which the diameter of the proximal part should be more than 60% of the diameter of the ascending aorta, the distal part - more than 50% and the isthmus - more than 40%. However, these indicators are considered insufficiently accurate, especially if there is hypoplasia of the ascending aorta. A formula is described according to which the arch is considered hypoplastic if its transverse diameter in millimeters is less than the patient’s weight, expressed in kilograms plus 1 [34]. The optimal diagnostic criterion for hypoplasia today is to determine the deviation from the mean value (Z) [35]. The arch is hypoplastic if it deviates from the standard value -2Z or more. A common form of hypoplasia is the so-called “bovine trunk”, when the brachycephalic trunk and the left common carotid artery arise as a single trunk, being, as it were, a continuation of the ascending aorta. The distal segment of the arch is a narrow and long lateral branch that passes into the isthmus. The left subclavian artery originates from the distal arch.
There are different opinions regarding the growth of a hypoplastic arch after correction. Some authors believe that the arch will develop after simple resection of coarctation with the formation of a circular end-to-end anastomosis [35], the rate of recoarctation in their study was 12.5%. However, there is evidence of 81% recoarctation in patients with arch hypoplasia after creation of a circular anastomosis [36]. Such data raise doubts regarding the development of the arch in the postoperative period, therefore, techniques have been proposed that eliminate hypoplasia of the arch in the absence of hope for its subsequent development: radically extended end-to-end anastomosis [26], plastic surgery with a reverse flap of the subclavian artery [29]. Some authors also tend to believe that the best long-term results are achieved when reconstructing the arch under conditions of artificial circulation during circulatory arrest [37].
Coarctation of the aorta and hypoplasia of the left heart structures
Coarctation of the aorta is often combined with underdevelopment of various structures of the left heart, including the mitral and aortic valves [38]. When these structures are hypoplastic and on the verge of maintaining systemic circulation, it is difficult to determine the optimal strategy for further treatment. If the left ventricle is too small to maintain systemic circulation, one should go down the path of univentricular correction or transplantation, excluding the possibility of biventricular correction. Several studies have shown that biventricular repair is possible for mitral and aortic valve deviations greater than -2Z. However, these studies focused on early survival [39, 40]. Study
M. Puchalski et al. [41] showed that after correction of KoAo in newborns in combination with hypoplasia of the left heart structures, the dynamics of the left heart structures are observed, as well as an excellent clinical result. Despite the initial annular hypoplasia, the need for interventional repair for mitral or aortic/subaortic stenosis is rare.
Coarctation of the aorta in newborns weighing less than 2 kg
Prematurity and low birth weight of infants with coarctation are not contraindications to surgical treatment. There is an opinion that such patients have a high risk of death and the development of recoarctation [47]. Previously, it was reported that there is a high incidence of hospital mortality (up to 20%) in small children with CoAo [30]. However, progress in intensive care and improvement of surgical techniques have led to good results in recent years. E. Bacha et al. [48] presented the results of treatment of 18 patients weighing less than 2 kg with critical coarctation. Hospital mortality was 5.5%. Analysis of the results of treatment of coarctation in such patients showed no correlation between the development of recoarctation and the patient’s weight at the time of surgery. According to many authoritative experts, residual ductal tissue plays a significant role in the development of recoarctation [49].
Recoarctation
Despite the many developed techniques, the problem of residual coarctation and recoarctation is relevant. Common correction methods include: resection with the formation of a circular anastomosis, aortoplasty with a patch, aortoplasty with a subclavian flap and resection with the creation of an extended anastomosis. The most widely used of these techniques is the subclavian flap aortoplasty technique [23]. Many centers have long abandoned resection with the formation of a circular anastomosis in newborns due to the high rate of recoarctation, reaching, according to some reports, up to 85% [42]. Patch aortoplasty also has a high risk of recoarctation in neonates. The Society of Congenital Heart Surgeons reported a 21% rate of recoarctation among 38 patients less than 1 month of age undergoing patch aortoplasty [43]. There are several disadvantages of subclavian flap aortoplasty, especially when compared with the extended anastomosis technique. This is a deteriorated blood supply to the left extremity, the leaving of ductal tissue, which will later lead to recoarctation through a spur, as well as the inability to cut a flap of sufficient length to bypass the crest of the ductal tissue and preserve the often encountered tubular hypoplasia of the arch. There have been reports of gangrene of the upper extremity after transection of the subclavian artery [44]. Because the coarctation ridge is not resected, rapid growth of remaining ductal tissue, which cannot be adequately assessed intraoperatively, may cause recurrence after subclavian flap repair [45]. The incidence of recoarctation after subclavian flap repair ranges from 12 to 42% [43, 46, 47]. Several centers have presented their results using the extended anastomosis technique, showing lower recoarctation rates ranging from 0 to 23%.
Interventional therapy
The role of balloon dilatation is limited to a narrow spectrum of diseases in this area: recoarctation, coarctation in the form of a membrane in infants in critical condition, coarctation syndrome, which does not occur in newborns.
Non-invasive manometric gradient between arms and legs greater than 20 mm Hg. is considered recoarctation and is an indication for re-intervention. An analysis of articles presenting the results of correction of coarctation in newborns when recoarctation occurs indicates the successful use of balloon dilatation without deaths or complications [46, 50].
Thus, despite the significant accumulated world experience on this problem, a number of debatable issues remain: the optimal method of correction, especially in combination with hypoplasia of the aortic arch; the problem of recoarctation and ways to eliminate it - balloon dilatation or repeated surgery. There is still no consensus on the advantage of one- or two-stage correction when coarctation is combined with other intracardiac anomalies. Pediatric cardiac surgeons, as a rule, do not change stereotypes, provided their own treatment results are good. The answer to these questions is possible after a multicenter analysis of accumulated long-term results using various approaches to solving these problems.
Consequences and complications
The pathology is quite dangerous and is one of the most common causes of child mortality. How favorable the prognosis will be depends on the severity of the baby’s condition and the Apgar indicator. If the score increases, the prognosis is considered favorableSource: Modern methods of treating neonatal asphyxia. Cherednikova E.N., Sherstnev D.G. Bulletin of Medical Internet Conferences, 2021. p.824.
However, with severe pathology, serious complications develop during the first year of life. Early consequences that may appear in the first few days after resuscitation include :
- respiratory arrest (the most common and dangerous complication);
- pulse failure;
- convulsions;
- cerebral edema;
- disruption of the urinary and digestive systems.
Later disorders include the following diagnoses:
- syndrome of increased excitability (hyperexcitability);
- increased intracerebral pressure (hypertension syndrome);
- lesions of the central nervous system (perinatal encephalopathy);
- disruptions in the functioning of the endocrine and vegetative-vascular systems (hypothalamic disorders).
With timely and competent medical intervention, as well as a high-quality recovery period, asphyxia of newborns may not have dangerous consequences in the future. Mild forms of asphyxia have almost no effect on the child; after the illness, his further development will proceed in the same way as in other babies.
Prevention of newborn asphyxia
The expectant mother should be involved in the prevention of the pathological condition during pregnancy. To do this you should:
- attend routine gynecological consultations;
- adhere to the recommendations of the obstetrician-gynecologist;
- be sure to take vitamin complexes if prescribed by a doctor;
- monitor the condition of the fetus and placenta during routine ultrasound examinations;
- treat any diseases only under the supervision of a doctor, do not self-medicate;
- follow a daily routine, do not overload the body;
- get rid of bad habits;
- to walk outside.
In obstetrics, considerable attention is paid to the development of effective preventive methods that can reduce the risk of asphyxia during childbirth and during the first days of a baby’s life.
Sources:
- Modern methods of treating newborn asphyxia. Cherednikova E.N., Sherstnev D.G. Bulletin of Medical Internet Conferences, 2016. p.824
- Protocol for therapeutic hypothermia for children born with asphyxia. Ionov O.V., Balashova E.N., Kirtbaya A.R., Antonov A.G., Miroshnik E.V., Degtyarev D.N. Neonatology: News. Opinions. Training, 2014. p. 81-83
- Carrying out therapeutic hypothermia in newborns born with asphyxia. K. B. Zhubanysheva, Z. D. Beisembaeva, R. A. Maykupova, T. Sh. Mustafazade. Science of Life and Health, 2021. p. 60-67
- Asphyxia of newborns. Zhetpisova L.B. West Kazakhstan Medical Journal, 2011
- Fetal hypoxia and asphyxia of the newborn. Kuznetsov P.A., Kozlov P.V. General Medicine, 2021. p. 9-15
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Prices
| Name of service (price list incomplete) | Price |
| Online opinion of a pediatrician (SPECIAL) | 0 rub. |
| Appointment (examination, consultation) with a pediatrician, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |