Hypertensive crisis is a severe form of arterial hypertension. Can occur at any time. More often observed in women than in men. The cause of the occurrence lies in the disruption of blood pressure regulation. If arterial hypertension is common in 40% of the population, then in only 1% of cases there may be a sudden jump from baseline values, which leads to a sharp deterioration in health with a high risk of death.
What exactly are the symptoms of a hypertensive crisis should be known not only to hypertensive patients, but also to their loved ones. Normal and elevated blood pressure values are individual for each person. When a crisis occurs, signs of impaired cerebral or coronary blood supply are observed.
Symptoms and signs of their manifestation
When a hypertensive crisis occurs, the following symptoms appear:
- nausea, vomiting, suffocation;
- convulsions and loss of consciousness;
- intense headache;
- clouding of consciousness and disturbances in speech and vision;
- heart pain and palpitations;
- trembling, sweating, chills;
- feeling of lack of air;
- Possible loose stools.
Are you experiencing symptoms of a hypertensive crisis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Pathogenesis
Neurohumoral mechanisms of the development of hypertensive crisis are important. Overstimulation of the RAAS initiates a vicious chain reaction that includes vascular damage, tissue ischemia, and further overproduction of renin. The body produces excessive amounts of angiotensin II, catecholamines, vasopressin, aldosterone, endothelin-1, and thromboxane. But there are not enough endogenous vasodilators. Therefore, local regulation of peripheral resistance. If blood pressure gradually increases and reaches an individual limit, endothelial regulation of vascular tone is disrupted.
As a result of hyperperfusion, following endothelial damage, fibrinoid necrosis of arterioles develops, vascular permeability increases, which leads to perivascular edema. An important aspect of clinical manifestations and prognosis is the concomitant activation of platelets and the coagulation system, which, in combination with the loss of fibrinolytic activity by the endothelium, contributes to disseminated intravascular coagulation.
Types of pathology
Types of hypertensive crisis are classified depending on the manifestation of symptoms. Medical care is selected individually according to indications and clinical manifestations. Hypertensive crisis types I and II, complicated and uncomplicated forms are types of pathology. Hyperkinetic crisis or type I is characterized by rapid development. Acute headache and dizziness, nausea, and vomiting occur. The state is close to fainting. Blood pressure rises above 200 mm Hg. Art. (systolic - upper), which is why red spots appear in the face, neck, chest, feeling of heat, tachycardia, moist skin.
Hypokinetic crisis or type II occurs when there is a violation of the treatment regimen or rhythm of life in patients with stage III arterial hypertension. Deterioration in well-being develops more slowly, although the intensity remains noticeable. The severity of the headache increases exponentially. Diastolic (lower) pressure remains in the range of 140-160 mmHg. Art. Symptoms include nausea and vomiting, lethargy, blurred vision and hearing, and a tense pulse.
A complicated hypertensive crisis has several vectors of development, which affects the type of complications. There are such subtypes: coronary, asthmatic, cerebral. Against this background, pulmonary edema or cardiac asthma, acute left ventricular failure may develop. Cerebrovascular accidents, ischemic stroke and other pathologies may occur. An uncomplicated hypertensive crisis requires pressure correction in the next 24 hours, but it has an important nuance - there is no risk of target organ damage.
Diagnostics
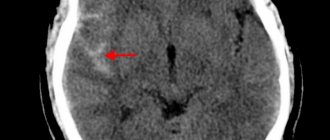
Diagnosis of a hypertensive crisis usually includes urine tests, ECG, and calculation of creatinine and serum urea concentrations. Patients with neurological symptoms require a CT scan of the head to rule out edema, intracranial hemorrhage, or cerebral infarction. Patients who complain of chest pain and shortness of breath are usually ordered to have a chest x-ray. On ECG findings, if target organs are affected, there are signs indicating acute ischemia or hypertrophy of the left ventricle. Negative changes in the results of urine tests are typical in cases where the kidneys are involved in the process. The doctor makes a diagnosis based on excessively high blood pressure numbers, as well as target organ damage.
Preventive measures
The best prevention of a hypertensive crisis is awareness of the peculiarities of the occurrence of attacks, an understanding of how an increase in blood pressure occurs and the causes of this phenomenon.
Timely diagnosis and interaction with a doctor, following medical recommendations is an opportunity to prevent the development of crises of varying degrees. Hypertension can be controlled if:
- avoid drinking alcohol;
- stop smoking;
- reduce salt intake to 5 g per day;
- normalize body weight;
- adhere to antihypertensive therapy;
- reduce stress levels;
- avoid overwork.
Prevention of hypertensive crisis
This is a dangerous condition that can be fatal. It is important to start treatment in a timely manner, to strive to prevent further progression of the disease that caused a sharp increase in blood pressure, following simple recommendations:
- control blood pressure;
- normalize nutrition (follow a regimen, diet);
- maintain normal weight;
- eliminate heavy physical and emotional stress;
- eliminate harmful addictions;
- be examined by a doctor.
Information about the diagnosis and treatment of patients
Regardless of the causes of a hypertensive crisis in a man or woman, diagnosis comes first to determine the further course of treatment. Symptoms may coincide with other pathological conditions. Diagnosis of hypertensive crisis includes the following procedures and studies:
- Analysis of urine;
- ECG, CT, radiography;
- heart rate measurement.
The doctor needs to collect a detailed history of the patient's condition. When the attacks began, the frequency of their occurrence, symptoms, whether the patient receives regular antihypertensive therapy, what methods were used to reduce blood pressure, whether there was experience in independently stopping the crisis, the presence of concomitant diseases - basic information for the doctor during the diagnosis.
Causes
There is currently no consensus on the causes of hypertensive crisis. It is generally accepted that this is a complication of diseases characterized, according to ICD 10, by high blood pressure. Crisis often develops in people suffering from hypertension and less often in people with secondary hypertension, which is a symptom of the following diseases:
- atherosclerosis of the aorta and arteries, especially renal;
- glomerulonephritis;
- pyelonephritis;
- pheochromocytoma;
- Cushing's disease;
- Pelfing's syndrome;
- Page syndrome;
- polyarteritis nodosa;
- nephropathy of pregnancy;
- diabetes;
- systemic lupus erythematosus;
- nephroptosis;
- acute alcoholic arterial hypertension.
Most often, HA develops against the background of pathologies associated with damage to the renal vessels. In this situation, HA is caused more by cerebral edema than by high blood pressure. However, there are significantly fewer such cases than crises caused by hypertension.
During a hypertensive crisis, blood pressure values can reach 220/110 mm. Hg pillar and above
The following factors can provoke HA:
- climate change;
- changes in meteorological conditions;
- air travel;
- psycho-emotional and physical stress: stress, lack of sleep, overwork, high and prolonged physical activity;
- large doses of alcohol;
- smoking;
- discontinuation of antihypertensive drugs;
- eating salt in large quantities;
- endocrine diseases.
Hypertensive crises in children develop, as a rule, against the background of secondary arterial hypertension. Most often these are renal diseases and neurogenic pathologies, less often - hyperthyroidism, pheochromocytoma and others. Adolescents may develop a crisis with primary hypertension.
Treatment and its features
Treatment for a hypertensive crisis is prescribed depending on the medical history and the presence of other conditions in acute form or chronic pathologies (cardiac percussion, auscultation of the heart, lungs, large vessels, hemorrhagic stroke, renal failure, severe myocardial ischemia). At the time of the attack, the patient needs medical attention. It consists of lowering blood pressure.
Afterwards, drug therapy is prescribed. When prescribing drugs, it is important that they act after a maximum of 20-30 minutes, and the effect lasts for at least 4-6 hours. When treating crises, the danger is the occurrence of uncontrollable hypotension. For this reason, self-medication with such a diagnosis carries the risk of drug collapse. Special medical supervision is necessary for patients with a history of concomitant diseases. It is important to understand that with proper treatment of arterial hypertension, crises occur extremely rarely.
How does it manifest?
The most common symptoms of a hypertensive crisis:
- feeling of anxiety;
- fear, anxiety;
- chills;
- trembling of limbs;
- hyperemia;
- swelling of the face;
- decreased vision;
- attack of vomiting;
- neurological disorders;
- with encephalopathy - irritability, euphoria or depression;
- in severe cases - acute pulmonary edema, coma, acute renal failure, arterial thrombosis, azotemia, decreased amount of urine excreted.
Answers to frequently asked questions from patients
How long does a hypertensive crisis last?
On average, an attack lasts about 2-3 hours. Symptoms develop either quickly or progressively, depending on the form of the crisis.
What should not be done during a hypertensive crisis?
You cannot endure and wait for the crisis to pass. It is necessary to carry out first aid measures that involve a gradual decrease in blood pressure. During an attack, the patient should not stand, stand up sharply, bend over, push, or take physical action. When blood pressure decreases, the patient can rest in a horizontal position, but with the head of the bed raised.
What is the hidden danger of a hypertensive crisis?
The consequences of a hypertensive crisis are widespread - stroke, myocardial infarction, disorders of the central nervous system, angina pectoris, and aneurysm. For this reason, hypertension should be monitored by a doctor, and the patient should take antihypertensive drugs regularly.
Consequences
A hypertensive crisis cannot be called a simple sudden sharp increase in blood pressure, accompanied by a headache. GC has a risk of developing many complications from most organs and even systems.
- Disorders of the central nervous system, manifested in confusion or coma (encephalopathy).
- Acute heart failure.
- Brain hemorrhage.
- Pulmonary edema (which results from sudden left ventricular failure).
- Aneurysm.
- Angina pectoris.
- Myocardial infarction.
- Eclampsia, which occurs during pregnancy.
Forecast
The prognosis for an uncomplicated crisis with subsequent continuous maintenance treatment of hypertension is favorable. In a complicated hypertensive crisis, 25-35% of patients die within 4 years either from renal failure or from the consequences of a stroke . Unfavorable prognostic factors are the duration of arterial hypertension , old age, increased serum urea creatinine, hypertensive retinopathy .
Epidemiology
Arterial hypertension has been and remains one of the most common diseases in Russia. About 40% of the adult population of our country suffer from high blood pressure.
Hypertensive crises most often occur with irregular use of antihypertensive drugs. A distinctive feature of the Civil Code is the possibility of its repetition:
- 62.7% of hypertensive crises recur within a year;
- 39.6% - within the next month;
- 11.7% - within 48 hours.