Pulmonary hypertension is a disease characterized by increased pressure in the pulmonary artery system, which can be caused by a significant increase in the volume of pulmonary blood flow or an increase in resistance in the vascular bed of the lungs.
Pulmonary hypertension is almost always a secondary condition. If doctors have not been able to identify the cause, then pulmonary hypertension in this case is considered to be primary. With this type, the pulmonary vessels narrow, their hypertrophy and fibrization occur. Due to pulmonary hypertension, right ventricular overload and failure develop.
- Causes and epidemiology
- Pathogenesis
- Classification
- Symptoms
- Diagnostics
- Treatment
- Forecast
Symptoms include shortness of breath on exertion, fatigue, possible fainting and chest discomfort. Diagnosis is made by measuring pulmonary artery pressure. Treatment is carried out with vasodilators, and in severe cases they resort to a lung transplant. In general, the prognosis is poor for primary pulmonary hypertension, since therapy cannot be carried out to eliminate the underlying pathology.
Normal pulmonary artery pressure readings :
- systolic 23-26 mm Hg.
- diastolic 7-9 mm Hg.
- average 12-15 mm Hg.
According to WHO recommendations, the maximum normal systolic pressure in the pulmonary artery should be 30 mm Hg, and the maximum diastolic pressure should be 15 mm Hg.
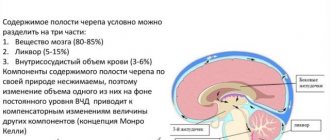
Pathogenesis
Primary PH is characterized by smooth muscle hypertrophy, variable vasoconstriction, and vessel wall remodeling. Vasoconstriction is caused by an increase in the activity of thromboxane and endothelin 1, as well as a decrease in the activity of nitric oxide and prostacyclin. Increased pulmonary vascular pressure is caused by vascular obstruction. It affects endothelial damage.
As a result, coagulation on the intimal surface is activated, which can aggravate arterial hypertension. This is also facilitated by thrombotic coagulopathy, which is a consequence of an increase in the content of plasmogen activator inhibitor type 1 and fibrinopeptide A and a decrease in the activity of tissue plasmogen activator. Focal coagulation on the surface of the endothelium must be distinguished from chronic thromboembolic pulmonary arterial hypertension, which is provoked by organized pulmonary thromboembolism.
As a result, in most patients, primary pulmonary hypertension becomes a provoking factor of right ventricular hypertrophy with dilatation and right ventricular failure.
Classification
Left ventricular failure
- Arterial hypertension
- Myocarditis
- Cardiomyopathies
- Mitral regurgitation
- Coarctation of the aorta, aortic valve defects
- Cardiac ischemia
Increased pressure in the left atrium
- Tumor or thrombosis of the left atrium
- Mitral stenosis
- Supravalvular mitral annulus, triatrial heart
Pulmonary vein obstruction
- Pulmonary venous thrombosis
- Mediastinal fibrosis
Parenchymal lung diseases
- Interstitial lung diseases
- Chronic obstructive pulmonary diseases (COPD)
- Acute severe lung injury (severe diffuse pneumonitis, adult respiratory distress syndrome)
Diseases of the pulmonary artery system
- Repeated or massive pulmonary embolisms
- Primary pulmonary hypertension
- Systemic vasculitis
- Thrombosis "in situ" of the pulmonary artery
- Increased pulmonary blood flow volume (patent ductus arteriosus, congenital heart disease with left-to-right shunting)
- Distal pulmonary stenosis
- Pulmonary hypertension caused by food or drugs
Pulmonary hypertension of newborns
- Hyaline membrane disease
- Persistent fetal circulation
- Meconium aspiration
- Diaphragmatic hernia
Hypoxia and/or hypercapnia
- Obstruction of the upper respiratory tract (obstructive sleep apnea syndrome, enlarged tonsils)
- Accommodation high in the mountains
- Primary alveolar hypoventilation
- Pickwick's syndrome (hypoventilation in fat people)
Many authors classify such forms of pulmonary hypertension as acute and chronic based on the timing of development.
Causes
The main diseases that provoke the development of pulmonary hypertension and cor pulmonale syndrome are chronic lung diseases. Most often these are bronchopulmonary diseases:
- chronic obstructive bronchitis (characterized by changes in lung tissue);
- bronchiectasis (distinguished by the formation of cavities in the lower parts of the lungs);
- fibrosis of lung tissue, which is caused by pathological processes in the parenchyma, etc.
In addition, heart disease may be a cause:
- certain birth defects;
- diseases that impair the functionality of the heart muscle.
Also, periodic thrombosis of the pulmonary artery vessels is also often the cause of the development of the syndrome. There are several main pathways in the development of the disease:
- alveolar hypoxia (lack of oxygen);
- changes in the structure of lung tissue;
- increase in the number of red blood cells.
There are other factors that can cause pulmonary hypertension:
- certain medications, toxins;
- medical and demographic factors (gender, condition, presence of diseases).
The development of pulmonary hypertension can be triggered by the presence of the following diseases:
- HIV infection;
- cirrhosis of the liver;
- blood diseases;
- portal hypertension;
- hyperthyroidism;
- some hereditary diseases;
- compression of the blood vessels of the lungs (by a tumor, a changed chest or as a result of obesity);
- physical activity, especially lifting in height.
Symptoms
The first clinical manifestations occur when there is a more than twofold increase in blood pressure in the pulmonary artery. The main symptoms are almost identical for pulmonary hypertension of any etiology. Main complaints:
- increased fatigue and weakness in the body
- shortness of breath (appears at the very beginning of the disease), first during physical activity, later at rest
- persistent pain in the heart area (caused by relative coronary insufficiency)
- fainting (due to a lack of oxygen in the human brain, typical for the primary form of the disease in question)
- pain in the liver and swelling in the feet and legs
- Hoarseness of voice (rare)
- hemoptysis (often, especially with a significant increase in pressure in the pulmonary artery)
The vast majority of cases are characterized by rapid fatigue and progressive shortness of breath during exertion. With shortness of breath, there may be atypical discomfort in the chest, and during physical activity, dizziness and even faintness are common. Such manifestations are mainly explained by insufficient cardiac output. Raynaud's phenomenon occurs in approximately 10 cases out of 100 with primary pulmonary hypertension, and 99% of such cases occur in women. A symptom such as hemoptysis is rarely noted; it most often signals a future death. Rarely, dysphonia occurs due to compression of the recurrent laryngeal nerve by the enlarged pulmonary artery (Ortner's syndrome).
In advanced cases, pulmonary hypertension can manifest itself with the following symptoms:
- diffuse second tone (S2) with an emphasized pulmonary component S (P)
- right ventricular bulge
- third sound of the right ventricle (S3)
- pulmonary ejection click
- swelling of the jugular veins
- peripheral edema
- congestion in the liver
Portopulmonary hypertension
This is severe pulmonary arterial hypertension with portal hypertension in patients without secondary causes. Pulmonary hypertension is observed in patients with various conditions that lead to portal hypertension without or with cirrhosis. Portopulmonary hypertension is less common compared to hepatopulmonary syndrome in people with chronic liver diseases; according to statistics, this is from 3.5 to 12% of cases.
The first signs to appear are increased fatigue and shortness of breath. ECG and physical examination methods reveal manifestations characteristic of PH. Regurgitation is often recorded at the tricuspid valve. This diagnosis is suspected upon receipt of EchoCG data, confirmation is carried out using catheterization of the right heart. Treatment requires elimination of primary pulmonary hypertension without prescribing hepatotoxic drugs. In some cases, the doctor resorts to vasodilator therapy. The outcome depends on the underlying liver disease.
Portopulmonary hypertension is a relatively contraindication to liver transplantation, since there is a high risk of complications and death for the patient. After transplantation, in some cases with moderate pulmonary hypertension, the disease reverses.
Symptoms of pulmonary valve insufficiency
The pathology is well tolerated by patients. Dozens of years pass from the development of the defect to the first symptoms.
Most patients with severe regurgitation requiring surgical correction are children. They were born with valve insufficiency and underwent balloon valvuloplasty for pulmonary stenosis or surgical correction of tetralogy of Fallot. After valvotomy, the first symptoms appear only after 30 years. After surgery for tetralogy of Fallot, they may occur earlier due to initial hypertrophy of the right ventricle (one of the components of tetralogy of Fallot).
Regurgitation itself does not cause any symptoms. They develop only with the development of right ventricular heart failure. The first manifestation is deterioration in exercise tolerance.
As the pathology progresses, other symptoms arise:
- dyspnea;
- interruptions in heart function;
- in severe cases - enlarged liver, edema, swelling of the neck veins.
Diagnostics
Objective examination reveals cyanosis. Developing for a long time without treatment, the disease leads to the fact that the distal phalanges of the fingers take on the appearance of “drumsticks”, and the nails take on the shape of “watch glasses”. Auscultation of the heart reveals typical signs: accent (maybe splitting) of the second tone over a.pulmonalis; systolic murmur over the area of the xiphoid process, increasing with inspiration. At the peak of the development of the disease, there may be a diastolic murmur in the second intercostal space on the left, which is explained by the relative insufficiency of the pulmonary valve with its strong expansion.
Cardiac percussion does not reveal signs typical of pulmonary hypertension, and therefore is not considered an effective diagnostic method in these cases. Rarely, an expansion of the border of vascular dullness in the second intercostal space on the left and a displacement of the right border of the heart outward from the right parasternal line are recorded (which is explained by hypertrophy of the right ventricular myocardium). With pulmonary hypertension, hypertrophy of the pancreas and right atrium is usually found, as well as signs that indicate an increase in pressure in the pulmonary artery.
To detect these signs, resort to the following methods:
- ECG,
- X-ray of chest organs,
- catheterization of the right heart with measurement of pressure in the right atrium, right ventricle, and in the trunk of the pulmonary artery
- EchoCG
To detect the causes of the disease, other methods are used :
- CT lungs
- X-ray tomography of the lungs
- angiopulmonography
- ventilation-perfusion radionuclide scintigraphy of the lungs
The above methods help to detect pathology of the parenchyma and vascular system of the lungs. In some cases, diagnosis is also carried out using a lung biopsy to detect pulmonary veno-occlusive disease, diffuse interstitial lung diseases, pulmonary capillary granulomatosis, etc.
Among the symptoms of PH, there may be hypertensive crises in the pulmonary artery system , which are manifested by the following symptoms:
- severe cough, sputum may contain blood
- severe suffocation (mainly in the evening/night hours)
- pronounced general cyanosis
- orthopnea (severe shortness of breath associated with stagnation in the pulmonary circulation)
- fast and weak pulse
- excitement (not always)
- bulging of the conus a.pulmonalis
- pronounced pulsation of a.pulmonalis in the 2nd intercostal space
- accent of the second tone on a.pulmonalis
- pulsation of the right ventricle in the epigastrium
- the appearance of vegetative reactions in the form of urina spastica, involuntary defecation after the end of the crisis
- swelling and pulsation of the neck veins
- appearance of the Plesch reflex
Primary pulmonary hypertension is suspected if the patient has severe dyspnea on exertion and there is no history of other diseases that could lead to PH. First, a chest X-ray, ECG, and spirometry are done to look for the most common causes of shortness of breath. After this, Doppler echocardiography is used to measure pressure in the right ventricle and pulmonary arteries and detect possible anatomical abnormalities that may be the cause of secondary PH.
In primary pulmonary hypertension, radiographs often reveal expansion of the roots of the lungs with a pronounced narrowing towards the periphery. Spirometric indicators and lung volumes may be normal or moderately limited. But the diffusivity of carbon monoxide (DL) is usually below normal. The ECG shows such general changes as include deviation of the electrical axis to the right, R > S in V; SQ T and peak P waves.
To detect secondary causes that cannot be determined by symptoms, the doctor prescribes additional tests. This includes perfusion-ventilation scanning to detect thromboembolic disease; pulmonary function tests (makes it possible to detect restrictive or obstructive pulmonary diseases); serological tests (to rule out or confirm rheumatic disease).
Chronic thromboembolic pulmonary arterial hypertension can be suggested by appropriate findings on computed tomography or pulmonary scans and is diagnosed by arteriography. If necessary, these methods are also used:
- polysomnography
- liver function tests
- HIV test
If the initial examination does not reveal conditions associated with secondary PH, the doctor performs a pulmonary artery catheterization. This measures pressure in the right side of the heart and pulmonary artery, pulmonary capillary wedge pressure, and cardiac output. To exclude atrial septal defect, blood O2 saturation in the right side is measured.
During the procedure, vasodilating drugs are often used (intravenous epoprostenol, adenosine, inhaled nitric oxide, etc.). If the body responds to the administration of the above-mentioned drugs by reducing the pressure in the right side, this indicates that such a drug will be effective in treating the condition. Previously, a biopsy was often used, but today doctors do not advise resorting to this method due to the large number of possible complications and the high percentage of deaths.
If a diagnosis of primary pulmonary hypertension is made, the patient's family history should be examined to detect possible genetic transmission (as indicated by cases of premature death of relatively healthy family members). For familial primary pulmonary hypertension, genetic counseling should be consulted to inform family members of the risk of the disease (approximately 20%). They are recommended to undergo echocardiography for evaluation. Testing for mutations in the BMPR2 gene in familial primary pulmonary hypertension may be of value in the future.
Treatment of pulmonary valve insufficiency
For the first time in the world, V.I. corrected pulmonary valve insufficiency. Burakovsky. He performed prosthetics - implanted a Golikov tricuspid petal valve into the pulmonary position. 1966 D. N. Fuller et al. reported successful implantation of a pulmonary allograft in a 15-year-old girl.
In the 70s and 80s, such operations were practically not carried out. At that time, the prevailing opinion was that valve disease was not dangerous and had virtually no effect on hemodynamics. Accordingly, there is no point in correcting it. But at the end of the twentieth century, it became clear that after surgical correction of tetralogy of Fallot, dysfunction of the outflow tract of the right ventricle develops in the long term. Many patients require pulmonary valve replacement to avoid developing heart failure.
In recent years, surgical techniques for correcting tetralogy of Fallot have been improved, and valve-sparing techniques have emerged. But in some cases it is impossible to avoid transannular repair, so the incidence of valvular insufficiency after surgery remains high.
Another medical procedure that can cause pulmonary regurgitation is balloon valvuloplasty. It is done for stenosis (narrowing) of the valve. The doctor inserts a balloon, inflates it and widens the hole. The stenosis disappears, but some patients develop valvular insufficiency instead.
Thus, although surgery and minimally invasive procedures are not the most common cause of pulmonary valve insufficiency, it is medical interventions that lead to severe regurgitation requiring surgical correction. Since the end of the twentieth century, such operations have been carried out more and more often. Bioprostheses are installed in the pulmonary position, which do not allow blood to flow in the opposite direction.
In the 21st century, transcatheter methods for implanting artificial valves appeared. They avoid open heart surgery. However, not all patients are candidates for such interventions. They are performed mainly in case of dysfunction of a previously installed bioprosthesis and in some patients after surgical correction of tetralogy of Fallot.
Drug therapy
Drug treatment is symptomatic only. It reduces the symptoms of heart failure. Conservative therapy is used to prepare for surgery - to stabilize the patient's condition and reduce surgical risks.
Valve replacement
Pulmonary valve reconstruction is not performed. In case of insufficiency, prosthetics is performed - installation of an artificial bioprosthesis, which will ensure blood flow in only one direction.
The timing of the operation is a constant subject of debate. On the one hand, the operation should be performed as late as possible. This is due to the fact that only biological prostheses are placed in the pulmonary position. Mechanical too often cause thrombotic complications, even with constant use of anticoagulants. But bioprostheses have a limited service life. Sooner or later the valve will have to be replaced. Accordingly, the later the operation is performed, the later the next surgical intervention will be required, and the fewer operations the patient should undergo during his life. On the other hand, even in the absence of symptoms, right ventricular function gradually deteriorates due to regurgitation. Moreover, this deterioration may be irreversible. From this point of view, intervention should be performed as early as possible in order to preserve the right ventricle.
Indications for surgical treatment differ in different guidelines. Possible indications for surgery:
- end-diastolic volume of the right ventricle more than 160 ml/m2;
- the ratio of right and left ventricular end-diastolic volume is 1.5 in the presence of symptoms and 2 in the absence of symptoms;
- the appearance of symptoms of right ventricular failure (some doctors consider it necessary to perform surgery, even if symptoms are detected only using stress tests);
- rapid progression of dilatation (expansion) of the right ventricle, even if its volume does not reach values considered indications for surgical correction of the defect.
Open heart surgery is required to install the prosthesis. In adult patients with right ventricular dilatation, two valve replacements may be required as they develop relative tricuspid regurgitation.
Minimally invasive prosthetics
Typically, patients prefer minimally invasive treatment to surgical treatment if possible. For pulmonary regurgitation, doctors use a transcatheter prosthetic method: a bioprosthesis is delivered through blood vessels. In this case, no incisions are needed on the chest, and a heart-lung machine is not used. Surgical risks are much lower, and there is no long recovery period after surgery.
Stent valves are used in Europe and can be implanted without major surgery. They are used for:
- repeated prosthetics - installation of a new valve over the old one, if the first prosthetics was performed using a standard surgical method;
- primary prosthetics - with a small diameter of the valve ring (can be performed in 20-25% after surgical correction of tetralogy of Fallot).
Within the framework of clinical studies, it is possible to implant a bioprosthesis through vessels even with a large diameter of the valve ring. For this purpose, new types of prostheses are used that are not yet part of standard treatment.
Advantages of transcatheter prosthetics:
- minimal mortality;
- the possibility of performing the procedure even in patients at high surgical risk who cannot undergo classical surgery due to right ventricular failure or other reasons;
- there are no complications associated with the use of a heart-lung machine;
- minimal blood loss, no need for blood transfusion;
- fast recovery;
- mild course of the postoperative period.
Especially often in Europe, bioprostheses are used, installed in a minimally invasive way, for reprosthetics. In children, biological valves wear out quickly. In addition, the child grows, and the diameter of his blood vessels increases. As a result, even an intact bioprosthesis may fail. In such situations, minimally invasive prosthetics can delay repeat open-heart surgery and reduce the total number of surgical interventions undergone during a lifetime.
Valves for transcatheter replacement
The most widely used valve is the Melody valve (Medtronic). It is used for dysfunction of the right ventricular outflow tract in children who have undergone surgery for tetralogy of Fallot, as well as for implantation into a previously installed bioprosthesis. Melody is made from bovine jugular vein placed inside a platinum-iridium stent. The prosthesis has already been implanted in 15 thousand patients, mainly in the USA, Canada and Western Europe.
The bioprosthesis has proven itself well in clinical studies. Its implantation was successful in 89-95% of cases. Good hemodynamic results were maintained for at least 5 years after implantation. After its installation, regurgitation (backflow of blood) in the pulmonary artery immediately stops or is reduced to a mild degree.
SAPIEN XT (Edwards Lifesciences) - used in the same cases as Melody. It consists of a tricuspid bovine pericardial valve within a cobalt-chrome frame and was originally designed for use in the aortic position, similar to the Edwards Lifesciences Novaflex delivery system.
There are fewer studies on this bioprosthesis. It appears to produce comparable results. According to the COMPASSION study, installation is achieved in 95.2% of cases, and the absence of re-intervention after 1 year is 97.1%, after 3 years – 93.7%. The results of the French registry confirm these results. The valve was successfully installed in 95.8% of patients.
Possible complications after installation of a transcatheter valve:
- Stent fracture . Melody valve problem. There are no reports of fractures of SAPIEN XT bioprostheses yet. Previously, fractures were common. But now prestent placement (pre-stenting - frame installation) has become a standard procedure. The load on the stent is reduced, so it breaks very rarely. Most often, the Melody bioprosthesis is used in the USA. In this country, the incidence of hemodynamically significant fractures has decreased to 3%.
- Conduit rupture . It occurs in those who have undergone surgery for tetralogy of Fallot, after angioplasty. The complication is relatively common, but only 1% of patients experience life-threatening conduit ruptures.
- Compression of the coronary arteries . These are the vessels that feed the heart. A complication develops with a probability of up to 5%. To reduce the risk, European doctors simultaneously perform balloon angioplasty of the conduit (expanding it with a balloon) and coronary angiography (x-ray examination of the coronary arteries with contrast).
- Endocarditis . Inflammation of the endocardium. The risk of developing a complication is about 2.4% per year after Melody installation. It is approximately the same for patients after surgical and transcatheter prosthetics.
Melody bioprostheses have a maximum size of 22 mm, and SAPIEN - 29 mm. They cannot be installed if the diameter of the pathological outflow tract of the right ventricle is too large. Only a quarter of patients undergoing surgical correction of Tetralogy of Fallot are suitable for transcatheter placement of these valves.
Others have to undergo open-heart surgery. But recently, new types of prostheses have emerged that are suitable even for patients with a large diameter outflow tract, and make transcatheter prosthetics possible: Medtronic Harmony and Alterra Prestent from Edwards Lifesciences. They are currently being used in clinical trials.
Harmony TPV is a porcine pericardial tissue valve mounted in a self-expanding coated nitinol frame. It is larger than the regular Melody - the input is 34 mm and the output is 42 mm. Additionally, TPV 25 is being studied - it is even larger.
The Alterra Adaptive Prestent is not a valve, but a “docking station” for the 29mm SAPIEN S3 valve. It is a self-expanding coated nitinol frame with an hourglass shape. Diameter – 40 mm.
Treatment
Treatment of secondary pulmonary hypertension is aimed at getting rid of the underlying disease. Patients with severe pulmonary arterial hypertension due to chronic thromboembolism are treated with pulmonary thromboendarterectomy. This operation is considered more complex than emergency surgical embolectomy. Under conditions of extrapulmonary circulation, an organized vascularized thrombus is excised along the pulmonary trunk. In specialized centers, the mortality rate during and after surgery is less than 10%.
Treatment of primary pulmonary hypertension should begin with oral calcium channel blockers. In a minority of patients, these drugs reduce pulmonary artery pressure or pulmonary vascular resistance. Most doctors do not recommend verapamil because it has a negative inotropic effect. If treatment with calcium channel blockers is effective, the prognosis is favorable, you need to continue the course. If there is no response to treatment, the doctor prescribes other drugs.
Intravenous epoprostenol (a prostacyclin analogue) is often used to treat pulmonary hypertension. It increases survival in patients, even those who do not respond to vasodilator medications during catheterization. This treatment has disadvantages, such as the need for an indwelling central catheter. Side effects also occur, such as bacteremia and diarrhea. Oral (beraprost), inhaled (iloprost), subcutaneous (treprostinil) analogs of prostacyclin are considered alternative drugs. But their effects on the human body are still being studied, so they are not widely introduced into medical practice.
The oral endothelin receptor antagonist bosentan is effective in some cases. It is mainly prescribed for milder forms of pulmonary hypertension and insensitivity to vasodilators. L-arginine and oral sildenafil are also currently under investigation.
Lung transplantation is a dangerous procedure that can cause complications, because it is possible that an infection may occur and the body may reject the new lung. The procedure is used for heart failure of the fourth degree (according to the classification of the New York Heart Association), when a person develops shortness of breath even with minimal activity, due to which he cannot actively live, but constantly lies or sits; and only if in such cases there is no effectiveness of prostacyclin analogues.
Many patients are prescribed additional medications to treat deficiency, including diuretics. They should also receive warfarin to prevent thromboembolism.
Prognosis for pulmonary valve insufficiency
In the natural course of the defect, the prognosis is unfavorable. It inevitably leads to right ventricular heart failure. This pathology is irreversible. In advanced cases, patients do not even undergo surgery to replace the pulmonary valve due to the high surgical risk.
But with timely treatment, the prognosis is favorable. The ten-year survival rate of patients after installation of a bioprosthesis is 86%, and in the best clinics in Europe - 95%.
The bioprosthesis has a limited service life, especially in children. In a mixed group of patients of different ages, the need for repeated prosthetics arises:
- after 5 years – in 19% of patients;
- after 10 years – in 42% of patients;
- after 15 years – in 59% of patients.
In adults, the survival rate of bioprostheses is better. They usually last 15-30 years. After 15 years, only 25% of patients need reprosthetics.
Forecast
Without treatment, a person with pulmonary hypertension lives on average 2.5 years. The cause of death was sudden death due to right ventricular failure. Five-year survival with epoprostenol treatment is observed in more than half of patients. And when treatment with calcium channel blockers is effective, the 5-year survival rate is 90% or more.
Pulmonary hypertension has a poor prognosis if symptoms such as low cardiac output, higher pulmonary artery and right atrium pressures, lack of response to vasodilators, heart failure (HF), hypoxemia, and deterioration in overall functional status are present.