Composition and release form
The drug is sold in pharmacies in the form of small tablets for oral administration. Externally, they are white in color with a soluble thin shell. Packaged in blisters of 14 pieces and secondary cardboard packaging. One pack contains 1-2 cells of 14-28 tablets and includes instructions for use.
The active component of the drug is moxonidine. Its amount in 1 tablet is 200 mcg.
Additional substances: castor oil, cellulose, magnesium stearate, Tween 80, Klucel and Aerosil.
pharmachologic effect
The drug belongs to the group of antihypertensive drugs. It is a direct agonist of imidazoline receptors. When used once, it helps to simultaneously restore the level of diastolic and systolic pressure. At the same time, it does not change the activity of the heart and does not affect the heart rate.
The drug is highly digestible, regardless of the time of meal. The biological availability of the drug is at least 88%. The highest concentration of the drug in the red channel is observed after 30 minutes or a maximum of 3 hours.
The role of moxonidine in the treatment of arterial hypertension
The article presents data on the antihypertensive effectiveness of the imidazoline receptor agonist moxonidine and the possibilities of its use as part of combination therapy for arterial hypertension. The mechanisms of the antihypertensive effect of the drug, its effect on carbohydrate metabolism, and tissue sensitivity to insulin are considered. Moxonidine has an organoprotective effect, and due to its ability to reduce insulin resistance, it is recommended for the treatment of arterial hypertension in patients with metabolic syndrome, diabetes mellitus, and obesity.
Arterial hypertension (AH) is a serious health problem and is included in the list of socially significant diseases, since its prevalence is high (up to 40% among the adult population of Russia) and contributes to an increased risk of cardiovascular complications. The incidence of hypertension increases with age and reaches 50–60% in people over 60 years of age [1].
According to the latest national recommendations and the recommendations of the European Society of Cardiology (ESC), the main goal of hypertension treatment is to minimize the risk of developing cardiovascular complications and thereby cardiovascular death [2, 3].
To achieve this goal, it is necessary to achieve the target level of blood pressure (BP), reduce the severity of the patient’s modifiable risk factors or eliminate them (smoking, dyslipidemia, obesity, etc.), achieve regression of identified target organ damage and, finally, effectively treat associated diseases, primarily coronary heart disease (CHD) and diabetes mellitus (DM). The presence of coronary artery disease and type 2 diabetes in patients with hypertension means a high or very high cardiovascular risk. Therefore, the antihypertensive therapy chosen for these patients should, at a minimum, not worsen the course of concomitant diseases.
Previously, an increased risk of myocardial infarction (for rauwolfia preparations) and a critical deterioration of peripheral circulation in patients with diabetes with macroangiopathies in response to the use of non-selective beta-blockers were noted. In addition, some antihypertensive drugs that effectively lower blood pressure can have an adverse effect on carbohydrate and lipid metabolism (non-selective beta-blockers, thiazide diuretics in high doses).
For more than ten years, a program to combat hypertension has been implemented in Russia, and the reduction in cardiovascular mortality achieved in recent years is associated with successes in the treatment of hypertension. However, the frequency of achieving the target blood pressure level (
For the treatment of hypertension, modern recommendations propose five main classes of drugs: angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, slow calcium channel blockers, and diuretics. Additional antihypertensive drugs include selective I1-imidazoline receptor agonists, in particular the drug moxonidine, and alpha-blockers (doxazosin).
Since activation of the sympathetic nervous system (SNS) plays an important role in the pathogenesis of hypertension, for the treatment of hypertension it is advisable to prescribe drugs that can reduce the activity of the SNS, primarily beta-blockers. However, in some patients their prescription is impossible due to the presence of absolute or relative contraindications. In this situation, second-generation centrally acting drugs, such as selective I1-imidazoline receptor agonists (moxonidine, rilmenidine), can be used.
Mechanism of action of moxonidine
Moxonidine is an imidazoline receptor agonist. There are three types of imidazoline receptors [4–6]. Type 1 imidazoline receptors are localized in the central nervous system (in the nuclei of the reticular formation, rostral ventrolateral region of the medulla oblongata). Their activation leads to a decrease in the activity of the sympathoadrenal system, the level of norepinephrine and, consequently, the level of blood pressure due to a decrease in peripheral vascular resistance while simultaneously reducing the heart rate. Type 2 imidazoline receptors are located in the sympathetic nerve endings (they regulate the release of norepinephrine and adrenaline) and the kidneys (when stimulated, the level of plasma renin decreases and a moderate natriuretic effect is provided). Type 3 imidazoline receptors are found in the pancreas (they regulate insulin secretion by the beta cells of the islets of Langerhans).
An increase in the level of atrial natriuretic peptide may also contribute to the antihypertensive effect of moxonidine [7].
Pharmacokinetics
When taken orally, 90% of moxonidine is absorbed from the gastrointestinal tract, the maximum concentration is reached after 60 minutes [8]. The half-life of moxonidine and its metabolites is 2.5 and 5 hours, respectively. The antihypertensive effect continues throughout the day due to strong binding to I1-imidazoline receptors in the medulla oblongata. Moxonidine is excreted primarily in the urine (more than 90% of the drug is excreted within 24 hours) by glomerular filtration and tubular secretion and does not accumulate with long-term use, including in patients with moderate renal failure. In patients with end-stage renal failure (creatinine clearance less than 10 mg/min), the concentration of moxonidine in the blood plasma may be several times higher compared to patients with normal renal function.
Application in clinical practice
The indication for the use of moxonidine is hypertension. The antihypertensive effect after taking 0.2–0.4 mg of the drug begins after 30 minutes, reaches a maximum after 2–5 hours and lasts up to 24 hours. Moxonidine does not cause an excessive decrease in blood pressure at night, but at the same time effectively prevents the rise in blood pressure in the early morning hours.
When treated with moxinidine, there is a decrease in systolic blood pressure by 20–30 mmHg. Art., diastolic - by 10–20 mm Hg. Art. The greatest antihypertensive effect is achieved after three weeks of therapy, and its evasion is not observed [9]. In contrast to first-generation centrally acting drugs (in particular, clonidine), when moxonidine is stopped, no hypertension syndrome is observed [10] - blood pressure gradually returns to its original level.
The antihypertensive effectiveness of moxonidine is comparable to that of diuretics, beta-blockers, calcium antagonists and ACE inhibitors [11–15]. The ratio of residual to maximum reduction in blood pressure for moxonidine is 70% [15]. This is a very important indicator that characterizes the duration of the antihypertensive effect and, therefore, the possibility of prescribing the drug once a day.
The work of W. Scwarz et al. demonstrated that therapy with moxonidine at a dose of 0.2 mg/day in patients with hypertension of the first and second degree helps to normalize blood pressure in 62% of cases. In another 36% of patients, normalization of blood pressure was achieved by increasing the dose to 0.4 mg/day. The maximum reduction in blood pressure is observed in the third week of therapy, the resulting effect persists throughout the year of observation [9].
In elderly patients with hypertension, moxonidine leads to a mild, gradual decrease in blood pressure, and is well tolerated [16]. It is important that no significant differences in the effectiveness and frequency of side effects of therapy were recorded in older and younger patients.
Moxonidine can also be used as part of combination antihypertensive therapy. The TOPIC study, conducted in the UK, examined the effectiveness of moxonidine both as monotherapy and as combination therapy in 566 patients with hypertension [17]. With monotherapy with moxonidine at a dose of 0.2–0.4 mg/day, blood pressure control was achieved in 52% of patients. In combination therapy with hydrochlorothiazide (25 mg/day), amlodipine (5 mg/day) or enalapril, the combination with the second drug was most effective.
J. Abellan et al. moxonidine was prescribed at a dose of 0.4 mg to 112 patients with hypertension and obesity in whom previous antihypertensive therapy was ineffective. After six months, there was a decrease in systolic blood pressure by an average of 23 mm Hg. Art., diastolic - by 12.9 mm Hg. Art. At the same time, 63% of study participants achieved the target level of systolic blood pressure, 86% – diastolic blood pressure [18].
Use for uncomplicated hypertensive crises
Since, when moxonidine is prescribed for hypertension, a higher initial level of blood pressure is associated with a stronger decrease in blood pressure, the possibility of using the drug to relieve hypertensive crises has been actively studied [19, 20]. With sublingual administration of moxonidine at a dose of 0.4 mg, a significant decrease in blood pressure was observed in 90% of patients [19]. A significant decrease in systolic and diastolic blood pressure after a single dose of moxonidine was recorded after 20 minutes and reached a maximum after 1.5 hours. According to the results of the AVES study, moxonidine with a single dose of 0.4 mg significantly reduces blood pressure levels after 30 minutes [21].
It is important that after taking moxonidine, blood pressure decreases gradually (no more than 25% of the initial level), which is an indispensable condition for the safe treatment of uncomplicated hypertensive crises. In this case, the effect lasts for 12 hours (unlike captopril, the duration of action of which does not exceed 6 hours) [22, 14].
Organoprotective effect
Moxonidine may promote regression of left ventricular hypertrophy. This effect was established when patients with hypertension were treated with moxonidine for six months, while the ejection fraction did not change significantly [23]. The reduction in left ventricular hypertrophy has been confirmed in experimental studies. The mechanism of action of moxonidine on the myocardium can be explained by the activation of imidazoline receptors localized in the heart, regulation of apoptosis processes and DNA stabilization [24].
In a group of patients with essential hypertension and microalbuminuria (n = 56), the effectiveness of moxonidine monotherapy was studied. Patients received the drug at a dose of 0.3–0.4 mg/day for six months. Moxonidine contributed to a significant decrease in blood pressure, a decrease in the severity of albuminuria, the concentration of plasma thrombomodulin and plasminogen activator inhibitor. The authors of the study associated the dynamics of the levels of these markers with the normalization of the endothelium during treatment [25].
The clinical and pharmacoeconomic efficacy of moxonidine and nitrendipine were compared in a prospective randomized trial. It included patients with hypertension who suffered from chronic renal failure. Over three years of observation, terminal chronic renal failure developed in 38% of cases in those receiving nitrendipine, and in 7% in those receiving moxonidine. The total cost of treatment with moxonidine was four times lower than the cost of treatment with nitrendipine [26].
The renoprotective properties of moxonidine were confirmed by J. Radermacher et al. [27]. In 601 patients undergoing renal allotransplantation, treatment with moxonidine resulted in a 70% reduction in the risk of allograft failure.
It has been established that the use of moxonidine can also reduce the frequency and duration of paroxysms of atrial fibrillation. Thus, 56 patients with paroxysmal atrial fibrillation received moxonidine or placebo for six weeks (a crossover design was used) under the control of 48-hour electrocardiography monitoring. During treatment with moxonidine, a significant decrease in diastolic blood pressure and a decrease in the average duration of episodes of atrial fibrillation per day from 28 to 16 minutes were noted. The authors suggested that the antiarrhythmic effect of moxonidine is associated with its sympatholytic activity [28].
Metabolic effects
Insulin resistance and hyperinsulinemia are the leading links in the pathogenesis of metabolic syndrome. The ability of moxonidine to influence tissue sensitivity to insulin has been studied in several studies [29]. Thus, G. Derosa et al. compared the effectiveness of moxonidine as monotherapy and in combination with irbesartan in 99 patients with hypertension and diabetes. For three months, all patients received moxonidine at a dose of 0.2 mg, then for some of them the dose of the drug was doubled, for others, irbesartan was added at a dose of 150 mg/day. In both groups, a significant decrease in blood pressure was recorded, however, only those taking moxonidine at a dose of 0.4 mg/day found a decrease in blood glucose levels, glycated hemoglobin, an improvement in the insulin sensitivity index, as well as a significant increase in high-density lipoprotein cholesterol levels [30].
Moxonidine modulates all three types of imidazoline receptors, thus exerting a complex effect on blood pressure levels and the metabolic profile.
The effect of moxonidine on metabolic status was demonstrated in the ALMAZ study. It was shown that tissue sensitivity to insulin increased equally with the administration of moxonidine and with the administration of metformin [31, 32]. Moxonidine therapy was accompanied by an improvement in carbohydrate and lipid metabolism parameters, a decrease in leptin levels, an improvement in endothelial function, and a decrease in body weight.
The effectiveness and safety of moxonidine in patients with hypertension and metabolic syndrome were assessed in a large multicenter international study, MERSY. Russia also took part in it (272 patients with hypertension and metabolic syndrome, including postmenopausal women). Almost half of the study participants, after adding moxonidine to therapy, had a target blood pressure level, and the effectiveness of antihypertensive therapy was higher in women with preserved menstrual function than in postmenopausal women (the target blood pressure level was achieved in 73 and 41% of cases, respectively). All patients showed a significant improvement in parameters characterizing carbohydrate and lipid metabolism. Particularly impressive was the reduction in triglyceride levels – by 24% [33].
The effect of moxonidine on insulin resistance is associated with an effect on sympathetic activity, which is accompanied by a decrease in fat hydrolysis, fatty acid content, the proportion of insulin-resistant (type IIB) fibers in skeletal muscles, and acceleration of glucose metabolism in tissues. It is the increase in tissue sensitivity to insulin that can explain the significant decrease in body weight in patients with metabolic syndrome who participated in both the MERSY study and the ALMAZ study.
The use of moxonidine promotes the activation of lipolysis of adipose tissue and weight loss. This was shown in the large open-label CAMUS study. 4005 patients with hypertension who also suffered from obesity or metabolic syndrome received moxonidine as monotherapy and as part of combination therapy. In addition to the hypotensive effect, moxonidine significantly reduced body weight. Moreover, the degree of its reduction depended on the initial body mass index. Over eight weeks of observation, during therapy with moxonidine, the body weight of patients in the group decreased by 1.4 kg on average, while in patients with third-degree obesity it decreased by 4 kg [34]. Based on the data obtained, the Russian Ministry of Health recommended moxonidine for the treatment of hypertension in this category of patients [35].
Moxonidine and chronic obstructive pulmonary disease
Moxonidine effectively reduces blood pressure in patients with chronic obstructive pulmonary disease (COPD), who often have problems when prescribed beta-blockers and ACE inhibitors. The former worsen bronchial obstruction, the latter provoke coughing and increase bronchial obstruction. Thus, during therapy with moxonidine in 40 patients suffering from hypertension and COPD, systolic and diastolic blood pressure decreased by 15.4 and 17.4%, respectively, while most of the patients achieved the target blood pressure level. In addition, hemodynamics in the systemic and pulmonary circulation improved [36].
Safety and Tolerability
Moxonidine, compared to first-generation centrally acting drugs (reserpine, clonidine, guanfacine, alpha-methyldopa), has a significantly lower affinity for alpha-2 adrenergic receptors in the brainstem, and therefore side effects such as dryness develop much less frequently with its use in the mouth and sedation. However, their severity decreases after a few weeks.
The safety and tolerability of moxonidine were analyzed based on the results of 74 clinical studies (370 thousand patient-years). The most common (more than 2% of patients) side effects of moxonidine are dry mouth, headache and weakness. The incidence of other side effects did not exceed 1%. The drug was discontinued due to the development of side effects in less than 4% of cases [37].
Conclusion
The selective inhibitor of I1-imidazoline receptors moxonidine can be considered as a universal antihypertensive drug, effective both for long-term treatment of hypertension and for the relief of uncomplicated hypertensive crises.
Moxonidine has an organoprotective effect, is easy to use (once a day in the morning), and is well tolerated, including in elderly patients.
The positive effect of moxonidine on carbohydrate and lipid metabolism makes it the drug of choice in patients suffering from diabetes and metabolic syndrome.
The drug can be used as monotherapy, as well as in combination with ACE inhibitors, ARBs, calcium antagonists, and diuretics.
Contraindications
It is prohibited to take the medicine for the following conditions:
- Individual intolerance to the active or auxiliary components.
- Acute form of bradycardia.
- Severe arrhythmia.
- Glaucoma.
- Mental disorders.
- Cardiac failure.
- Previous Quincke's edema.
- The period of bearing a child and breastfeeding.
- Children under 18 years of age.
- Disturbance of the liver and kidneys.
- Angina pectoris.
- Lactose deficiency or intolerance.
- Various pathologies of the circulatory system.
Side effects
As a result of treatment with Moxonidine, patients may experience the following adverse reactions:
- High fatigue, malaise.
- Migraine.
- Sleep disorder - insomnia or drowsiness.
- Dizziness, headache.
- Dyspeptic manifestations - dry mouth, discomfort in the epigastrium, nausea, vomiting, abnormal stool.
- Increased nervousness and irritability.
- Swelling of peripheral tissues.
- A sharp decrease in pulse and blood pressure.
- Allergic signs are skin rash and severe itching.
Drug overdose
If medical recommendations are not followed and the maximum volume of the drug is exceeded, an overdose may develop. The condition is determined by severe symptoms:
- Intense headache and dizziness.
- Nausea followed by vomiting.
- Painful sensations in the stomach area.
- Weakness and severe malaise.
- Extensive reduction in pressure.
- Dryness in the mouth.
If the above symptoms occur, you should definitely consult a doctor. Treatment involves relief of symptoms. Prescribed medication, gastric lavage, parenteral administration of saline. To suppress the symptoms of bradycardia, the use of Atropine is indicated.
Moxonidine, while reducing sympathicotonia, does not lead to better blood pressure control
Studying the effects of central regulators of the sympathetic nervous system, blockers of the renin-angiotensin-aldosterone system and diuretics on endothelial function and blood pressure in metabolic syndrome.
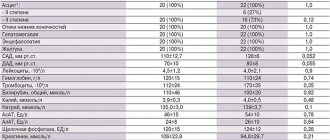
A randomized, double-blind, crossover study was conducted in 31 obese patients with untreated hypertension. The aim was to determine the effect on endothelial function and blood pressure in obese patients of different classes of drugs: central inhibitors of the sympathetic nervous system (moxonidine 0.4 mg), blockers of the renin-angiotensin-aldosterone system (aliskiren 300 mg), diuretics (hydrochlorothiazide 25 mg) and placebo. Control was carried out by measuring flow-mediated endothelium-dependent vasodilation* and 24-hour blood pressure (BP) monitoring.
With placebo, flow-mediated endothelium-dependent vasodilation was 4.0% and significantly increased with aliskiren by 0.81% (95% CI 0.02%-1.79%), which did not occur with moxonidine 0.20 %(95% CI -0.46%-1.03%) and hydrochlorothiazide 0.39% (95% CI -0.31%-1.26%). Similarly, 24-hour BP monitoring showed a better reduction with aliskiren (-9.8/-6.3 mmHg) compared with placebo and a lesser effect with hydrochlorothiazide (-5.9/- 2.6 mmHg). It is important that moxonidine, despite its central effect on inhibiting the pressor action of the sympathetic nervous system, did not show a statistically significant effect on blood pressure levels. Insulin resistance worsened while taking hydrochlorothiazide. Thus, renin inhibitors improve endothelial function and lead to better control of blood pressure levels. The authors hypothesize that renin-angiotensin-aldosterone system inhibitors, as opposed to moxonidine, are an effective first step in the treatment of hypertension in individuals with metabolic syndrome.
Source: Dorresteijn JA et al. Differential effects of renin-angiotensin-aldosterone system inhibition, sympathoinhibition and diuretic therapy on endothelial function and blood pressure in obesity-related hypertension: a double-blind, placebo-controlled cross-over trial. J Hypertens. 2012 Dec 11.
A comment
In view of recent data on the early termination of the ALTITUDE study due to an increase in the incidence of side effects in the aliskiren group compared with the placebo group in the absence of clinical benefits among patients with type 2 diabetes, talk about aliskiren as a first-line drug in the treatment of arterial hypertension in people with metabolic syndrome we can not. However, the results regarding the ineffectiveness of moxonidine in a small cohort of patients compared with hydrochlorothiazide and aliskiren, obtained by the authors of the study under discussion, “cast a shadow” on the drug and make its use questionable. Of course, to create recommendations for treatment tactics for patients, it is necessary to conduct large, well-organized randomized clinical trials.
Detailed results of the ALTITUDE randomized clinical trial are presented on our website in the “Expert Advice” section (Aliskiren Trial in Type 2 Diabetes Using Cardiorenal Endpoints).
* The essence of the DS Celermajer test (flow-mediated endothelium-dependent vasodilation) is to measure the diameter of the brachial artery using an ultrasound method. First, the initial diameter of the brachial artery is determined at rest. Then a sphygmomanometer cuff is placed on the shoulder and inflated to a level of 50 mmHg. exceeding systolic blood pressure. The next measurements of the diameter of the brachial artery are determined at 30, 60, 90 seconds after removing air from the cuff. The change in the diameter of the vessel at 60 seconds is assessed as a percentage of the initial value. Normally, the diameter of the brachial artery increases by more than 10% from the initial level.
Related materials:
- The results of a randomized, double-blind, crossover study in 31 obese patients with untreated hypertension have been published.
- The role of antiadrenergic drugs in the treatment of arterial hypertension and chronic heart failure
special instructions
The use of an antihypertensive drug for therapeutic purposes requires constant monitoring of blood pressure, heart function and heart rate.
During the course of treatment, you should completely avoid alcoholic beverages. It is recommended not to drive vehicles or engage in activities that require concentration, memory and high mental activity.
You need to stop taking the drug gradually, gradually reducing the dose until complete withdrawal.
If the use of Moxonidine was combined with beta-blockers and it is necessary to discontinue both drugs, the latter are removed first. After some time, the antihypertensive drug is discontinued.
Currently, the significance of arterial hypertension is beyond doubt: an increase in blood pressure (BP) above 140 mm Hg. responsible for a significant increase in mortality and disability (70%) and the largest number of deaths due to coronary heart disease (4.9 million), hemorrhagic (2.0 million) and ischemic (1.5 million) strokes [1]. A meta-analysis of randomized trials showed that a decrease in systolic blood pressure (SBP) by 10 mm Hg. or diastolic blood pressure (DBP) by 5 mmHg. is associated with a reduction in cardiovascular events by 20%, overall mortality by 10-15%, stroke by 35%, coronary events by 20%, and heart failure by 40% [2, 3]. Thus, adequate treatment of arterial hypertension (AH) is one of the main tasks in preventing the development of cardiovascular events and, ultimately, mortality.
In 2021, new European guidelines for the diagnosis and treatment of hypertension were published, and in the same year an updated revision of the Russian clinical guidelines for hypertension was published, according to which there are two strategies for lowering blood pressure levels: modification of risk factors and drug therapy. Both documents state that patients with stage 2–3 hypertension should receive drug therapy regardless of lifestyle changes [4, 5]. When using antihypertensive drugs, the primary goal is to reduce blood pressure to <140/90 mmHg. If well tolerated, further titration of the dose is necessary to achieve a blood pressure level of 130/80 mm Hg. in most patients, and in patients over 65 years of age, the recommended values for SBP are 130-140 mm Hg, DBP is less than 80 mm Hg.
Currently, five main classes of drugs are recommended for drug therapy of hypertension: angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), beta-blockers, calcium antagonists, and diuretics. The most widely used classes of antihypertensive drugs are ACE inhibitors and angiotensin receptor blockers (ARBs), which in clinical trials have shown similar positive effects on the incidence of cardiovascular events and mortality among patients with arterial hypertension [6, 7].
ACE inhibitors and ARBs are recommended for the treatment of hypertension if the patient has concomitant diabetes mellitus (DM) or metabolic syndrome, chronic ischemic heart disease, a history of myocardial infarction (MI), heart failure, or atrial fibrillation [8, 9, 10]. Drugs of both classes, compared to others, more significantly reduce the level of albuminuria and are more effective in slowing the progression of chronic kidney disease (CKD), including in patients with diabetes.
However, it should be noted that ACE inhibitors are not able to block alternative pathways for the formation of angiotensin II and at the same time activate the bradykinin system, which contributes to the development of side effects such as cough and angioedema.
The positive effects of ARBs are mediated by several mechanisms. Due to the selective blockade of angiotensin II type 1 receptors (AT1), the effects of activation of the renin-angiotensin-aldosterone system (RAAS), such as vasoconstriction, stimulation of aldosterone synthesis and sodium reabsorption, are eliminated. The use of ARBs also has a positive effect on endothelial dysfunction by inhibiting the processes of inflammation and vascular remodeling, as well as oxidative stress, which, in turn, can prevent the development of atherosclerosis and reduce the risk of major cardiovascular events [11, 12, 13]. With the use of ARBs, the effect of angiotensin II on AT2 receptors increases, which leads to vasodilation and natriuresis.
ARBs have also been shown to be the only class of drugs that reduce the risk of adverse outcome in patients with end-stage chronic kidney disease (CKD) [14].
Currently, the doctor's arsenal has a sufficient number of ARBs for the treatment of arterial hypertension: azilsartan, candesartan, eprosartan, irbesartan, losartan, olmesartan, telmisartan and valsartan. Due to their molecular differences, these drugs differ significantly in pharmacokinetic and pharmacodynamic properties, which may influence clinical efficacy. These differences relate to lipophilicity, volume of distribution, bioavailability, biotransformation, plasma half-life, receptor affinity and retention time, and elimination [15].
Telmisartan has a longer antihypertensive effect compared to other ARBs, which is likely due to the longest half-life of the drug, which is about 24 hours. As the most lipophilic, telmisartan also has the highest volume of distribution, which facilitates penetration into tissues and organs, thereby blocking not only the systemic, but also the local renin-angiotensin-aldosterone system, which reduces target organ damage [16, 17]. The drug has a high affinity for the AT1 receptor subtype of angiotensin II, through which the action of angiotensin II is realized. Displaces angiotensin II from its connection with the receptor, without exhibiting agonist properties in relation to this receptor. Telmisartan binds only to the AT1 receptor subtype of angiotensin II, and the association is long-lasting. In patients with hypertension, telmisartan at a dose of 80 mg once daily completely blocks the hypertensive effect of angiotensin II. The onset of the antihypertensive effect is observed within 3 hours after the first oral dose. The effect of the drug remains significant for up to 48 hours. A pronounced antihypertensive effect usually develops 4 weeks after regular use [18].
Today, a sufficient evidence base has been accumulated regarding the effectiveness and safety of telmisartan for the treatment of hypertension. A randomized, double-blind, multicenter, international clinical trial in parallel groups, ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial), was performed to compare the effectiveness of telmisartan alone and in combination with ramipril on disease outcome in patients at high risk of developing cardiovascular disease. complications. The results of the study showed that the primary end point (death from cardiovascular causes or myocardial infarction, stroke, hospitalization for CHF) developed in the same number of patients, regardless of therapy: in 1412 patients (16.5%) in the ramipril group, in 1423 patients in the telmisartan group (16.7%; RR=1.01; 95% CI 0.94-1.09), 1386 patients in the combination therapy group (16.3%; RR=0.99; 95% CI 0.92–1.07). Regarding the number of side effects in patients receiving telmisartan, compared with ramipril, cough (1.1% vs 4.2%; p < 0.001) and angioedema (0.1% vs 0.3%; p) were less common. =0.01), however, hypotension was observed significantly more often (2.7% vs 1.7%; p<0.001) [19]. The results of this randomized clinical trial (RCT) allowed ARBs to be considered not only as an alternative to ACE inhibitors, but also as a drug of choice when initiating antihypertensive therapy. In modern clinical guidelines for the diagnosis and treatment of arterial hypertension, the combination of ARBs and ACE inhibitors is considered irrational [10].
In another large randomized international multicenter study, TRANSCEND (Telmisartan Randomised AssessmeNt Study in ACE iNtolerant subjects with cardiovascular disease), telmisartan prescribed at a dose of 80 mg once a day (n=2954) was compared with placebo (n=2972) in patients who cannot tolerate treatment with ACE inhibitors, have cardiovascular diseases or type 2 diabetes with signs of target organ damage. As with ONTARGET, therapy lasted an average of 56 months. The average age of the patients was 66.9 years, the initial blood pressure level was 141/82 mm Hg. in both groups. In the TRANSCEND trial, telmisartan was well tolerated but did not affect the primary endpoint of ONTARGET (all cardiovascular death, MI, stroke, and heart failure hospitalizations). At the same time, telmisartan significantly reduced the incidence of the secondary endpoint (all cases of cardiovascular death, MI and stroke compared with placebo (13.0% vs 14.8%, respectively) [20].
In addition, important data were obtained regarding the effect of telmisartan on left ventricular hypertrophy (LVH) in patients at high cardiovascular risk in the absence of heart failure (HF). In the TRANSCEND trial, telmisartan significantly reduced the prevalence of LVH (p=0.0017) compared with placebo after 2 years of therapy (10.5% vs 12.7%) and after 5 years of therapy (9.9% vs 12.8%) . It is important to note that telmisartan also prevented the occurrence of new cases of LVH [21].
Also worthy of attention is the prospective multicenter study PRoFESS (Prevention Regimen For Effectively avoiding Second Strokes) on secondary prevention of stroke in patients both with and without hypertension. This study compared telmisartan 80 mg/day (n=10,146) with placebo (n=10,186) in patients with recent stroke (less than 90 days before randomization). Patients were aged 50 years or older, with a mean age of 66 years. Initial blood pressure in both groups averaged 144.1/83.8 mm Hg. The observation lasted 2.5 years. According to the results obtained, in the telmisartan group there was a tendency to reduce the incidence of recurrent stroke (8.7% vs 9.2%; p=0.23), major cardiovascular events (13.5% vs 14.4%; p=0. 11) and new cases of diabetes mellitus (1.7% vs 2.1%; p=0.10) [22].
The results of the TRANSCEND and PRoFESS studies proved that treatment with telmisartan significantly reduces the risk of MI, stroke and cardiovascular events compared with placebo in patients with a high and very high risk of complications, regardless of the initial blood pressure level.
The drug has also been studied in patients with atrial fibrillation (AF). In a study in patients with moderate hypertension (BP 140–159/90–99 mmHg) and a confirmed episode of AF within the previous 6 months, telmisartan 80 mg/day was compared with carvedilol 25 mg/day. The observation period was 1 year. As a result, the incidence of AF episodes in the telmisartan group was significantly lower (14.3% vs 37.1%; p<0.003). Both drugs significantly reduced the left ventricular mass index, but in the telmisartan group this indicator was also significantly lower (117.8±10.7 vs 124.7±14.5; p<0.0001) [23].
A similar study was performed in 2012 in patients with hypertension and metabolic syndrome. The study included 391 patients with documented AF, who were randomized into 3 groups: telmisartan, ramipril and amlodipine. The observation period was 1 year. According to the results, all drugs showed equal effectiveness in lowering blood pressure levels. The incidence of AF paroxysms in the telmisartan group was 12.9%, which was significantly lower compared to other groups (p<0.01 compared to amlodipine and p<0.05 compared to ramipril). Researchers suggest that this effect of telmisartan is associated with a positive effect on atrial electrical remodeling [24].
An important aspect when conducting antihypertensive therapy is its metabolic neutrality, and ideally, a positive effect on metabolic parameters. This is especially true in older patients, where hypertension is often associated with metabolic syndrome or diabetes. Telmisartan in studies had a positive effect on the severity of both hemodynamic and metabolic disorders in patients with hypertension and obesity. The results of a meta-analysis showed that telmisartan therapy significantly improves key metabolic parameters such as fasting glucose, insulin, glycated hemoglobin (HbA1c) and HOMA (insulin resistance index) in patients with metabolic syndrome [25].
It is also necessary to cite data from the ATHLETE study (ARB trial of hypertension in obese patients with hyperinsulinemia assessed by oral glucose tolerance test) lasting 6 months, which included 28 elderly patients with an average body mass index (BMI) of 27.1 kg/m2. Patients were randomly assigned to either switch from candesartan or valsartan to telmisartan according to the study design, or to continue receiving the previously prescribed sartan. It was shown that in patients with obesity, hypertension and insulin resistance, telmisartan significantly improved insulin response in the glucose load test [26].
It is known that an increase in blood pressure is mediated in a variety of ways, and therefore in most cases, especially in patients with moderate and severe hypertension, the use of a combination of antihypertensive drugs that act on various parts of the pathogenesis of the disease is required [27]. According to clinical guidelines for the treatment of arterial hypertension, in cases where systolic or diastolic blood pressure exceeds target values by 20 mm Hg. or 10 mm Hg. Accordingly, multicomponent antihypertensive therapy should be used. In turn, prescribing fixed doses of drugs in one tablet can increase patient adherence to treatment, provide more adequate blood pressure control, and also reduce the number of potential side effects [28, 29].
In connection with the above, the results of studies on the use of telmisartan as a combination therapy are of interest. The TEAMSTA-5 and TEAMSTA-10 studies (TElmisartan plus AMlodipine STudy - Amlodipine 5 mg and 10 mg) followed 1814 patients. Patients were randomized into one of the groups: telmisartan 40 mg / amlodipine 5 mg - T40/A5, telmisartan 80 mg / amlodipine 5 mg - T80/A5 (TEAMSTA-5), telmisartan 40 mg / amlodipine 10 mg - T40/A10, telmisartan 80 mg / amlodipine 10 mg - T80/A10 (TEAMSTA-10), and are further divided into subgroups depending on the tactics: adding other drugs to therapy or increasing the dose of telmisartan. The primary efficacy endpoint was rate of DBP control (ie, <90 mmHg). These BP targets were achieved in ≥76% of participants and did not require an increase in dose to the maximum dose or the addition of other drugs to therapy (T80/A5+drug, TEAMSTA-5) or dose escalation (T80/A5); DBP could be controlled in 46.4% and 66.7% of patients in these groups, respectively. Treatment response rate assessed by achieving DBP <90 mmHg. or ≥10 mmHg decrease in DBP was 69%, and the response rate as assessed by SBP (SBP <140 mmHg or ≥15 mmHg decrease in SBP) was greater than 70% in all groups [30].
Telmisartan has also been studied in combination with other major classes of antihypertensive drugs. Thus, in a multicenter randomized trial involving 805 patients, telmisartan at a dose of 40 mg in combination with hydrochlorothiazide (HCTZ) 12.5 mg demonstrated superiority over losartan 50 mg in combination with HCTZ 12.5 mg in patients with essential hypertension during a 24-hour outpatient period. blood pressure monitoring, including assessing the decrease in blood pressure during the last 6 hours of the dosing interval. Compared with the group of combination of losartan with HCTZ, a significantly more significant decrease in blood pressure was demonstrated. In addition, glucose tolerance was shown to be significantly improved in the telmisartan group [31].
Today, there is a generic telmisartan on the Russian pharmaceutical market - the drug Telsartan, which has proven bioequivalence to the original telmisartan, which significantly expands the possibilities of using this ARB in clinical practice. The optimal price of the drug Telsartan is also of considerable importance, which makes it affordable to most patients with hypertension.
Thus, the drug telmisartan is an effective and safe drug for long-term treatment of patients with hypertension and coronary artery disease, to reduce cardiovascular diseases, including a history of stroke, diabetes mellitus, and atherosclerosis of peripheral arteries. The drug has been proven to cause regression and prevent the development of new cases of left ventricular hypertrophy.
It is very important to note that the drug telmisartan is well tolerated by patients without causing clinically significant side effects.
Russian clinical guidelines for the diagnosis and treatment of hypertension also prescribe other (additional) classes of antihypertensive drugs. These classes, in particular, include imidazoline receptor agonists; a representative of this class is the drug moxonidine (Physiotens) [5]. Imidazoline receptor agonists represent a separate subclass of drugs with fewer side effects and can be used in combination at any stage of the treatment of hypertension, especially in patients with signs of hypersympathicotonia, in patients with metabolic syndrome and insulin resistance. It is advisable to add this group of drugs for resistant hypertension associated with obesity. [32]. The uniqueness of the original moxonidine lies in the fact that it is not only used in routine therapy of patients with hypertension, but is also widely used to relieve uncomplicated hypertensive crisis [33, 34, 35].
Moxonidine has a high affinity for imidazoline I1 receptors and, unlike other drugs with a central effect on the sympathoadrenal system (clonidine, methyldopa), only slightly binds to central α2-adrenergic receptors, the action of which is responsible for the development of the main side effects (drowsiness, sedation , dry mouth) [36]. The decrease in systolic and diastolic blood pressure when taking moxonidine is associated with a decrease in the pressor effect of the sympathetic nervous system on peripheral vessels, a decrease in total peripheral vascular resistance, while there is no significant effect on cardiac output and pulmonary hemodynamics.
V. Mitrovic et al. studied the hemodynamic and neurohumoral effects of a single oral dose of 0.4 mg moxonidine for 4 hours in ten patients with stage I-II hypertension. Indicators of pulmonary artery pressure and cardiac output were determined both at rest and during ergometric exercises using a Swan-Hans catheter. As a result of the study, moxonidine caused a significant decrease in blood pressure during a 4-hour observation period - from 176/105 mm Hg. up to 158/95 mm Hg. (p<0.01), accompanied by a decrease in systemic vascular resistance from 1695 to 1427 dynes/cm2 (p<0.01). Cardiac output remained unchanged, while heart rate increased slightly, from 69 to 75 beats/min (p<0.01). No significant changes in pulmonary artery pressure were recorded. Plasma levels of norepinephrine (337 vs 224 pg/ml) and renin (2.6 vs 2.0 ng/ml/h) were significantly reduced by moxonidine (p<0.05) both at rest and during exercise. exercises. Although plasma aldosterone levels decreased slightly, angiotensin II levels remained unchanged [37].
In an 8-week study, moxonidine monotherapy 0.2–0.6 mg/day reduced DBP to a significantly greater extent than placebo (on average 10.7–13.2 mmHg from baseline), in patients with mild or moderate hypertension. SBP values decreased by an average of 19.5–24.9 mmHg. The decrease in SBP and DBP during therapy with moxonidine 0.2-0.8 mg/day for 8 weeks was similar to the decrease in these indicators when using enalapril 5-20 mg once a day, atenolol 50-100 mg/day (except for women after menopause, where atenolol reduced blood pressure to a greater extent than moxonidine), hydrochlorothiazide 25 mg once daily. In another study, during a 26-week follow-up, the reduction in SBP and DBP while taking moxonidine 0.2-0.4 mg/day was similar compared to patients receiving sustained-release nifedipine 20-40 mg/day. In other studies, in patients who did not respond to moxonidine monotherapy, the average improvement in DBP after 4 weeks of therapy was −7.3 mmHg. with a combination of moxonidine 0.4 mg plus amlodipine 5 mg once a day, −4.8 mmHg. with a combination of moxonidine plus enalapril 10 mg and −3.2 mmHg. with a combination of moxonidine 0.4 mg plus hydrochlorothiazide 12.5 mg. In another study, changes in SBP and DBP after 8 weeks of treatment were significantly greater with the combination of moxonidine 0.4 mg plus hydrochlorothiazide 25 mg than with the corresponding monotherapy (−27 mmHg vs. −20 mmHg and −22 mmHg). Hg and –16 mmHg vs –12 mmHg and –13 mmHg) [38].
G. Derosa et al. Patients with type 2 diabetes mellitus and mild hypertension (DBP >90 and <105 mmHg), who had not previously received treatment, were prescribed moxonidine at a dose of 0.2 mg/day during the first 3 months of the study. They were then randomized to either moxonidine 0.4 mg monotherapy or moxonidine 0.2 mg plus irbesartan 150 mg. The study involved 99 patients, average age 55 years, average body mass index 26.8 kg/m2. After 3 months, therapy with moxonidine at a dose of 0.2 mg led to a significant decrease in SBP and DBP compared to baseline values (p <0.05), while there were no significant changes in the level of HbA1c and lipid spectrum indicators. At 6 months, significant reductions from baseline in HbA1c, triglycerides, and low-density lipoprotein levels were observed in the moxonidine 0.4 mg group (p < 0.05) but not in the combination treatment group. It was also noted that while taking moxonidine 0.4 mg, there was a significant increase in the level of high-density lipoproteins compared to baseline (p < 0.05). The authors concluded that monotherapy with moxonidine 0.4 mg in patients with type 2 diabetes mellitus and mild hypertension leads to more significant improvements in glucose metabolism and plasma lipid profile compared with the combination of moxonidine 0.2 mg and irbesartan [39] .
In conclusion, it should be noted that, despite the fact that moxonidine does not belong to the main classes of antihypertensive drugs recommended by the European Society of Cardiology for the treatment of hypertension, the drug has proven its effectiveness and safety, including as a combination therapy, and there is no reason to discontinuation of such therapy in patients receiving this group of drugs, provided they are well effective and tolerable.
The authors declare no conflict of interest.