HomeChildren's clinicCardiologyCongenital heart disease
Congenital heart defect
- a disease of the heart valves, in which the organ begins to malfunction. As a result of a congenital change in the structure of the valve apparatus, cardiac septa, walls, or large vessels extending from the heart, a disturbance in the blood flow of the heart occurs. The disease may progress. In some cases, death is possible.
Congenital heart defects occur with a frequency of 6-8 cases per thousand births, which is 30% of all developmental defects. They rank first in mortality of newborns and children of the first year of life. After the first year of life, mortality decreases sharply, and no more than 5% of children die between the ages of 1 and 15 years.
The earlier a congenital heart defect is detected, the greater the hope for its timely treatment.
General information
Congenital heart disease is the most common congenital anomaly leading to mortality. Occurs in approximately 1% of newborns. Congenital heart defects most often appear in childhood. They can progress and, if not treated correctly, lead to death. Source: JIE Hoffman, S. Kaplan The incidence of congenital heart disease // JACC, 2002, Vol. 39, p.1890—1900
CHD can manifest as single anomalies or a combination of several disorders. It is most dangerous when the disease has no external manifestations and passes hidden. In modern conditions, treatment is usually successful, but timely and accurate diagnosis is vital.
The actions of the mother during pregnancy and of both parents during preparation for it are also important. To assess the risk of having a baby with congenital heart disease, you need to contact a geneticist.
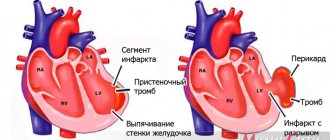
CHD entails a number of complications, including bacterial endocarditis, heart failure, early pneumonia with a prolonged course, short-term fainting, pulmonary hypertension, myocardial infarction, attacks of shortness of breath, and angina syndrome.
Narrowing of the aortic tunnel (coarctation of the aorta)
Aortic narrowing is a congenital heart defect diagnosed in approximately 5-10% of newborns with abnormalities in the structure of the heart. This is a partial closure of the aortic light within the subclavian artery on the left. It is important to note that this heart defect is diagnosed much more often in boys than in girls. Coarctation of the aorta in children takes the form of a narrowing along a long section of the main artery. At the same time, it is also accompanied by other heart defects indicating hypoplasia of cardiac structures (for example, bicuspid aortic valve, mitral valve stenosis, hypoplasia of the aortic arch). Among the consequences of this heart defect are ischemia of the lower half of the body, necrotizing enterocolitis, and renal failure. Aortic narrowing is usually accompanied by tachycardia, shortness of breath and liver enlargement. Characteristic symptoms of this heart defect:
- Accelerated cardiac activity.
- Dyspnea.
- Fast fatiguability.
- Enlarged liver.
- Low urine production.
- Cold extremities.
- Metabolic acidosis.
Treatment requires immediate administration of prostaglandin E1, a hormone with vasodilating properties. In addition, it is necessary to reduce the degree of unpleasant symptoms that can threaten the child’s life, and sometimes implement artificial ventilation. Surgical treatment for this heart defect can be used no earlier than the child is 6 months old.
Phases of the disease
CHD occurs in three phases:
- first phase: during it, a compensatory and adaptive reaction to a failure in the dynamics of blood circulation is observed; in case of a serious violation, myocardial hyperfunction occurs.
- second phase: relative compensation occurs. The child’s motor activity and physiological development improves.
- the third phase is terminal. The body has already exhausted the possibilities of compensation; degenerative, dystrophic pathologies of the heart and nearby blood vessels are developing. If a child is sick, especially with complications, then the terminal phase occurs faster. Its outcome is only fatal. Source: E.E. Chepurnykh, E.G. Grigoriev Congenital heart defects // Siberian Medical Journal (Irkutsk), 2014, No. 3, pp. 121-127
Therefore, the earlier the pathology is detected, the more favorable its prognosis.
To wait or not to delay?
A quarter of the defects are critical, for which surgery must be done immediately after birth. You can wait with other types of them. And there are also defects (for example, small defects of the interventricular septum of the heart) that often close on their own over time.
Previously, such children were diagnosed with a huge delay and often when it was too late to do anything. But with the advent of high-quality ultrasound diagnostics, many congenital heart defects are detected even at the stage of intrauterine development. And, although a definitive diagnosis can only be made at birth, such a diagnosis is extremely important.
Sudden death - during physical education. Why do children die in class? More details
Causes of pathology
CHD may develop if:
- parents smoke;
- parents drink alcohol;
- the fetus is affected by external factors during the period of development and formation (high background radiation, lack of vitamins, viruses carried by the mother, polluted air, water, a number of chemicals, including heavy metals). Source: L.N. Falyush, V.V. Florensov Risk factors for congenital heart defects // Clinical medicine. Bulletin of the All-Russian Scientific Center SB RAMS, 2010, No. 6(76), p.67-69
Mitral valve narrowing
Mitral valve narrowing is a relatively rarely diagnosed heart defect. This leads to impaired blood flow, increased pressure in the left atrium and, as a result, overload of the right ventricle. This defect occurs in three variants: subvalvular, valvular and supravalvular. Characteristic symptoms of this heart defect are: shortness of breath, fatigue (decreased tolerance to physical activity), lack of body weight. Due to the high risk of serious complications, the recommended treatment for this heart defect is implantation of an artificial or biological valve. It is important to note that people with artificial or biological valves must take anticoagulants throughout their lives because they often have thromboembolic complications.
Section: Articles Tags: cardiology
Symptoms of congenital heart disease
They are divided into two large groups according to the color of the child’s skin: “white” and “blue”. A changed skin tone is the first reason for parents and pediatricians to be wary.
"Blue" vices
They usually appear either immediately at birth or a little later. In this case, the ears, lips and body skin are susceptible to cyanosis. Blue discoloration can occur during exertion (screaming, crying of a newborn), during breastfeeding. The “blue” appearance is usually manifested by a mirror arrangement of the great vessels, atresia of the pulmonary artery, and tetralogy of Fallot.
CHD of the “white” variety
Accompanied by pallor and coldness of the extremities. When listening with a stethoscope, noises are heard. They are not direct symptoms, but a heart examination is still required. With “white” pathologies, heart failure is often detected. Changes are detected on x-rays, ECG, ECHO-CG. This type of congenital heart disease is most often a pathology of the interatrial septum and interventricular septum.
Unfortunately, not all types of congenital heart disease occur in newborns. A child can feel well even up to 10 years of age. But sooner or later the vice will appear:
- delay in physiological development;
- pallor or cyanosis;
- shortness of breath during exercise.
Heart defects in children
Diseases of the cardiovascular system occupy one of the leading places among all diseases diagnosed in children and adolescents.
There has been a steady increase in the number of children with this pathology. The majority of diseases of the cardiovascular system are heart defects. In most cases, the cause of the defect is unknown. However, it is often associated with factors such as chromosomal abnormalities, viral infections, and intoxication. Nowadays, heart defects in children can be expressed in a ratio of 1:200 (1 child with a heart defect per 200 healthy ones). However, such diseases are not always life-threatening.
Heart disease in children
Functional divisions of the heart into the right (pulmonary) and left (systemic) sections occur only after birth. During the period of intrauterine development, the atria and ventricles of a child act as a single hollow organism, communicating through the foramen ovale.
The essence of all defects is as follows: the four chambers of the heart (2 atria and 2 ventricles) are separated from each other by partitions and valves, ensuring blood flow in the right direction. The presence of a defect in one of the walls or an abnormality of the valve is a heart defect. All defects are conventionally divided into two categories - congenital and acquired.
Congenital heart disease in children
These are anomalies in the structure of the heart and large vessels that form during the period of embryonic development, as a result of which disturbances in hemodynamics occur - the movement of blood through the vessels, which can lead to heart failure and degenerative changes in the tissues of the body.
This is one of the most common congenital anomalies in children - 30% of all congenital malformations. The highest incidence of congenital malformations among all live births is found in low birth weight infants, especially premature infants. In terms of frequency of occurrence, it ranks third after congenital pathologies of the musculoskeletal system and nervous system.
All congenital heart defects can be divided into four main groups; they can occur in isolation and in various combinations:
- defects of the interatrial, interventricular, atrioventricular septa;
- stenosis or insufficiency of heart valves;
- three-chambered (single-ventricle) heart;
- transposition of the great vessels;
- dextrocardia is an abnormal location of the heart in the right half of the chest.
Patent ductus arteriosus, Atrial septal defect, Ventricular septal defect, Patent atrioventricular canal, Common truncus arteriosus, Isolated pulmonary artery stenosis, Tetralogy of Fallot, Ebstein's anomaly, Coarctation of the aorta - these are a few of the diagnoses that parents of a sick baby can hear from a doctor. More than 90 variants of the disease and about 200 different combinations exist in the structure of congenital heart defects.
Approximately 50% of patients with congenital heart disease require therapeutic or surgical intervention in the first year of life. In half of these cases, the critical condition is associated with heart failure and in half with arterial hypoxemia or the threat of closure of the patent ductus arteriosus (ductus). A relatively small group consists of children with isolated rhythm disturbances.
Separately, I would like to note the ventricular septal defect and not, because it accounts for approximately 30% of all heart defects. But because in more than 80% of cases it does not require treatment, since it closes on its own in the child during the first months or years of life.
Acquired heart defects in children
Acquired heart defects in children are typical for the older age group. They arise as a result of progressive or chronic diseases, or traumatic damage to valve structures. This type of heart defect is detected in 3% - 6% of children; it should be taken into account that at present this figure has decreased significantly due to the fact that the incidence of rheumatism, which is the main source of the formation of PPS, has decreased. Although sometimes a congenital heart defect remains undetected until later in childhood.
Classification of acquired heart defects:
- Mitral valve defects;
- Aortic valve defects;
- Tricuspid valve defects;
- Pulmonary valve disease;
- Infective endocarditis;
- Pericarditis.
Abnormalities of valve structures disrupt blood flow throughout the body. There are three main types of heart valve dysfunction:
- stenosis - the leaflets cannot open fully, resulting in a decrease in the area of the valve opening;
- prolapse - the valves lengthen and sag when closing;
- regurgitation is a condition when the valves are not able to close completely, and a reverse blood flow occurs, opposite to the normal, physiological one. Pathology of the heart valves provokes the development of arrhythmia and thromboembolism as a result of the accumulation of blood clots in the dilated chambers of the heart.
A rare but serious cause of heart valve pathology is infective endocarditis.
Bacteria enter the bloodstream as a result of:
- direct infection through intravenous injections;
- dental and medical procedures;
- severe or chronic infections such as abscesses.
Bacteria enter the bloodstream and settle on the valve flaps, causing irreversible changes.
Symptoms of heart defects in children
Many congenital heart defects are recognized before birth. At the 18th week of pregnancy, an ultrasound examination, in addition to assessing the size of the fetus, diagnoses structural abnormalities. Ultrasound diagnostic specialists, among other things, identify signs of congenital heart disease in a child.
Symptoms of heart defects can be observed at birth. For example, severe cyanosis (bluish tint of the skin and mucous membranes due to insufficient oxygen supply to the blood). However, in babies with normal skin color, heart defects cannot be ruled out. It should be noted that clinical manifestations of this pathology may appear later, as a result of changes in the first hours of life.
The external symptoms of CHD and PPS are similar. However, often the first manifestations of heart disease are its complications - atrial fibrillation, acute pulmonary edema or symptoms associated with pulmonary infarction or impaired blood supply to an organ or tissue.
These symptoms arise due to blockage of blood vessels by any particles carried by the blood or lymph flow. Under normal conditions, these particles are naturally absent from the body. The symptoms of infective endocardia appear slightly differently; they are complemented by the degree of activity of the inflammatory process. Symptoms consist of three main syndromes: toxicosis, endocardial damage and thromboembolic complications, accompanied by high fever.
The disease of pericarditis has its own characteristics, it is usually acute. The defining clinical picture is: signs of compression of the cavities of the heart (hypodiastole). They, in turn, lead to stagnation in the venous cava system, edema, hepato- and splepomegaly. One of the common and fairly typical symptoms is pain. It is characterized by persistence; in young children it is often localized in the abdominal area and is accompanied by flatulence.
Signs of heart defects in children
Signs of heart defects in children usually appear only during physical activity, when one can notice rapid fatigue, shortness of breath, severe tachycardia; as the pathology progresses, the feeling of lack of air occurs more and more often, in connection with performing the simplest actions, for example, when getting dressed. Complaints of general fatigue, weakness, pain in the heart, cough, dizziness and headaches, swelling of the veins in the neck and a tendency to swelling.
A sharp increase in pain when changing body position or deep breathing can be considered quite typical. In older children, the localization of the pain syndrome is more typical—pain in the chest, radiating to the left shoulder and neck.
In infants, one of the signs is difficulty breastfeeding: after 1-2 minutes the child refuses the breast, becomes restless, severe shortness of breath appears, and sometimes cyanosis of the face, hands, and feet. Another obvious sign will be impaired growth and development.
Treatment of heart defects in children
There can be two types of treatment for heart defects in children - surgical and therapeutic, both for congenital and acquired heart defects.
The main direction of therapy for all forms is the fight against heart failure. If an immunological mechanism is present, anti-inflammatory therapy, mainly non-hormonal drugs, may be recommended. For vascular lesions, drugs that improve microcirculation are used.
During the recovery period, cardiotrophic drugs may be recommended. Antibiotics (penicillin drugs) are used for bacterial lesions, in particular for post-streptococcal myocarditis. In parallel, therapy for the underlying disease is carried out. For infectious pericarditis, the main treatment is massive and long-term antibiotic therapy.
Indications for surgical correction of the defect are: 1) the appearance of shortness of breath and signs of heart failure during physical activity; 2) increasing signs of hypertrophy and overload of the heart; 3) increase in pressure in the right - left ventricle. Surgical treatment is optimally performed in children of early school age, and for emergency indications - at any age. Because sometimes early surgical correction of a defect is the only way to save the patient.
Moms and dads should know that heart disease is a serious disease that requires the most careful attention. Therefore, you should not trust unverified clinics, and even more so, you should not turn to unconventional methods of treatment.
Many parents are afraid of operations, trying to avoid them by any means, not realizing that sometimes this is the only possible way to cure. Parents should not be afraid of this, they should talk with specialists several times - understand everything well, become obligatory participants in the child’s healing process, objectively know the situation and how the child will need to be managed after the operation. This is a serious test for the whole family, but not all operations are as dangerous as they seem. In heart surgery, there are a number of operations for which the mortality rate is zero. And this is the merit of our doctors.
And as soon as the diagnosis of heart disease is removed, almost all paths are open to children. The most important thing is to diagnose the disease in time and contact specialists, because 97% of former patients live a full life after surgery.
Treatment methods
Treatment of congenital heart disease is carried out only by surgery . Cardiac surgeons perform complex reconstructive interventions, successfully curing those forms of congenital heart disease that were previously considered inoperable. If the diagnosis is made early and treatment is carried out promptly, heart function can be restored to 100%.
Non-invasive therapy (medication, physiotherapy, etc.) may be prescribed as an auxiliary measure. Such treatment is also carried out in cases where it is possible to postpone the operation to a later time or there is a “white” congenital heart disease that has little impact on the child’s well-being during growth and development.
Narrowing of the pulmonary artery trunk
Pulmonary artery stenosis is a relatively common heart defect in newborns - it is diagnosed in approximately 6-9% of children. This mild heart defect usually causes no symptoms. For this reason, it is usually diagnosed in adolescence or adulthood as a result of shortness of breath and a significant decrease in the body's physical performance. It is important to note that pulmonary artery narrowing does not usually require surgery, only a pulmonary valvuloplasty procedure, which involves widening the valve. A contraindication to this procedure is the occurrence of a dysplastic valve (not fully formed). In this case, it is necessary to perform heart surgery, which involves widening the valve using a special patch.
We invite you to “SM-Clinic”
Our clinic’s staff includes some of the best specialists in the Northern capital. We employ experienced pediatricians and pediatric cardiologists who will promptly identify the presence of alarming symptoms and prescribe all the necessary examinations. “SM-Clinic” is well equipped; we can conduct all tests for the presence of congenital heart disease.
Make an appointment with us as soon as possible if you notice signs of congenital heart disease in your child. Time plays a huge role in this disease.
Sources:
- HER. Chepurnykh, E.G. Grigoriev. Congenital heart defects // Siberian Medical Journal (Irkutsk), 2014, No. 3, pp. 121-127.
- L.N. Falyush, V.V. Florensov. Risk factors for congenital heart defects // Clinical medicine. Bulletin of the All-Russian Scientific Center SB RAMS, 2010, No. 6(76), p.67-69.
- J. I. Hoffman, S. Kaplan. The incidence of congenital heart disease // JACC, 2002, Vol. 39, p.1890—1900.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Steep route
According to accepted standards, the expectant mother should undergo a second ultrasound screening at 16–20 weeks of pregnancy. From this time on, it is already possible to identify congenital heart defects and other developmental defects in the fetus. If something happens, completing this important study will help develop the optimal route for the treatment of a tiny patient.
If any suspicions arise, the pregnant woman will be sent to a specialized hospital, where there is not only precision equipment, but also highly qualified doctors. A council of specialists will decide what to do next: whether to recommend that the woman terminate the pregnancy (after all, part of the congenital heart disease, unfortunately, is incompatible with life or is accompanied by severe mental retardation) or wait for childbirth and plan an operation (emergency or delayed) for the baby.
Those defects that could not be detected at the second screening are most often detected at the third (at 30–32 weeks). By the way, the method of delivery is also chosen by specialists.
Article on the topic
Heart disease is not a death sentence. How children with cardiac pathologies are now saved
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a cardiologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Electrocardiography (ECG) | 1400 rub. |
| Echocardiography (ultrasound of the heart) | 3500 rub. |