Edited by: Kirgizov K.I., Deputy Director (Research Institute of Early Childhood Education, Federal State Budgetary Institution "N.N. Blokhin National Medical Research Center of Oncology" of the Ministry of Health of Russia) for scientific and educational work, pediatric oncologist, leading researcher, Ph.D. .
Childhood leukemia is a malignant disease of the blood system. One of the features of leukemia is that its manifestations at the initial stage can be mistaken for signs of other diseases. Today we will talk about how leukemia manifests itself in children, how to recognize it by the first symptoms and which specialists to contact so as not to waste precious time.
SIGNS OF LEUKEMIA IN CHILDREN
The main symptoms of childhood leukemia include:
- frequent ailments;
- increased fatigue;
- weakness;
- heat (fever);
- frequent bleeding from the mucous membranes and “causeless” (easily occurring) hematomas;
- swollen lymph nodes;
- pain in bones and joints;
- unexplained pale skin.
Below we will look in detail at how certain symptoms manifest themselves at different stages of the disease and what you need to pay special attention to if you suspect leukemia in a child.
SYMPTOMS OF LEUKEMIA IN CHILDREN IN THE INITIAL STAGE
The most common form of childhood leukemia is acute leukemia, which tends to spread very quickly throughout the body. The first signs of leukemia in children can appear within just a few weeks. How does leukemia begin? It has the following manifestations:
- lethargy and pallor (anemic state);
- refusal of usual games and activities;
- feeling of constant fatigue, complaints of lack of strength.
The first symptoms of the disease in children are associated with the fact that cancer cells begin to multiply almost unhindered in the bone marrow, “displacing” normal blood cells and preventing the body from reproducing them in the required quantity. Because of this, the number of normal cells in the blood decreases.
DEVELOPMENT OF LEUKEMIA AND SIGNS OF LATE STAGES
It becomes difficult for the body to fight harmful microorganisms and pathogens. Because of this, the child becomes more susceptible to various infections, often with high fever and acute loss of strength. In addition, a reduced number of platelets, which are responsible for blood clotting, can lead to pinpoint hemorrhages (hematomas) and bleeding of the mucous membranes. As leukemia cells begin to fill not only the bone marrow, but also other organs and tissues, other signs of leukemia appear in the body of children: pain in the arms and legs, in the abdominal area, blurred vision, vomiting, nausea.
The first signs of leukemia in adults and children
Leukemia is a blood disease characterized by disruption of normal hematopoiesis. The disease belongs to a malignant pathology. A pediatric hematologist-oncologist treats leukemia in a child. The true causes of the disease are still unknown. However, doctors identify a number of provoking factors, among which the main ones are:
- radiation exposure;
- high doses of chemotherapy (secondary leukemia);
- chromosomal disorders;
- immunodeficiency states;
- blood diseases;
- Down syndrome, Klinefelter syndrome.
The main causes of chronic leukemia in women are heredity and exposure to various mutagenic factors.
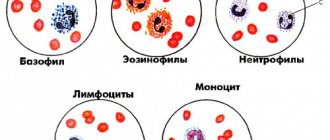
TYPES OF CHILDHOOD LEUKEMIA: HOW ARE THEY DIFFERENT
Leukemia in children and adolescents is known under different names: “leukemia”, “leukemia”, “blood cancer”. However, experts operate in completely different terms, designed to divide the types of childhood leukemia by cell type and their maturity. In general, leukemia is a group of hematological diseases that are characterized by excessive proliferation of leukemic cells and displacement of normal blood cells. Leukemias are divided into acute and chronic, and depending on the predominant cell type involved.
ACUTE LYMPHOBLASTIC LEUKEMIA
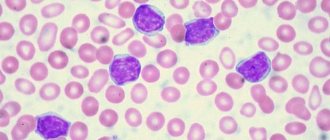
Acute lymphoblastic leukemia (ALL) accounts for about 25% of all malignant tumors in children and adolescents under 18 years of age and is the most common childhood cancer. Lymphoid forms of acute leukemia account for 80–90% of childhood leukemia. In ALL, the maturation process of lymphocytes - white blood cells, which are responsible for fighting infections and providing protection to the body - is disrupted. The immaturity of white blood cells (blasts), their replacement of normal blood cells, leads to the appearance of symptoms of ALL in children: frequent infections, problems with blood clotting, and an anemic appearance.
ACUTE MYELOID LEUKEMIA
Acute myeloid leukemia (AML) is the second most common childhood leukemia after ALL, accounting for 20% of all acute childhood leukemias and 6% of all childhood tumors. It affects blood cells called myeloid stem cells. Normally, these cells form mature blood cells: red blood cells, granulocytes and platelets. However, in AML this process is disrupted and large numbers of immature white blood cells cause the above symptoms.
On the left is healthy bone marrow, on the right is the bone marrow of a child with AML.
JUVENILE MYELOMONOCYTIC LEUKEMIA
Juvenile myelomonocytic leukemia (JMML) is one of the rarest forms of leukemia, occurring exclusively in young children. On average, this diagnosis is made before the child reaches the age of 2 years. JMML differs from CML in that its leukemia cells do not have the Philadelphia chromosome (but other chromosomal abnormalities are often present). In addition, JMML is associated not only with impaired hematopoietic processes, but also with increased production of monocytes.
CHRONIC MYELOID LEUKEMIA
Chronic myeloid leukemia (CML) occurs very rarely in children, accounting for about 3–5% of all cases of childhood leukemia. However, the vast majority of children with CML have a genetic mutation called the “Philadelphia chromosome.” Being a chronic form of leukemia, CML develops over a fairly long period of time. Unlike acute leukemia, where weeks count, with CML it can take months before the first symptoms appear.
Prevalence of different types of leukemia.
Classification of the disease
According to the course, acute and chronic forms of the disease are distinguished.
Spicy. The disease develops very quickly and tends to progress. The fight against acute leukemia is significantly different from the treatment of chronic leukemia.
Chronic. The disease is less aggressive and is often detected during diagnosis for another pathology. The chronic form is characterized by alternating periods of remission and exacerbation.
On our website Dobrobut.com you can sign up for a consultation with a specialist and learn about leukemia, what kind of disease it is, and its causes. At the clinic you can undergo a full examination of the body, including laboratory and instrumental studies.
DIAGNOSIS OF LEUKEMIA IN CHILDREN
As a rule, from the moment the first symptoms of leukemia appear in children and adolescents until medical confirmation of the diagnosis takes from several weeks to several months1. Therefore, as soon as you notice any symptoms in your child, it is very important to consult a doctor as soon as possible. You can diagnose acute or chronic leukemia and determine its exact type using the following tests:
- General examination, assessment of the patient’s physical condition and medical history.
- General detailed blood test with mandatory differentiated leukocyte count (leukocyte formula).
- Bone marrow puncture followed by cytological and cytochemical examination.
- Lumbar puncture with cerebrospinal fluid examination.
- X-ray, ultrasound and other instrumental diagnostic methods.
If necessary, specialists can prescribe other tests and procedures - in particular, high-tech studies for specific markers and parameters of tumor cells.
Diagnostics
To confirm such a formidable pathology, the doctor will prescribe the following studies:
- general blood analysis;
- blood chemistry;
- bone marrow biopsy;
- X-ray examination;
- computed tomography.
A blood test for leukemia is of decisive importance.
It is important to differentiate leukemia from autoimmune thrombocytopenic purpura, juvenile rheumatoid arthritis, neuroblastoma and infectious mononucleosis.
TREATMENT AND PREVENTION OF LEUKEMIA
Treatment of leukemia is a voluminous, high-tech and continuously improving area of medicine. Currently, there are many methods for treating leukemia in children, these include: chemotherapy (the main method);
- targeted therapy;
- bone marrow or stem cell transplantation;
- immunotherapy;
- radiation therapy.
The most optimal treatment method is individually prescribed by a pediatric oncologist, who will select a therapy protocol to achieve maximum results. Treatment is carried out in a hospital in accordance with clinical recommendations.
Causes
The causes of oncological blood diseases have not been precisely established. It could be:
- genetic failure;
- abnormal development of blood cells;
- exposure to radiation;
- hereditary factor;
- poor environmental stop;
- consumption of carcinogens, etc.
Even a medical luminary is unlikely to be able to say exactly why a child, who does not yet have negative habits and does not eat harmful foods, develop an illness.
PROGNOSIS FOR LEUKEMIA IN CHILDREN
Fortunately, the two most common forms of childhood leukemia—ALL and AML—have fairly good prognoses for survival and durable remission. Modern treatment protocols are successful in 80–90% of children with leukemia—and with fewer complications than previous regimens10. In both cases, patients are considered recovered after approximately 5 years of stable remission, but they should continue follow-up with an oncologist and/or hematologist. If, after the first courses of treatment, doctors diagnose a resistant form (i.e., not responding to treatment), or a relapse of leukemia occurs, further treatment options are selected taking into account all the parameters and available medical capabilities. The main thing to remember when faced with leukemia is that modern medicine and self-confidence sometimes really work miracles! Treatment of leukemia is becoming more and more high-tech, and prognoses for treatment and remission today are much more optimistic than they were in the recent past.
There is even more information about leukemia in children on the information portal from the Zhivi charity foundation infoleikoz.ru.
Prevention
As such, there is no prevention of the occurrence of the disease. It is recommended to adhere to a properly balanced diet, walk more in the fresh air, avoid gas pollution, exposure to radiation, etc.
Dear parents!
Remember that only a qualified pediatrician can make an accurate diagnosis, determine the causes and nature of the disease, and prescribe effective treatment. You can make an appointment with our specialists or call a doctor at home by calling 8-800-700-31-69 Grow up healthy and happy!
LIST OF REFERENCES USED
1. Clinical guidelines of the Ministry of Health of the Russian Federation “Acute lymphoblastic leukemia”, 2021. 2. Bernbeck B., Wüller D., Janssen G., Wessalowski R., Göbel U., Schneider DT Symptoms of childhood acute lymphoblastic leukemia: red flags to recognize leukemia in daily practice. Klin Padiatr. Nov-Dec 2009;221(6):369–73. doi: 10.1055/s-0029-1239538. Epub 2009 Nov 4. PMID: 19890789 (https://pubmed.ncbi.nlm.nih.gov/19890789/). 3. Lyengar V., Shimanovsky A. Leukemia. StatPearls. Publishing LLC 2020. PMID: 32809325 (https://www.ncbi.nlm.nih.gov/books/NBK560490/). 4. Sokolova T.A., Kotlovsky Yu.V., Dubynina E.V., Ivanovskaya O.V., Veselova V.K., Kuznetsova E.Yu. Cytogenetic diagnostics for oncohematological diseases. Academy of Natural Sciences, 2012. ISBN: 978-5-91327-211-9. 5. Clinical guidelines of the Ministry of Health of the Russian Federation “Acute myeloid leukemia”, 2020. 6. Lee JW, Chung NG The treatment of pediatric chronic myelogenous leukemia in the imatinib era. Korean J Pediatr 2011 Mar;54(3):111–6. doi: 10.3345/kjp.2011.54.3.111. PMID: 21738540 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3120996/). 7. Dvorak CC, Loh ML Juvenile Myelomonocytic Leukemia: Molecular Pathogenesis Informs Current Approaches to Therapy and Hematopoietic Cell Transplantation. Front Pediatr. 2014;2:25. doi: 10.3389/fped.2014.00025. PMID: 24734223 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975112/). 8. Davis AS, Viera AJ, Mead MD Leukemia: an overview for primary care. Am Fam Physician. 2014 May 1;89(9):731–8. PMID: 24784336 (https://pubmed.ncbi.nlm.nih.gov/24784336/). 9. National Cancer Institute, Advances in Leukemia Research, May 29, 2020 (https://www.cancer.gov/types/leukemia/research). 10. Whitehead TP, Metayer C, Wiemels JL, Singer AW, Miller MD Childhood Leukemia and Primary Prevention. Curr Probl Pediatr Adolesc Health Care. 2021 Oct;46(10):317–52. doi: 10.1016/j.cppeds.2016.08.004. PMID: 27968954 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5161115/).
La Fondation La Roche-Posay and CCI (Childhood Cancer International) make every effort to ensure that the information provided is accurate and current at the time of publication. We are not responsible for information provided by third parties, incl. those that we refer to or highlight in this publication. The information in this publication should be used to supplement appropriate professional advice in your particular circumstances.
Acute myeloid leukemia status after treatment
The long-term prognosis of each patient largely depends on how well and quickly the disease responds to treatment: the better the body’s first reaction, the more optimistic the prospects.
Remission - no signs of leukemia: the bone marrow contains less than 5% blasts. Blasts are rapidly growing immature, non-functioning white blood cells. , and the number of blood cells is within normal limits. Complete molecular remission means that doctors were unable to detect the altered cells even with very sensitive tests.
Minimal residual disease , MRD: This term is used when, after treatment, abnormal cells are not detected by conventional methods - for example, by standard examination of samples under a microscope, but are detected by modern accurate examinations.
Active disease: after treatment there are more than 5% blasts in the bone marrow, or after therapy a relapse occurred - the disease returned.